Glad to see #ME/CFS mentioned as a disease potentially connected to immunometabolic reprogramming of host cells. But #pathogen activity in ME/CFS is severely understudied. For example, no team has yet searched for organisms in patient cerebrospinal fluid
https://twitter.com/ImmunoMet/status/1227565447073206272
2/ Further, numerous outbreaks of the disease have occurred that were directly linked to #enterovirus/coxsackie #viruses + autopsy studies of patients w/ ME/CFS have identified enteroviruses in patient brain tissue + stomach biospy samples: ncbi.nlm.nih.gov/pubmed/17872383
3/ Moreover early studies on #microbiome activity in ME/CFS indicate dysbiosis of #bacterial communities in patients w/ the #disease, w/ one study noting an increase in bacterial phyla in patient blood after a symptom-provocation challenge: ncbi.nlm.nih.gov/pubmed/26683192
4/ Or this team found that the prevalences + median values for serum IgA against the LPS of enterobacteria were significantly greater in patients with ME/CFS than controls: ncbi.nlm.nih.gov/pubmed/17007934
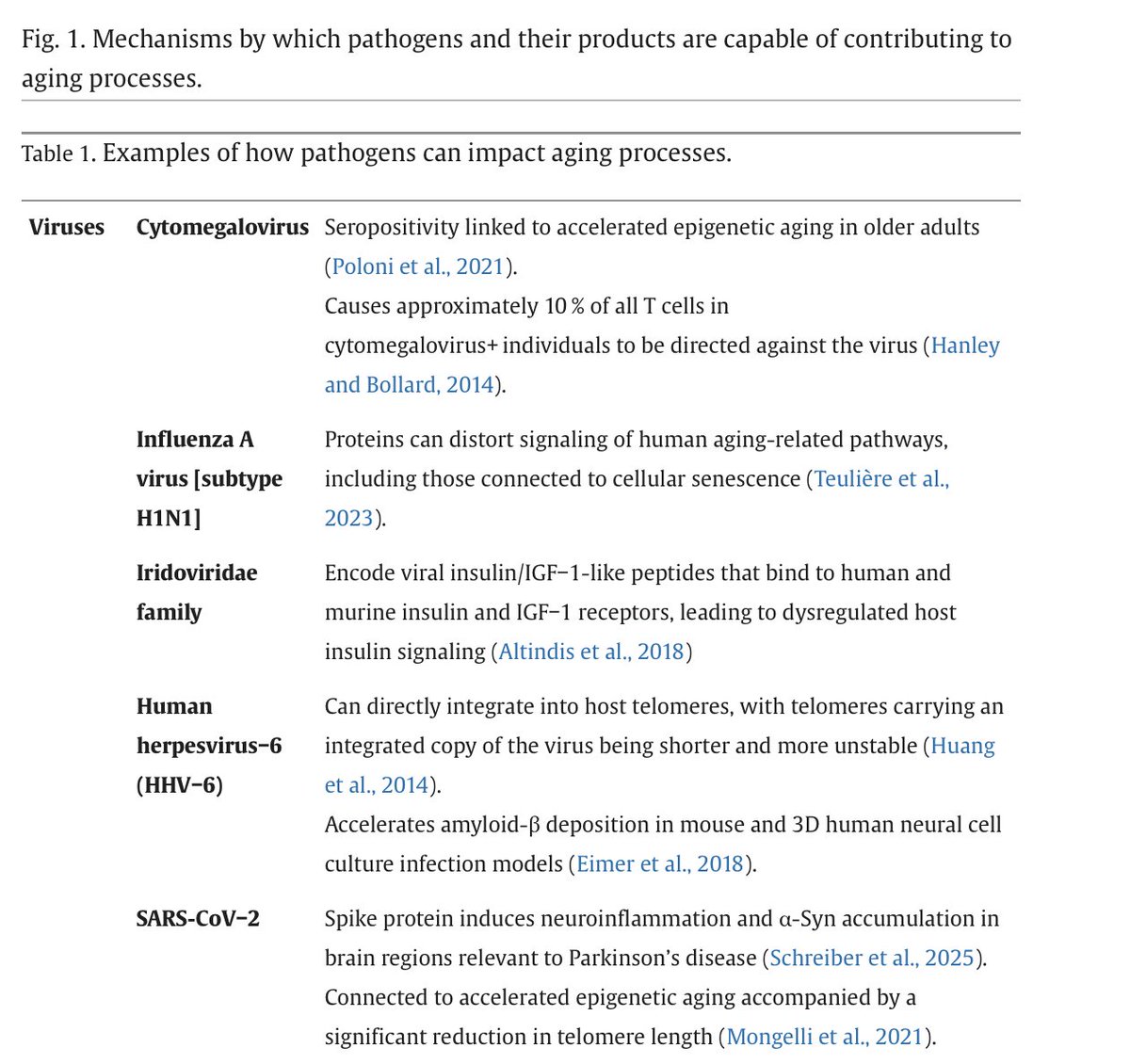
5/ Those and related studies matter greatly, b/c a growing range of intracellular #viruses + #bacteria are capable of driving potential immunometablic (Warburg-associated) changes in immune cells of patients with ME/CFS.
6/ Even #LPS itself has been shown capable of directly inducing a Warburg-like metabolism in host cells (often via activation of TLR4): ncbi.nlm.nih.gov/pubmed/29603622 

7/ The paper I linked to above further discusses how a range of intracellular #bacteria (mycobacteria, chlamydia etc) can reprogram + remodel host cells to Warburg-like #metabolic state. This shift allows them to better create nutrients needed for their survival/replication.
8/ A range of #viruses - EBV, Dengue - etc also shift host cells towards a Warburg metabolism, which provides such viruses w/ increased pools of free nucleotides for rapid replication, viron assembly etc: ncbi.nlm.nih.gov/pubmed/25812764 

9/ That means we must continually study Warburg/immunometabolic reprogramming of host cells in the context of the #organisms/pathogens present in any patients’ microbiome/#virome communities (in all chronic conditions!)
10/ Keep in mind this @BrodinPetter paper which found variation in the human immune system is largely driven by non-heritable influences like pathogens. We must always factor these environmental influences into the "immune" component of "immunometabolism": ncbi.nlm.nih.gov/pubmed/25594173 

• • •
Missing some Tweet in this thread? You can try to
force a refresh