Our study led by @KevinAnBrown associating crowding in #Ontario nursing homes (defined as the mean number of residents per bedroom and bathroom) with #COVID19 infection and mortality has now been published in @JAMAInternalMed: jamanetwork.com/journals/jamai…
1/9
1/9

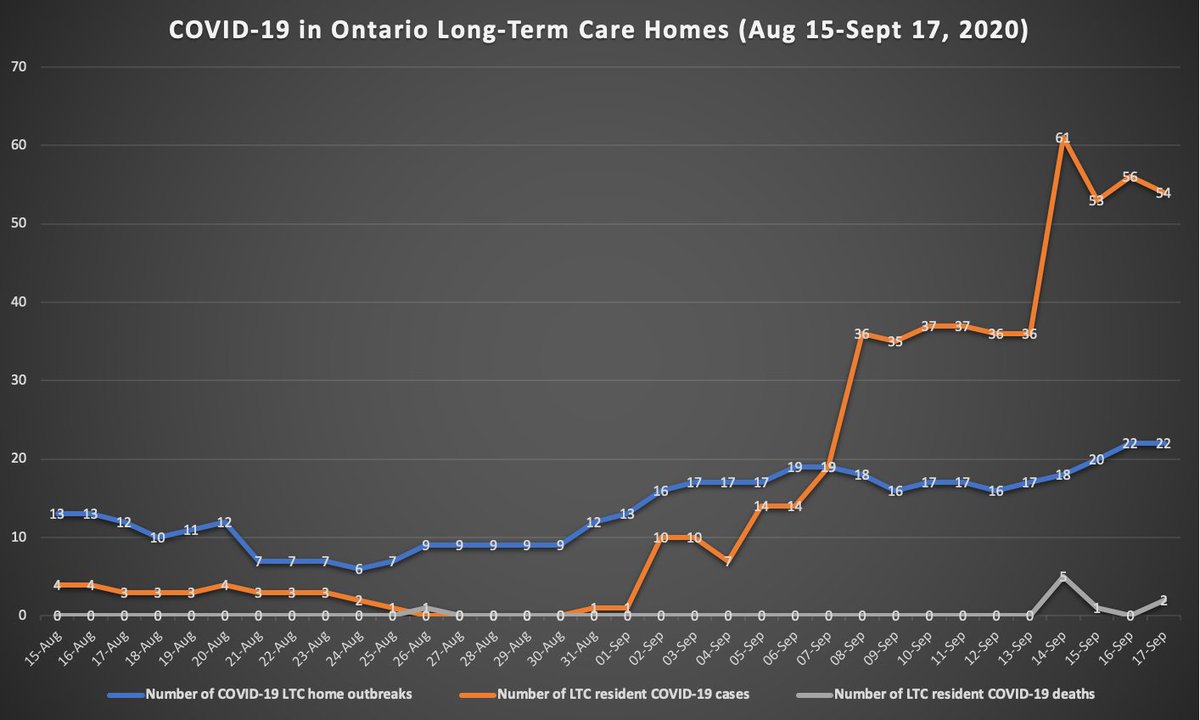
We analyzed #COVID19 incidence and mortality data for residents of nearly all of Ontario's 623 nursing homes from March 29-May 20, 2020.
As of March 29th there were 78,607 residents in these homes, with 36.9%, 37.3%, and 25.8% in single, double, and quadruple-bedded rooms.
2/9
As of March 29th there were 78,607 residents in these homes, with 36.9%, 37.3%, and 25.8% in single, double, and quadruple-bedded rooms.
2/9

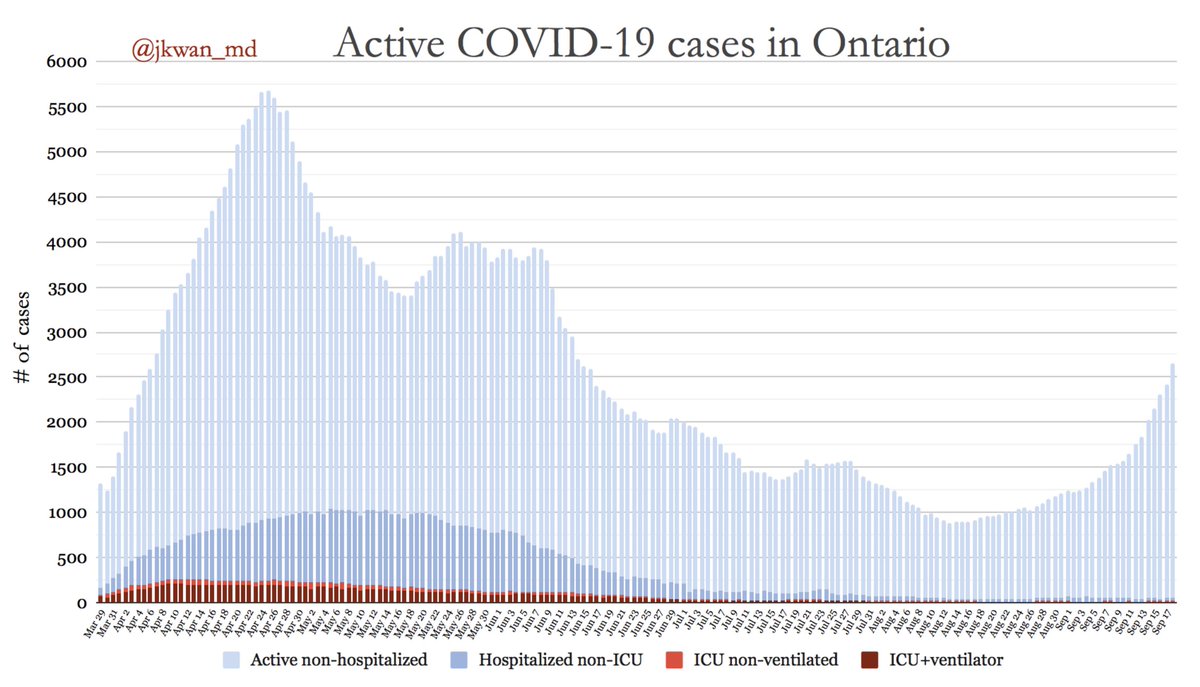
As of May 20th, 5218 (6.6%) residents developed #COVID19 infection, and 1452 (1.8%) died of #COVID19 (case fatality rate = 27.8%).
#COVID19 infection was distributed unequally across Ontario's nursing homes, with 4496 infections (86%) occurring in just 63 homes (10%).
3/9
#COVID19 infection was distributed unequally across Ontario's nursing homes, with 4496 infections (86%) occurring in just 63 homes (10%).
3/9

Compared to homes with low crowding, home with high crowding had higher #COVID19 incidence (9.7% vs. 4.5%) and mortality (2.7% vs. 1.3%).
Outbreaks in crowded nursing homes were also larger; there were 9 outbreaks involving more than 100 residents in high crowding homes.
4/9
Outbreaks in crowded nursing homes were also larger; there were 9 outbreaks involving more than 100 residents in high crowding homes.
4/9

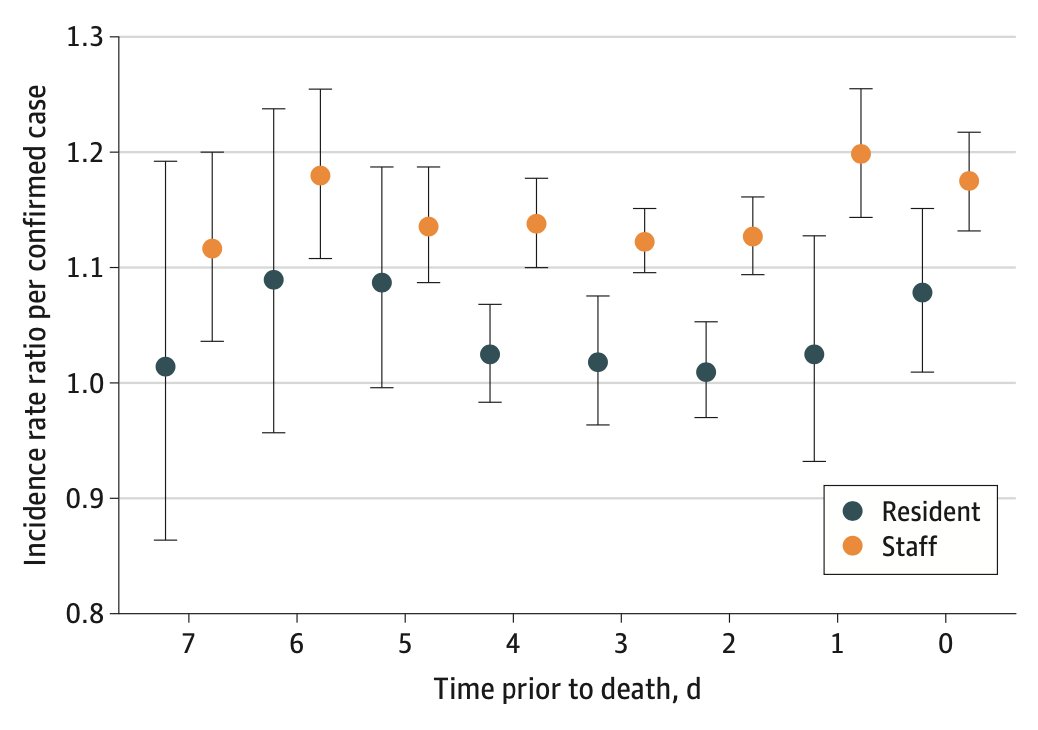
Regression models also showed that compared to nursing homes with low crowding, those with high crowding had significantly increased risk of #COVID19 incidence and mortality.
Importantly, crowding was not associated with the probability of #COVID19 introduction into a home.
5/9
Importantly, crowding was not associated with the probability of #COVID19 introduction into a home.
5/9

Simulation analyses suggested that 998 infections (19.1%) and 263 deaths (18.1%) may have been prevented if 4-bed rooms had been converted to 2-bed rooms. In this scenario, an additional 5070 new 2-bed rooms would have been needed to maintain capacity across the province.
6/9
6/9
Our results suggest that cohorting as an infection control strategy may be ineffective in crowded homes with many shared rooms.
Recognizing this, #Ontario capped the maximum room occupancy for newly admitted residents to two on June 10, 2020: health.gov.on.ca/en/pro/program…
7/9
Recognizing this, #Ontario capped the maximum room occupancy for newly admitted residents to two on June 10, 2020: health.gov.on.ca/en/pro/program…
7/9
However, as @jessiecatherine reported in @QPbriefing, Ontario's nursing homes were facing pressure at the onset of the second wave to readmit residents to multi-occupancy rooms to clear "Alternate Level of Care" patients from hospitals waiting for nursing home placement.
8/9
8/9

Overall, our findings underscore the urgency of securing temporary locations to decrowd nursing homes (e.g. underoccupied hotels or field hospitals).
In the long-term, crowded homes must be upgraded or rebuilt entirely, to convert all remaining rooms to single occupancy.
9/9
In the long-term, crowded homes must be upgraded or rebuilt entirely, to convert all remaining rooms to single occupancy.
9/9
• • •
Missing some Tweet in this thread? You can try to
force a refresh