NEJM published 2 RCTs of #AFib ablation vs AF drugs.
The rub was that the ablation was done EARLY in the course.
Practice had been to try drugs first then do ablation.
EARLY AF and STOP AF studied the procedure early.
#AHA20 Thread and my column >>
The rub was that the ablation was done EARLY in the course.
Practice had been to try drugs first then do ablation.
EARLY AF and STOP AF studied the procedure early.
#AHA20 Thread and my column >>
Both trials used the Medtronic cryoballoon system.
Medtronic participated in funding both trials.
STOP AF was 100% an industry trial. See pic.
Early AF had funding from many other sources
Medtronic participated in funding both trials.
STOP AF was 100% an industry trial. See pic.
Early AF had funding from many other sources

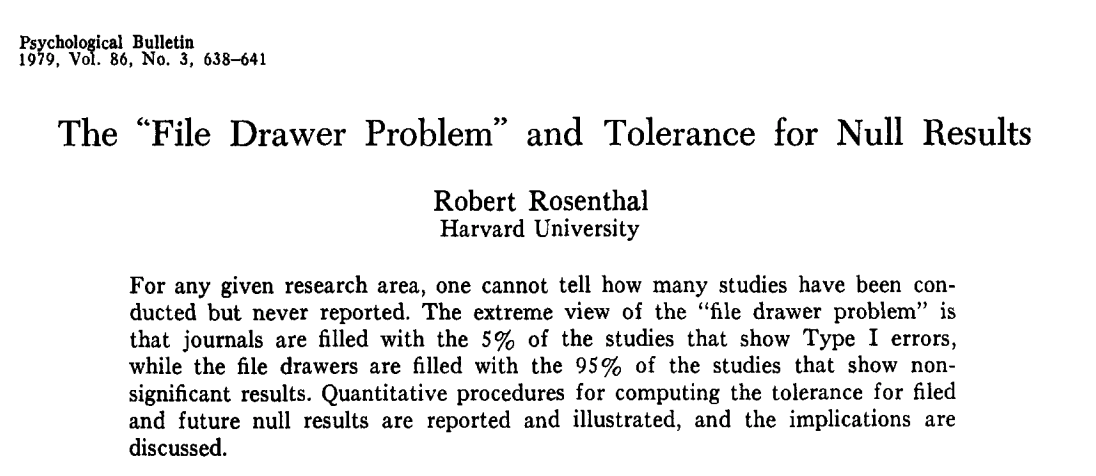
Background -- numerous trials have shown that AF ablation using different techniques (freezing or burning) can reduce AF episodes relative to meds.
In CABANA -- the largest outcome trial, AF ablation reduced AF but had no sig effect on clinical outcomes like stroke or death.
In CABANA -- the largest outcome trial, AF ablation reduced AF but had no sig effect on clinical outcomes like stroke or death.
EARLY AF and STOP AF enrolled young patients with good hearts, small left atrium and mostly low-burden AF.
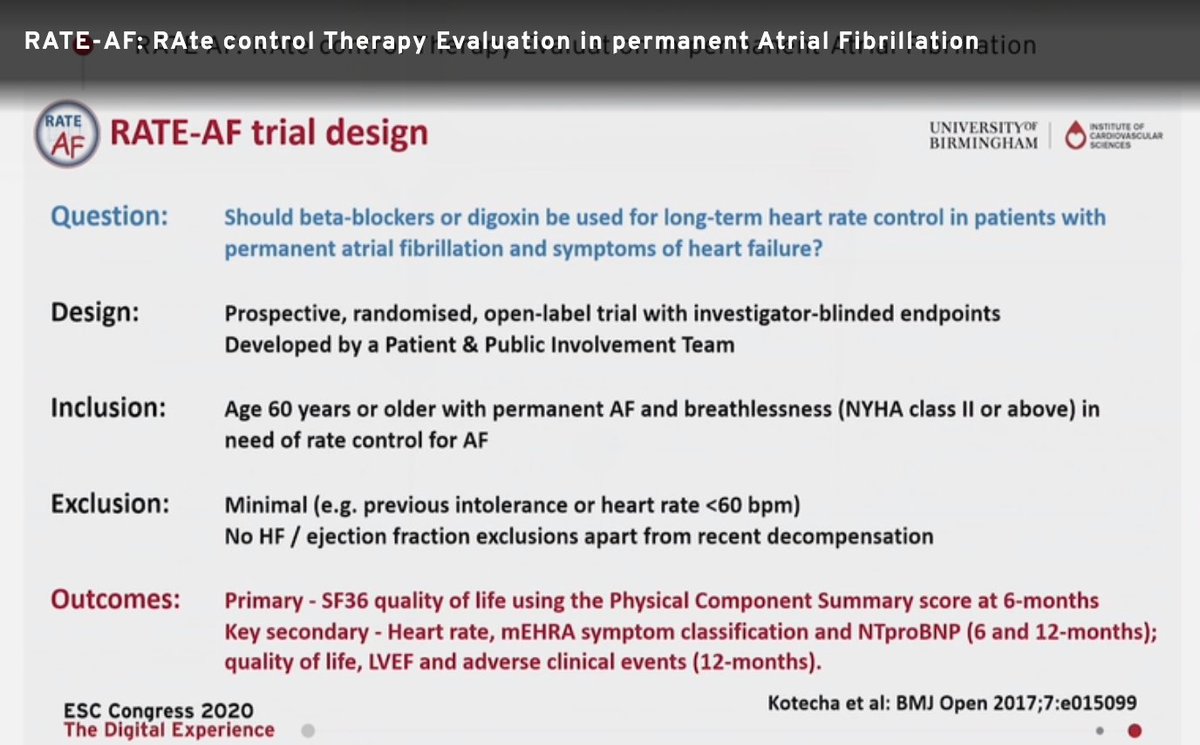
Both trials chose as their endpoint a surrogate endpoint (not stroke or death) but --essentially--an AF episode or in STOP AF, a marker of procedure failure.
Both trials chose as their endpoint a surrogate endpoint (not stroke or death) but --essentially--an AF episode or in STOP AF, a marker of procedure failure.
Both trials found that AF ablation reduces any recurrence of AF.
EARLY AF had the more rigorous design with loop recorders and maximal dosing of drugs.
Both trials reported complications from the procedure (and to an extent from the drugs)
EARLY AF had the more rigorous design with loop recorders and maximal dosing of drugs.
Both trials reported complications from the procedure (and to an extent from the drugs)
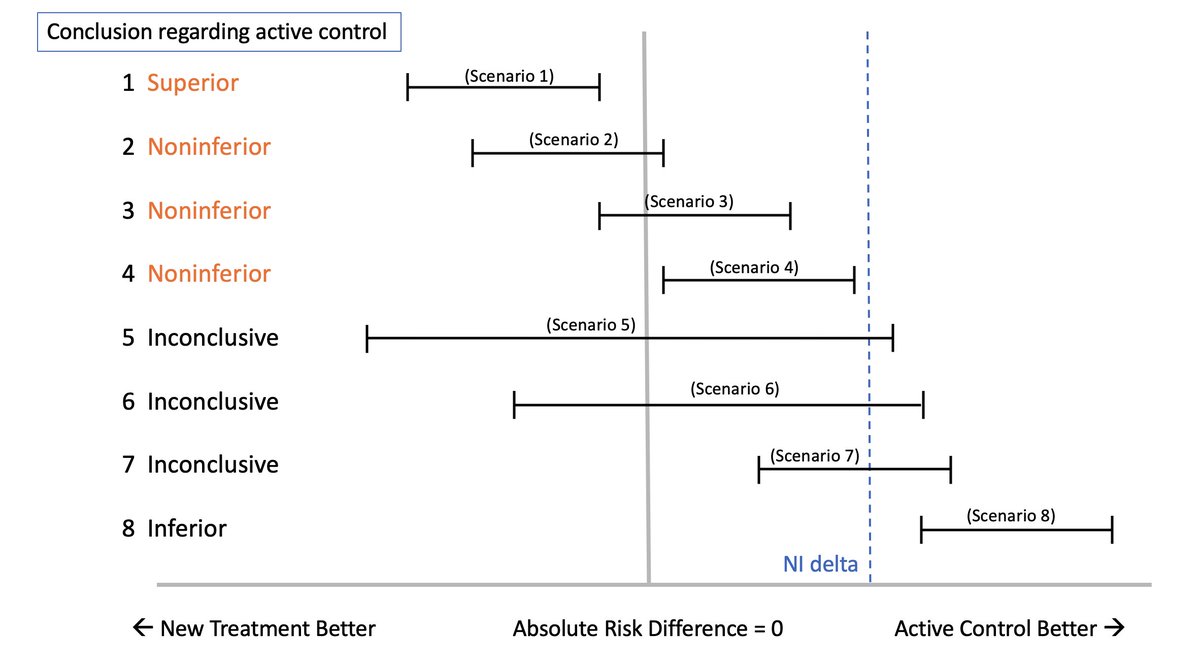
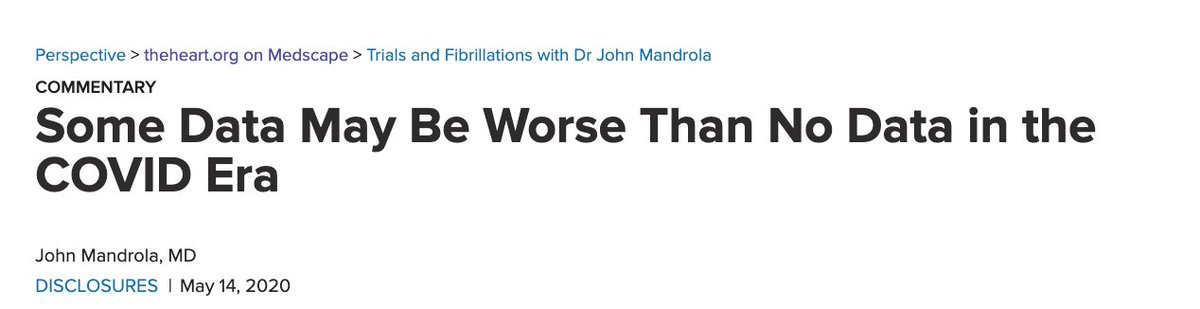
In my column I explore the translation of these trials.
I express fear that these trials may fuel a rise in inappropriate AF ablation procedures
AF ablation is well-reimbursed and is a money maker for industry, hospitals and docs. *Moral Hazard*
medscape.com/viewarticle/94…
I express fear that these trials may fuel a rise in inappropriate AF ablation procedures
AF ablation is well-reimbursed and is a money maker for industry, hospitals and docs. *Moral Hazard*
medscape.com/viewarticle/94…
But these trials have limitations.
STOP AF was hugely biased against drugs -- see my column
In EARLY AF the median AF burden in ablation arm was 0% vs 0.13% in the drug arm. Yet patients feel better after ablation????
No AF ablation trial has yet had a proper control...
STOP AF was hugely biased against drugs -- see my column
In EARLY AF the median AF burden in ablation arm was 0% vs 0.13% in the drug arm. Yet patients feel better after ablation????
No AF ablation trial has yet had a proper control...
...as Dr. Rod Gimbel points out in my piece, there ought to be an observation arm. No rhythm drugs, no ablation, just a calm caring clinician. AF often regresses
I think we also ought to have a placebo procedure arm. Like was done w single-vessel coronary disease in Orbita.
I think we also ought to have a placebo procedure arm. Like was done w single-vessel coronary disease in Orbita.
Ablation has a role in selected patients, but #epeeps ought to have the humility to realize future generations will scoff at the inelegance of this procedure.
Please do read my column and make a comment.
thanks to @theheartorg @DhirajGuptaBHRS @ftrae and Dr. P Dorian
Please do read my column and make a comment.
thanks to @theheartorg @DhirajGuptaBHRS @ftrae and Dr. P Dorian
And congratulations to the many investigators especially the PIs @DrJasonAndrade and @omwazni
Critiques of trials and commentary on how they apply in the real world should NEVER be considered personal.
Critiques of trials and commentary on how they apply in the real world should NEVER be considered personal.
• • •
Missing some Tweet in this thread? You can try to
force a refresh