Differential Diagnosis for cortically based masses
P-DOG 🐶
1️⃣Pleomorphic Xanthoastrocytoma (PXA)
2️⃣Dysembryoplastic neuroepithelial tumor (DNET)
3️⃣Oligodendroglioma
4️⃣Ganglioglioma
#Neurology #neurosurgery #peds #radres #neurotwitter @The_ASPNR @TheASNR #MedTwitter



P-DOG 🐶
1️⃣Pleomorphic Xanthoastrocytoma (PXA)
2️⃣Dysembryoplastic neuroepithelial tumor (DNET)
3️⃣Oligodendroglioma
4️⃣Ganglioglioma
#Neurology #neurosurgery #peds #radres #neurotwitter @The_ASPNR @TheASNR #MedTwitter



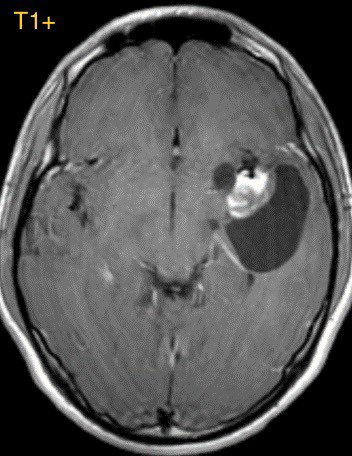
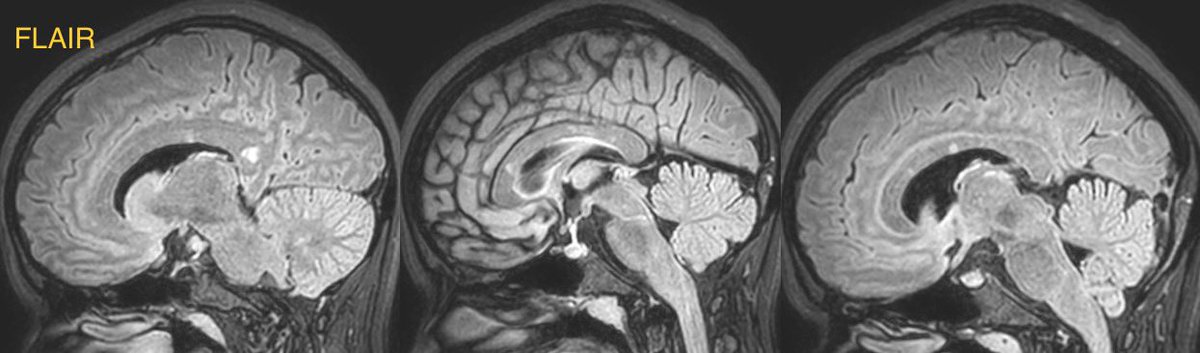
1️⃣PXA
Originate in the subpial astrocytes typically in children and young adults often with a seizure history
Temporal lobe is most common
Originate in the subpial astrocytes typically in children and young adults often with a seizure history
Temporal lobe is most common
Imaging (variable):
▶️Classically appear as a cortically based mass with cyst and enhancing nodule and overlying DURAL TAIL or enhancing leptomeninges
▶️Calcifications are RARE

▶️Classically appear as a cortically based mass with cyst and enhancing nodule and overlying DURAL TAIL or enhancing leptomeninges
▶️Calcifications are RARE


▶️Can look very similar to ganglioglioma though calcifications are rare in PXA and if you’re lucky enough to have a dural tail/enhancing leptomeninges then PXA is favored
▶️Companion case of another PXA below



▶️Companion case of another PXA below
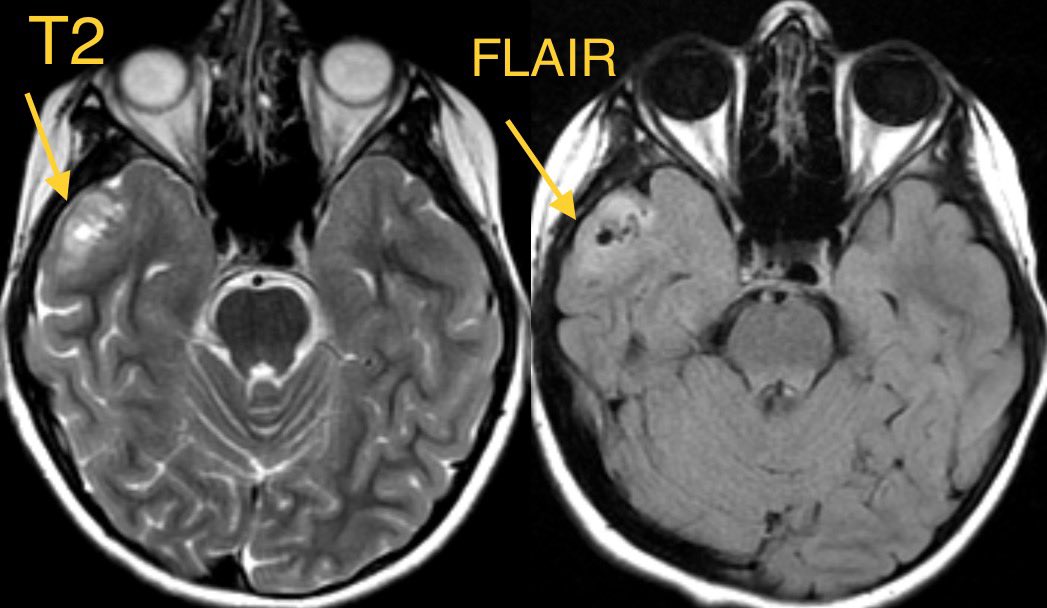



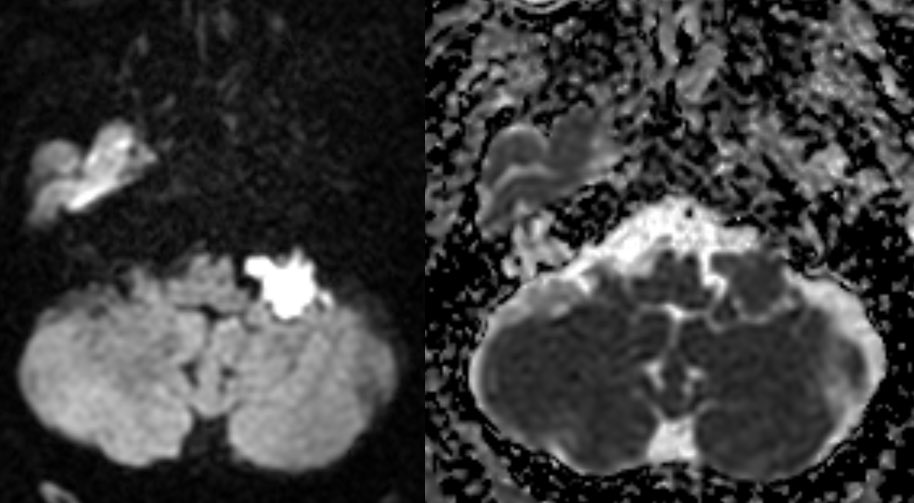
2️⃣DNET
▶️Cortically based mass in children and young adults presenting with long-standing seizures
▶️Most frequently occurs in temporal and frontal lobes
▶️Cortically based mass in children and young adults presenting with long-standing seizures
▶️Most frequently occurs in temporal and frontal lobes
Imaging:
▶️Classically presents as a well demarcated cortically based “BUBBLY” mass with HYPERINTENSE RIM AROUND CYSTS ON FLAIR


▶️Classically presents as a well demarcated cortically based “BUBBLY” mass with HYPERINTENSE RIM AROUND CYSTS ON FLAIR



▶️Usually there is NO ENHANCEMENT (though can have punctate or ring enhancement). However, when enhancement is seen, consider the possibility of more aggressive tumors.
▶️Companion case below of another DNET


▶️Companion case below of another DNET



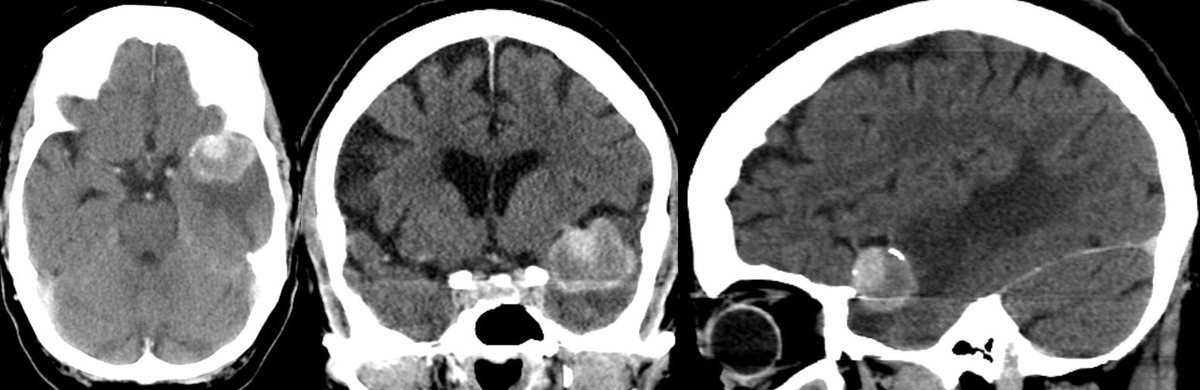
3️⃣Oligodendroglioma
▶️Cortically based mass mainly in ADULTS
▶️Location: FRONTAL and temporal lobes most common
▶️Cortically based mass mainly in ADULTS
▶️Location: FRONTAL and temporal lobes most common
Imaging:
▶️Classically presents as a gyriform cortical/subcortical based mass with GYRIFORM OR CLUMPED CALCIFICATIONS
▶️Consider this diagnosis in an ADULT WITH A CALCIFIED FRONTAL MASS



▶️Classically presents as a gyriform cortical/subcortical based mass with GYRIFORM OR CLUMPED CALCIFICATIONS
▶️Consider this diagnosis in an ADULT WITH A CALCIFIED FRONTAL MASS




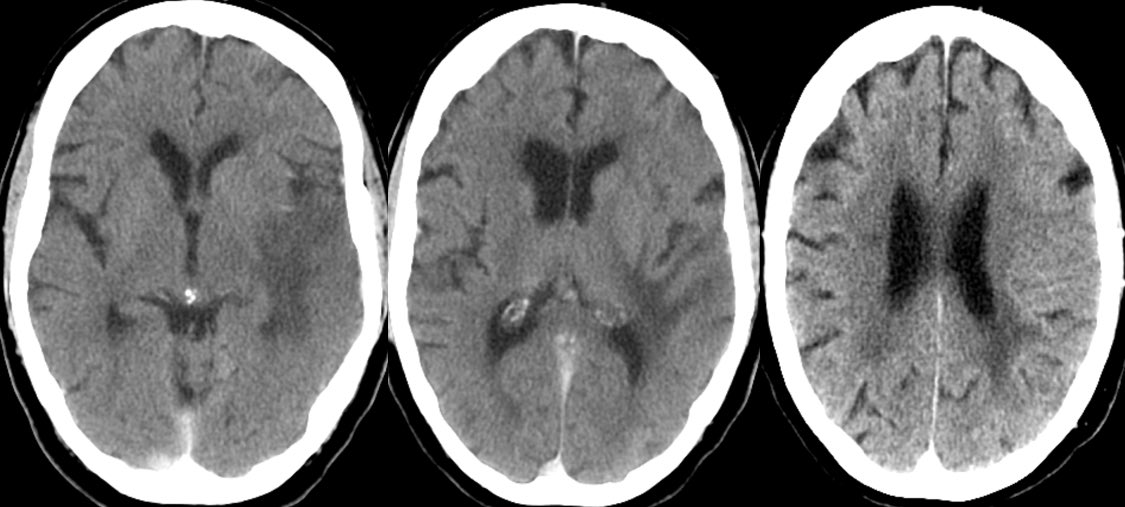
4️⃣Ganglioglioma
▶️Occurs in children and young adults
▶️Location: Temporal lobe (most common)
▶️Occurs in children and young adults
▶️Location: Temporal lobe (most common)
Imaging (variable and can look very similar to PXA):
▶️Classically presents as a cystic and solid mass in the temporal lobe in a child/young adult with seizures
▶️Presence of CALCIFICATIONS & LACK OF DURAL TAIL may help to differentiate from PXA


▶️Classically presents as a cystic and solid mass in the temporal lobe in a child/young adult with seizures
▶️Presence of CALCIFICATIONS & LACK OF DURAL TAIL may help to differentiate from PXA



💡 Learning points/summary:
P-DOG 🐶
1️⃣PXA: Cyst w/ enhancing mural nodule with DURAL TAIL/leptomeningeal enhancement and NO CALCIFICATIONS
2️⃣DNET: BUBBLY well demarcated mass with NO ENHANCEMENT



P-DOG 🐶
1️⃣PXA: Cyst w/ enhancing mural nodule with DURAL TAIL/leptomeningeal enhancement and NO CALCIFICATIONS
2️⃣DNET: BUBBLY well demarcated mass with NO ENHANCEMENT




3️⃣Oligodendroglioma: Gyriform mass in frontal lobe of an ADULT w/ CALCIFICATIONS
4️⃣Ganglioglioma: Cyst w/ enhancing nodule in temporal lobe w/ CALCIFICATIONS and NO DURAL TAIL


4️⃣Ganglioglioma: Cyst w/ enhancing nodule in temporal lobe w/ CALCIFICATIONS and NO DURAL TAIL



• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter