Interesting case, what is the most likely diagnosis in this 25 y/o F w/ 1 year history of migraine headaches, left hand numbness, and b/l retinal artery occlusions? 🧠 👁️
#Ophthalmology #neurology #neurosurgery #neurotwitter #MedEd @TheASNR #MedTwitter



#Ophthalmology #neurology #neurosurgery #neurotwitter #MedEd @TheASNR #MedTwitter



Answer: Susac syndrome 🧠
▶️Susac syndrome is a microangiopathy (likely autoimmune affecting the precapillary arterioles) with a strong female predilection, typically occurring in women age 20-40
▶️Susac syndrome is a microangiopathy (likely autoimmune affecting the precapillary arterioles) with a strong female predilection, typically occurring in women age 20-40
Clinical presentation:
Classic triad
1️⃣Encephalopathy
2️⃣Branch retinal artery occlusions
3️⃣Hearing loss
💡Though most patients do not present with the complete triad (it may develop over years)
Classic triad
1️⃣Encephalopathy
2️⃣Branch retinal artery occlusions
3️⃣Hearing loss
💡Though most patients do not present with the complete triad (it may develop over years)
Imaging:
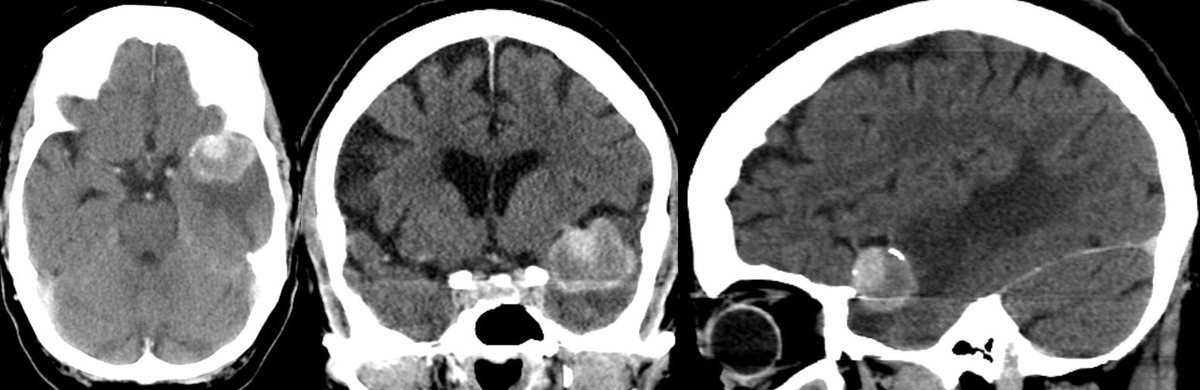
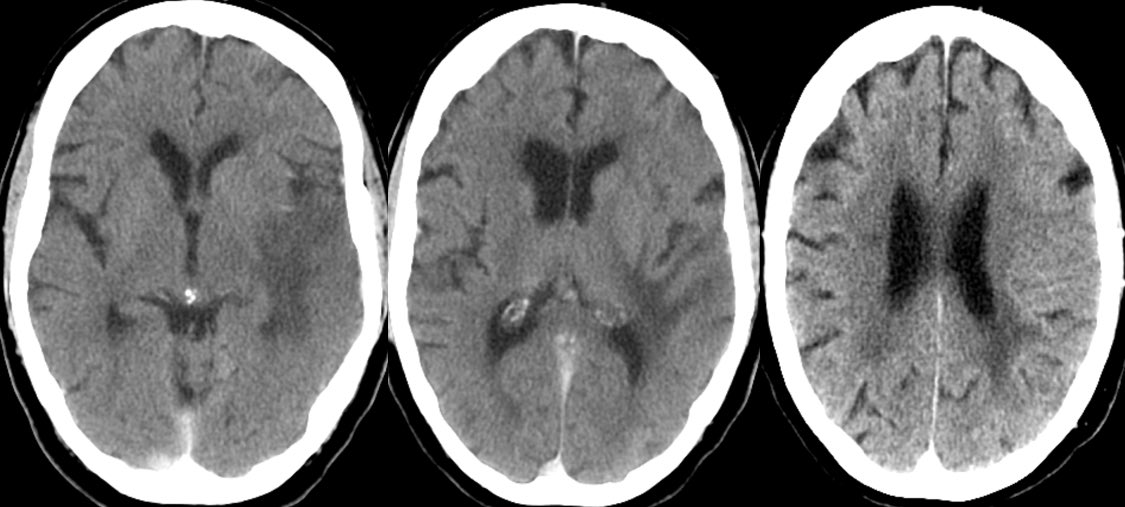
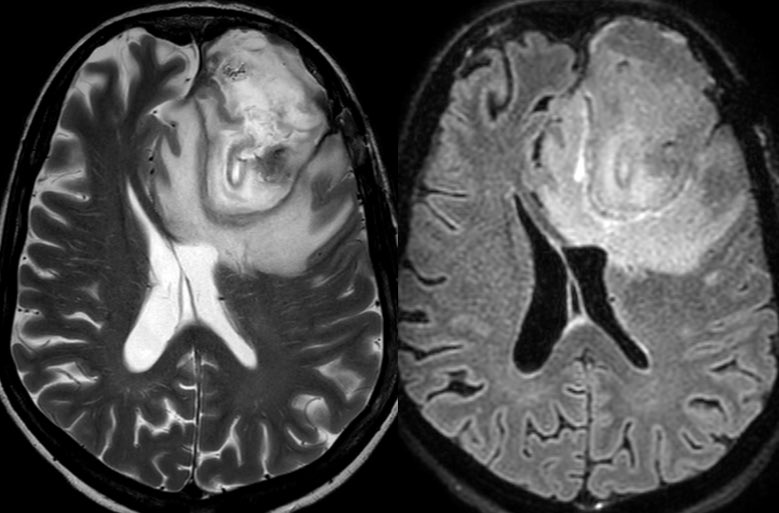
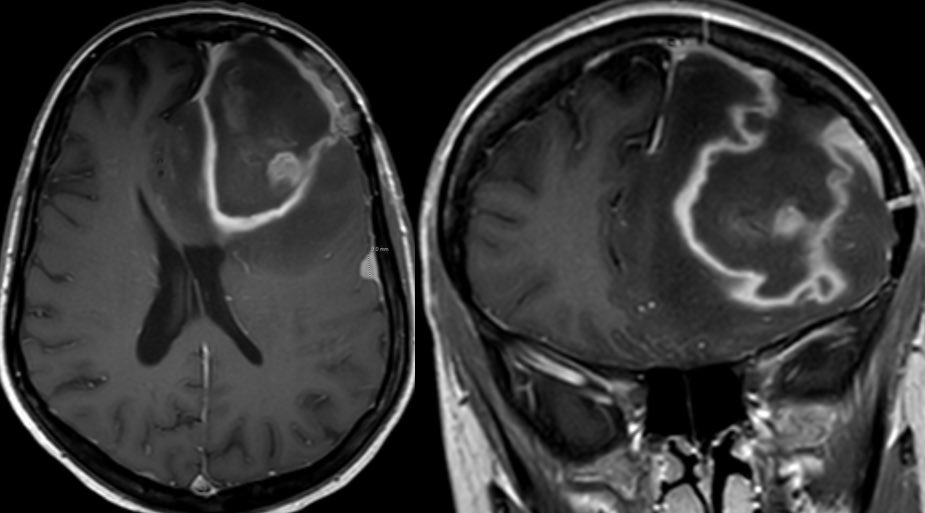
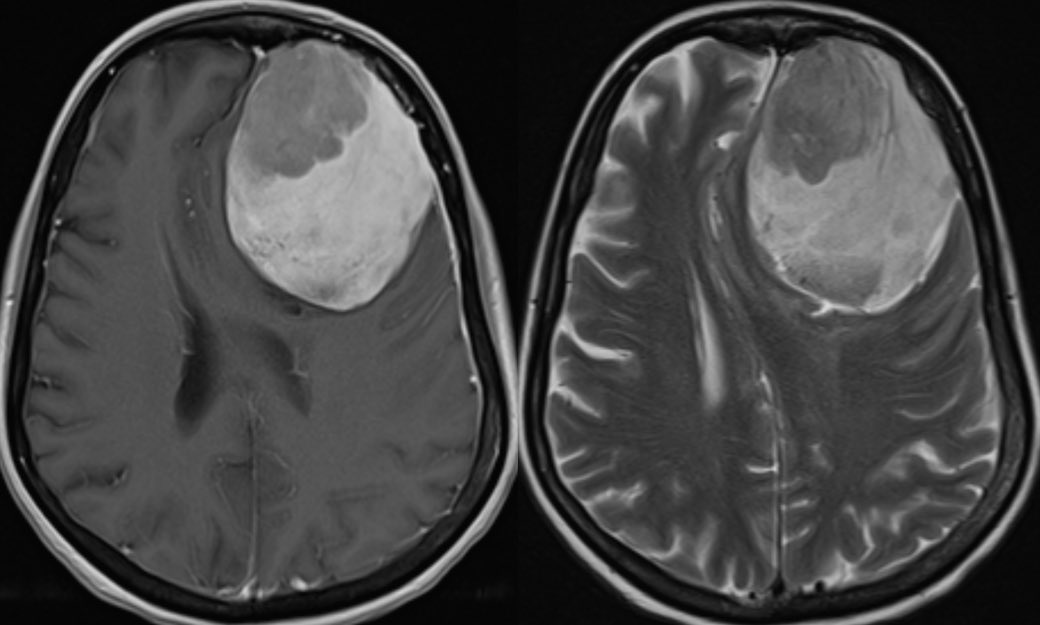
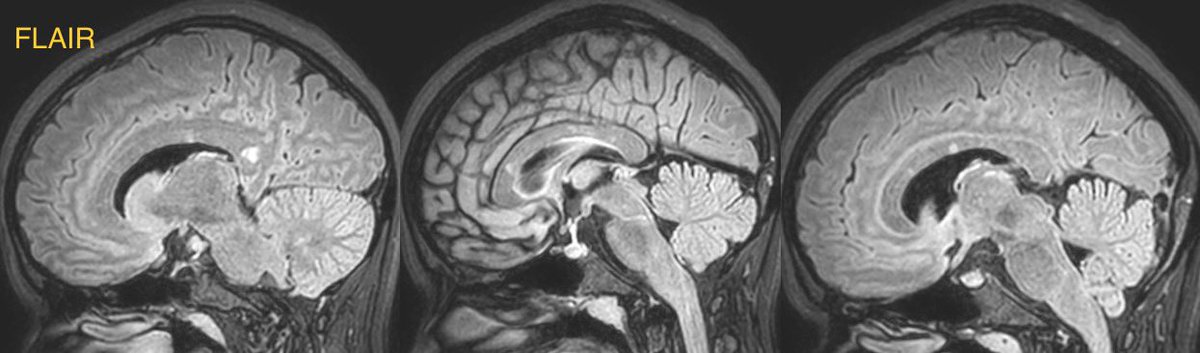
▶️T2/FLAIR: Similar to lesions seen in multiple sclerosis but with more ROUNDED MORPHOLOGY and a predilection for the MIDDLE LAYERS of the corpus callosum (rather than the callososeptal interface seen in MS)
▶️T2/FLAIR: Similar to lesions seen in multiple sclerosis but with more ROUNDED MORPHOLOGY and a predilection for the MIDDLE LAYERS of the corpus callosum (rather than the callososeptal interface seen in MS)

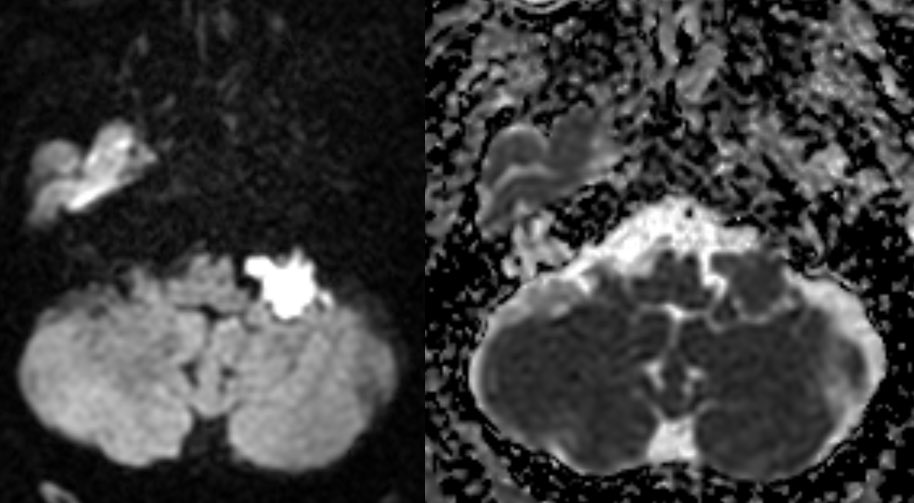
▶️DWI/ADC: May see true restricted diffusion due to microinfarcts (case shows an example in the splenium)
▶️T1C+: Variable but often has leptomeningeal enhancement (as seen in the cerebellar folia in this case)

▶️T1C+: Variable but often has leptomeningeal enhancement (as seen in the cerebellar folia in this case)


Learning points:
💡 Consider this diagnosis in patients with the classic clinical triad, especially if lesions of the corpus callosum are present
1️⃣Encephalopathy
2️⃣Branch retinal artery occlusions
3️⃣Hearing loss
💡 Consider this diagnosis in patients with the classic clinical triad, especially if lesions of the corpus callosum are present
1️⃣Encephalopathy
2️⃣Branch retinal artery occlusions
3️⃣Hearing loss
💡 Rounded morphology of lesions and predilection for the middle layers of the CC may help suggest the diagnosis in the appropriate setting
💡 Though beware, imaging often mimics vasculitis or the much more common MS, so clinical context is 🔑
ajnr.org/content/25/3/3…
💡 Though beware, imaging often mimics vasculitis or the much more common MS, so clinical context is 🔑
ajnr.org/content/25/3/3…
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter