Here, despite younger age at diagnosis, lower prevalence of obesity and diabetes family history, individuals with recently diagnosed type 2 diabetes who had a low birthweight were more likely to have greater use of glucose-lowering medications and a larger burden of comorbidity. 
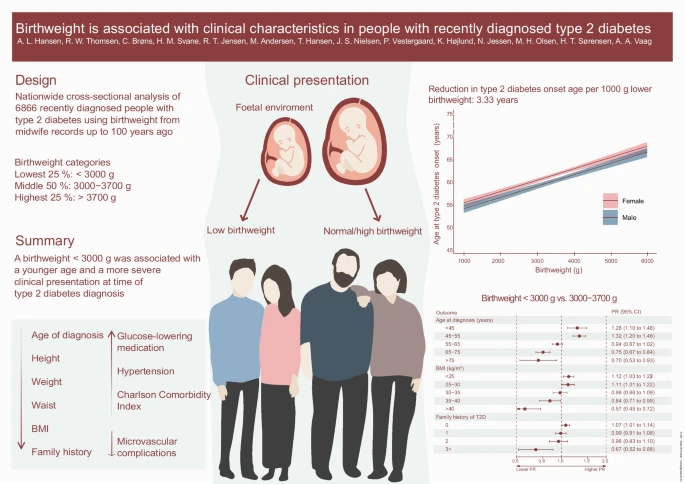
- Low birthweight is a risk factor for type 2 diabetes but it is unknown whether low birthweight is associated with distinct clinical characteristics at disease onset.
- This study examined whether a lower or higher birthweight in type 2 diabetes is associated with clinically relevant characteristics at disease onset.
- Compared with individuals with type 2 diabetes falling within the 50% middle range of birthweight, those within the lowest 25% birthweight (<3000g) were younger at disease onset, had a lower prevalence of obesity, and a greater burden of comorbidity including an SBP ≥155 mmHg.
- These individuals also displayed greater use of glucose-lowering and antihypertensive medications and were less likely to have a diabetes-associated neurological disease at enrolment.
- They were less also likely to report a family history of type 2 diabetes.
- Interestingly, adjustment for currently known genetic predispositions to type 2 diabetes and birthweight did not attenuate the associations.
- Opposite relationships were generally observed for participants with type 2 diabetes who were in the 25% highest compared with lowest birthweight groups.
- Case–control analysis reconfirmed the association between low birthweight and type 2 diabetes risk in the current study population.
Birthweight is associated with clinical characteristics in people with recently diagnosed type 2 diabetes (open access)
doi.org/10.1007/s00125…
#MetabolicSyndrome #Diabetes #nutrition #diet #Women #pregnancy
doi.org/10.1007/s00125…
#MetabolicSyndrome #Diabetes #nutrition #diet #Women #pregnancy
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter









