New research update!
We have just completed a prospective observational study: "Clinical Trajectories of Acute Kidney Injury in Surgical Sepsis" to determine the long-term impacts of #AKI in #sepsis patients.
Read more about our study: journals.lww.com/annalsofsurger…
We have just completed a prospective observational study: "Clinical Trajectories of Acute Kidney Injury in Surgical Sepsis" to determine the long-term impacts of #AKI in #sepsis patients.
Read more about our study: journals.lww.com/annalsofsurger…
The delayed or incomplete recovery of acute organ dysfunction during sepsis is an important determinant of survival and functional recovery. Since the kidney is highly susceptible to acute dysfunction during sepsis, we studied trajectories of AKI to see how they affect outcomes.
This single-center prospective 1-year longitudinal cohort study included 239 septic patients hospitalized in a surgical ICU. Blood and urine samples were collected to characterize endothelial function, inflammation, and immunosuppression.
Clinical assessments of functional and renal status were performed at 3, 6, and 12 months after enrollment. We characterized distinct clinical trajectories for cohorts of patients with persistent and rapidly reversed AKI, and compared them to a cohort of those without AKI.
Results: persistent AKI was not only common but also carried the highest burden of the adverse outcomes. More than half of the patients with sepsis developed AKI and for two-thirds of them, renal injury persisted after 3 days. 

Patients with persistent AKI had 3-fold increase in thirty-day and 1-year mortality.
At 1-year follow up, only 57% of patients with persistent AKI were alive and among survivors, only 12% could carry on pre-disease activities without restrictions.
At 1-year follow up, only 57% of patients with persistent AKI were alive and among survivors, only 12% could carry on pre-disease activities without restrictions.
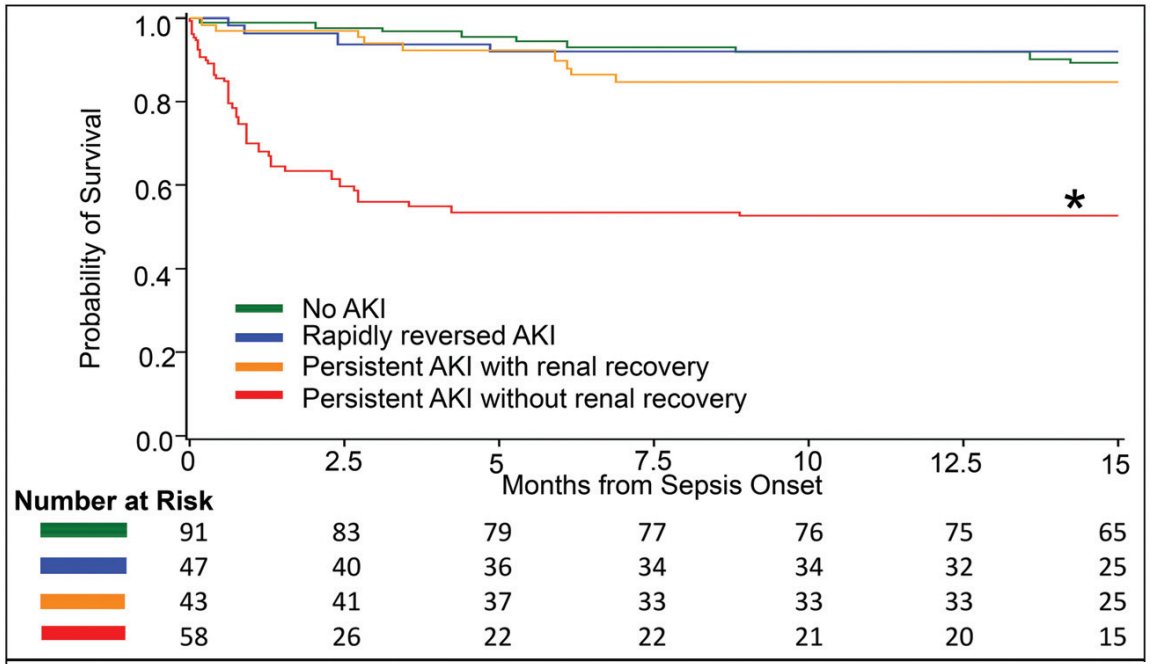
Patients with persistent AKI had a 50% rate of major adverse kidney events at 1 year, a 5-fold increase compared to patients without AKI and a 2-fold increase compared to patients with rapidly reversed AKI.
The cohort with persistent AKI exhibited more profound early physiologic derangement, persistent immune dysregulation, and endothelial dysfunction that distinctly differentiated them from patients with rapidly reversed AKI or no AKI.
Conclusions:
Among critically ill surgical sepsis patients, persistent AKI and the absence of renal recovery were associated with distinct early endothelial dysfunction, inflammation and immunosuppression, and decreased long-term physical function and survival.
Among critically ill surgical sepsis patients, persistent AKI and the absence of renal recovery were associated with distinct early endothelial dysfunction, inflammation and immunosuppression, and decreased long-term physical function and survival.
We can potentially improve rates of survival and quality of life among sepsis patients by identifying those with an increased risk for developing persistent AKI, establishing preventive strategies, and promoting renal recovery by discharge.
Shoutout to Drs. @TBaslanti, @_TylerLoftus, @rajesh_mohandas, @brakenridge_md, and @AzraBihorac for contributing to this incredible work!
Thank you to @NIGMS, @NIH, @PepperOAIC, @ncats_nih_gov, @UF, @UFMedicine @UFSurgery, @UFPHHP, and @UFAging for supporting this research.
Thank you to @NIGMS, @NIH, @PepperOAIC, @ncats_nih_gov, @UF, @UFMedicine @UFSurgery, @UFPHHP, and @UFAging for supporting this research.
• • •
Missing some Tweet in this thread? You can try to
force a refresh