ft.com/content/d738b2…
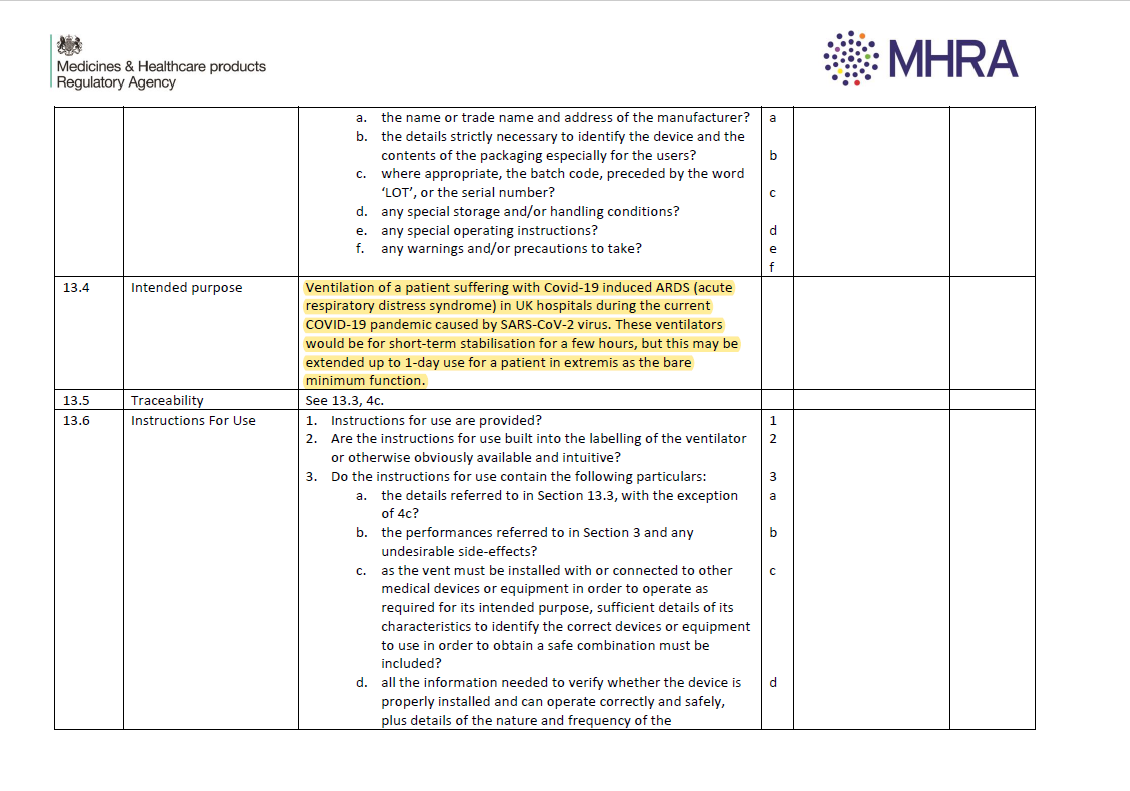
1) it creates a structure/ensures this is not random or on a whim
2) NOTE the 'caveat' - clinical judgment is still key here
3) Docs do this all the time, #COVID19 just foregrounds it /2
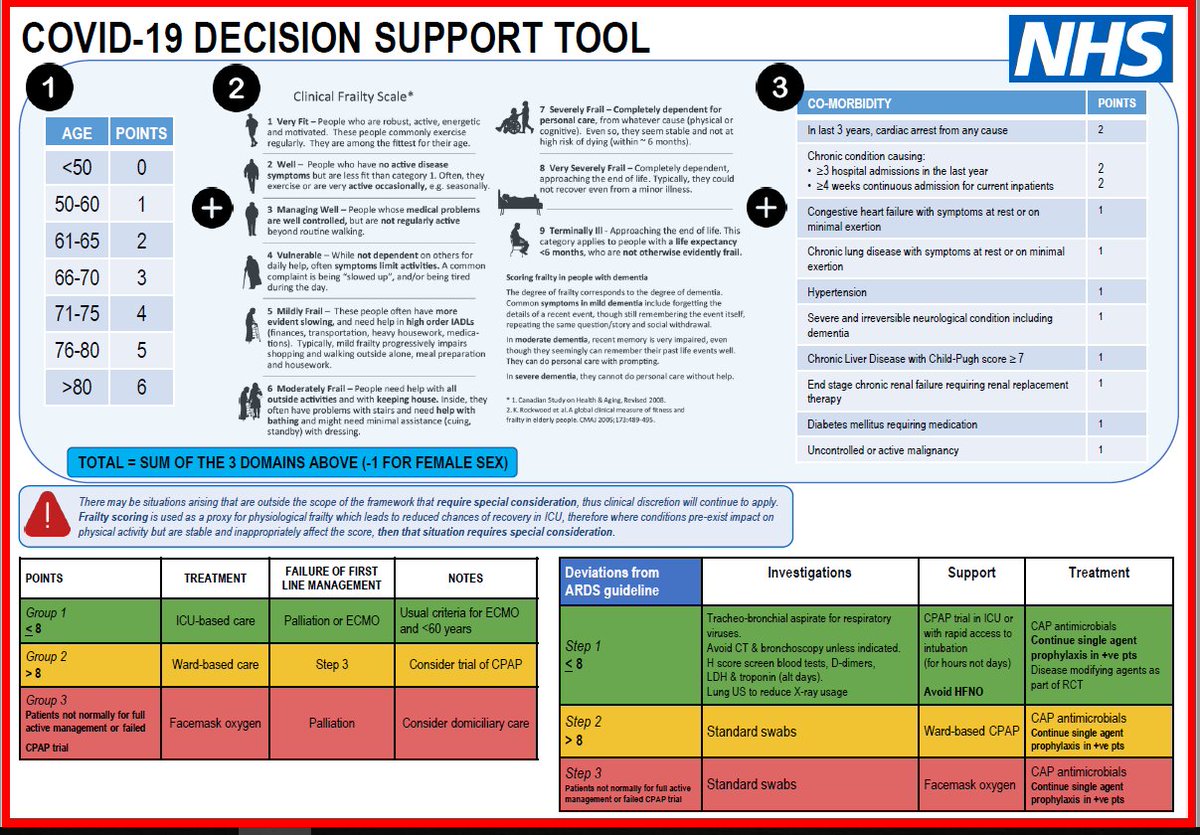
Is a patient that scores >8 and doesn't get sent to ICU/ventilation being triaged that way because of a) lack of resource b) they aren't likely to make it c) better for them medically? /3
BUT, as doc tells me, the thing about #Coronavirus is that there is NO cure. Which means ventilation and organ support, but not like you go to ICU to 'cure' disease /4
It demonstrates how much thought goes into this - the blend of art and science as the doctor says.
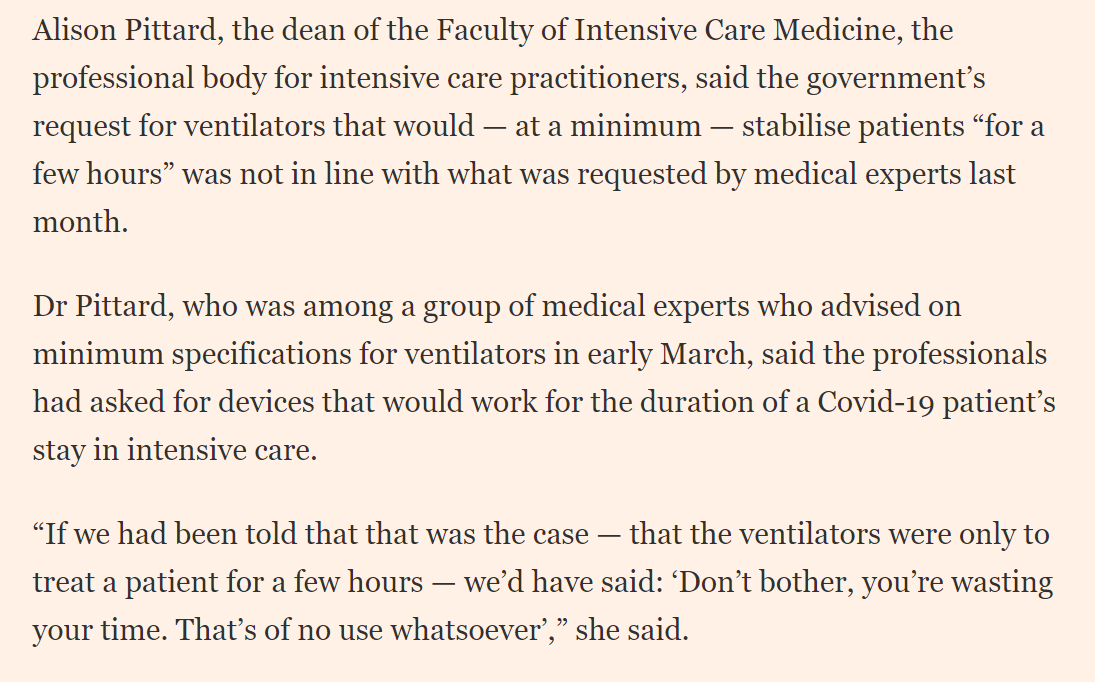
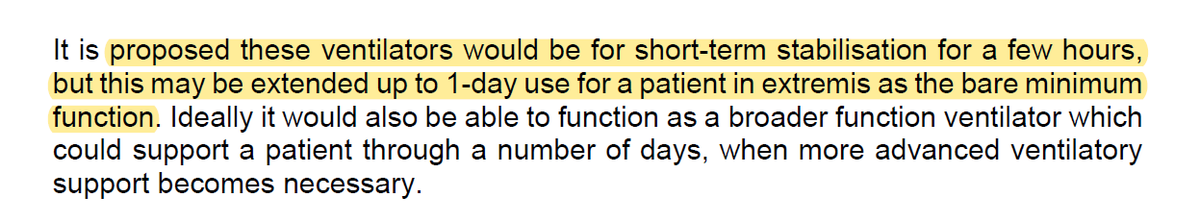
Of course, one Q is IF intensive capacity runs low, HOW does that shift balance /6
There are very tough decisions there too. That means families having difficult conversations in advance. /7
Instinctively we think ICU care is the best care - but for some it may not be so. /11
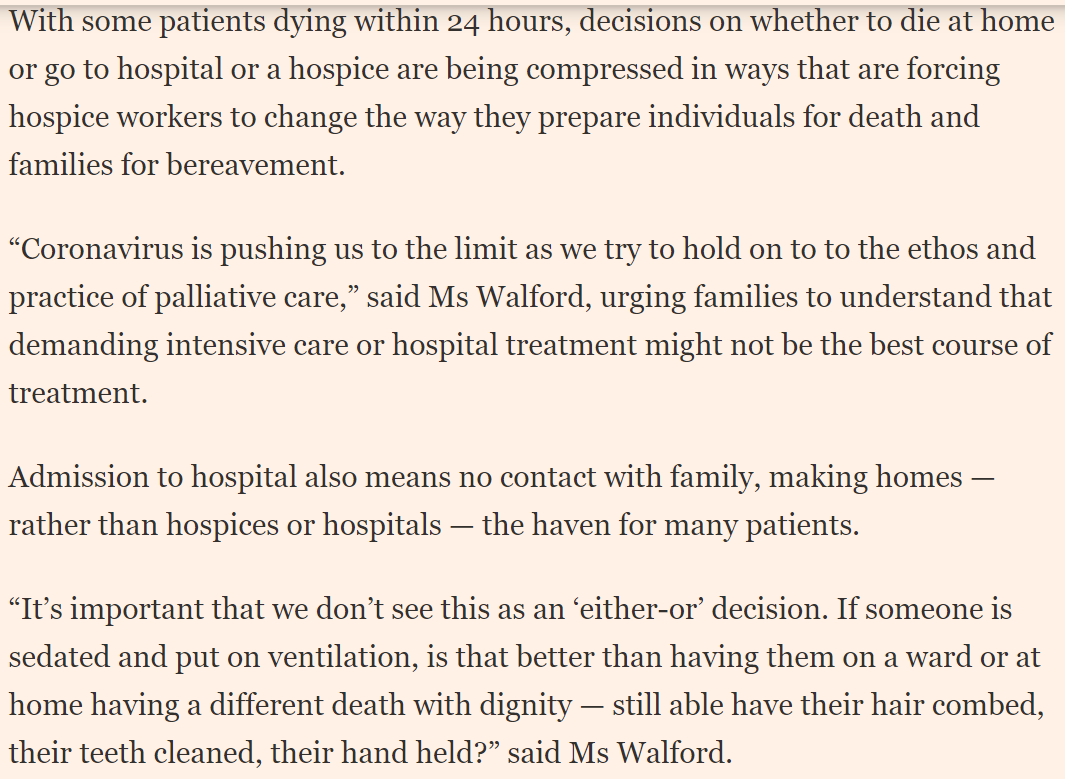
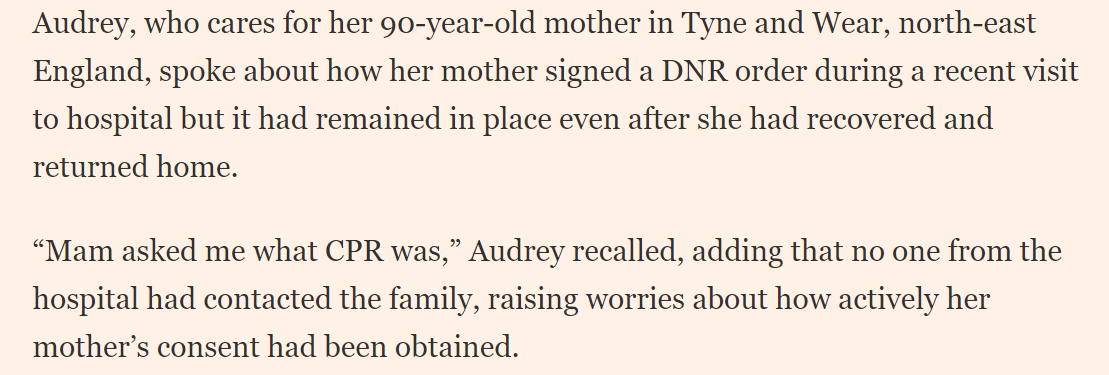
Am told the data shows resuscitation doesn't work well with elderly; more likely to lead to broken ribs, brain damage and only mildly prolonged life.
So better to go in peace?/13
As @TraceyBleakley the @hospiceuk boss told me, are we comfortable that this incredible hospice service is funded mostly via donations? /15
Perhaps #COVID19 will raise Qs over these vulnerabilities? /16
After #COVID19 perhaps this will be ONE area that actually does change. ENDS