1st #NIHRECOVER adult cohort results are out today in @JAMA_current, proposing an expanded working definition of #LongCovid (aka post-acute sequelae of SARS-CoV-2 [PASC]). Led by @tthaweethai, this is a dense paper with a ton of results. Buckle up! 🧵
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…
#NIHRECOVER Adult is a cohort study of ~15k adults with/without #COVID, followed prospectively. They answer symptom surveys every 3 months and do additional tests yearly. 93% of cohort has been enrolled; this paper includes 9,764 participants. recovercovid.org
Main goal of this paper is to establish an expanded, working symptom-based definition of #LongCOVID for research purposes. Please note we do not propose this as a clinical definition right now pending further validation & refinement.
Methods: we studied symptoms reported 6 months or later (for those who enroll >6 months after infection) after infection. Main analysis uses all symptoms, whether present pre-COVID or not. Sensitivity analysis used just new symptoms.
Methods: symptom survey has 44 symptoms. We included 37 with frequency >2.5% in cohort, restricting to >=moderate severity where possible. We used balancing weights (by age/sex/race/ethnicity) to match uninfected and infected participants.
First, we assessed each symptom to see which were more common in infected vs uninfected participants. Result: all of them! But some much more than others. Note also that some common symptoms have lower OR because also common in uninfected (e.g. fatigue, 38% vs. 17%). 

Most studies stop here. But these symptoms, while more common in infected, happen in uninfected too. So just having a symptom is not enough for a reliable research definition. We decided to look for a SET of symptoms that collectively would be rare to find in uninfected.
We fit a LASSO model using 10-fold cross-validation and class weighting, with the 37 symptoms as predictors, infection as outcome. That method helps us select symptoms that best distinguish between infected/uninfected, and it got us down to just 12 symptoms.
📷
📷
IMPORTANT: these are not the ONLY symptoms that people have, nor are they necessarily the most important to patients, the most common, the most severe or most burdensome. They are just the symptoms that are the most useful in trying to decide who might have #LongCOVID.
Then, we took the coefficients of this model, multiplied each by 10 and rounded them to turn each coefficient into nice, tidy integer points. For each participant, we added up all their points to generate a total score. 

Now, the tricky part. What total score is reasonable to call #LongCOVID? There is no “right” answer. We used 10-fold cross-validation to identify an optimal threshold that minimized misclassification of uninfected while capturing infected.
Our optimal threshold was score of 12. At this cutoff, only 4% of uninfected are misclassified as having #LongCOVID. (Note, it is also possible that some of our “uninfected” had occult infection; we check antibodies but those do wane.) 

For some face validity, we noted that the higher the score, the worse the quality of life, general physical health, and ability to carry out everyday physical activities: as expected. 

Now, we are cooking with gas. With #LongCOVID definition in hand, we could take a quick, early look at interesting questions that we will revisit later with more rigor.
For instance, what is prevalence of #LongCOVID? We find it to be 10% @6 months in “acutes” enrolled <30 days from infection (least biased – enrolled prior to knowing if they have #LongCOVID). Note, they all had Omicron and are almost all vaccinated.
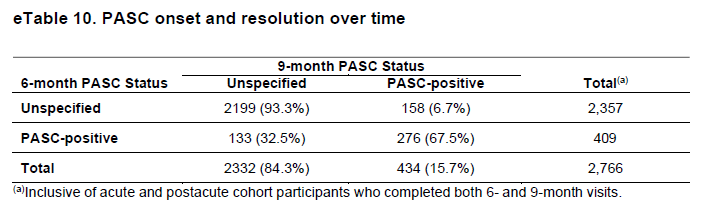
What is recovery like? 1/3 of people who met #LongCOVID definition at 6 months no longer met it at 9 months; not likely just random variation around threshold because reverse is only 7% (no at 6 mo/yes at 9 mo). 
Does vaccination reduce risk? At first glance, yes. We didn't do a formal analysis; that will come in future. 

Is #LongCOVID a collection of different syndromes? We did a cluster analysis and found 4 clusters that had some differences but not dramatically different profiles. BUT, score requires symptoms in multiple domains, so this could be artifact of definition. 

Want to participate in generating more science like this? We have reserved the last few slots in the adult cohort for people living in rural areas or who identify as Hispanic. If you meet these criteria and are interested, check out recovercovid.org to volunteer.
#NIHRECOVER is an extraordinary collaborative effort; tagging authors I know are on twitter; there are many others! @SE_Jolley @LevitanEmily @LisaAMcCorkell @girish_nadkarni @sai_sparthamd @galbamd @hashktorab @LBatemanMD @shamik_b @Blomkalns @HelenChuMD @SushmaCribbs @kerlands
@NerdmannID @ernstkc @JC_Gander @rhessmd @SLHWV @brennahughesmd @prasannaj77 @DrJohnKirwan @JerryKrishnan @jleeiannotti @JHMaley @vmarconi12 @MetzTorri @jarrodmosier @ChrisMouchati @Ighid
@vmarconi2 @PalatnikAnna @ParimonTanyalak @RachelPatzerPhD @MichaelPelusoMD @DrPemuH360x @cmpettker @kpb_Epi @athenapoppas @rebecca_reece3 @harrison_reeder @JRosand_MD @DanielSkupskiMD @jeffsparks @DrBarbaraTaylor
@atitapatterns @A_E_Urdaneta @zach_wallace_md; & a ton of non-Twitter authors including senior author Andrea Foulkes. If you have a common name and I couldn't find you feel free to add yourself!
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter





