Going to try to pick up where @ahandvanish left off on live-tweeting today's NIH #LongCovid workshop
https://twitter.com/ahandvanish/status/1334377560998817792?s=20
"We're really having an epidemic of this chronic critical illness and it deserves attention as well." - Dr. Terri Hough, OSU on pulmonary sequelae of #LongCovid.
GI in #LongCovid –– COVID in stool. From below slide: "as long as 5 weeks after negative respiratory PCR."
@itsbodypolitic patients have had difficulty accessing COVID stool testing but have been asking for it for months.
@itsbodypolitic patients have had difficulty accessing COVID stool testing but have been asking for it for months.

Study of 15 hospitalized patients that examined intensity of shedding and the gut microbiome.
Drop in good, rise in bad stuff in microbiome after COVID.
Drop in good, rise in bad stuff in microbiome after COVID.

Metabolic #LongCovid –– Dr. Hashem El-Serag (Baylor) 

Rheumatology and Immunology in #LongCovid with Judith James MD PhD
Talking about MIS-A, APS, vasculitis, fatigue & malaise
Talking about MIS-A, APS, vasculitis, fatigue & malaise

I'm particularly interested in APS antibodies in COVID-19. My wifi just cut out for a minute (agh!). 

Role of endothelial cell in #LongCovid vasculitis. 

#LongCovid fatigue, malaise, myalgias and arthralgias. (aghh my wifi cut out again 😫) 
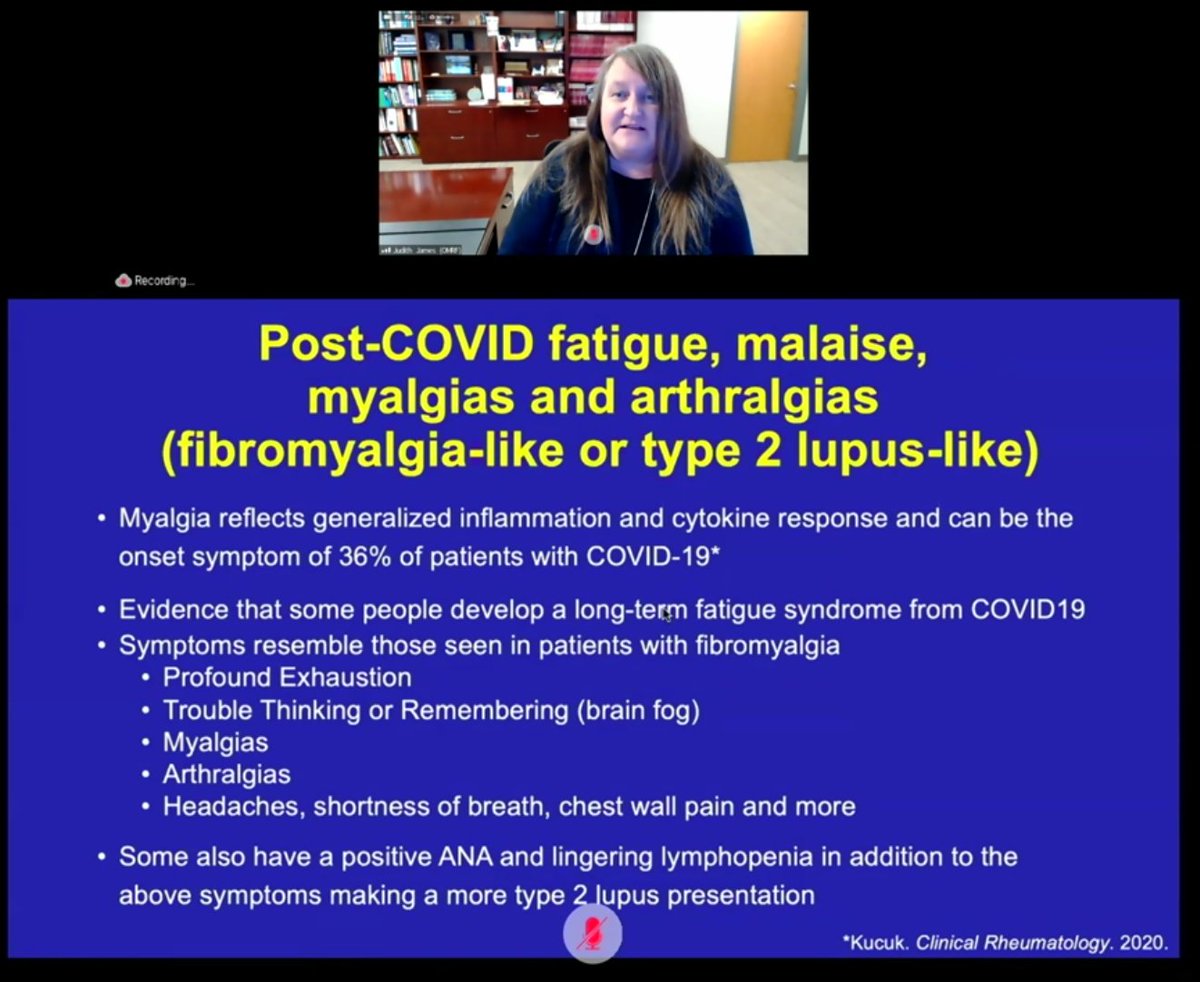
We may need to look more at prolonged lymphopenia. She says it may be found in up to 70% of COVID patients.
Autoantibodies in #LongCovid. My wifi is really cutting out so I think I need to stop live tweeting because I'm missing a lot of this. 

Considerations going forward for looking at immunology and rheumatology in #LongCovid 

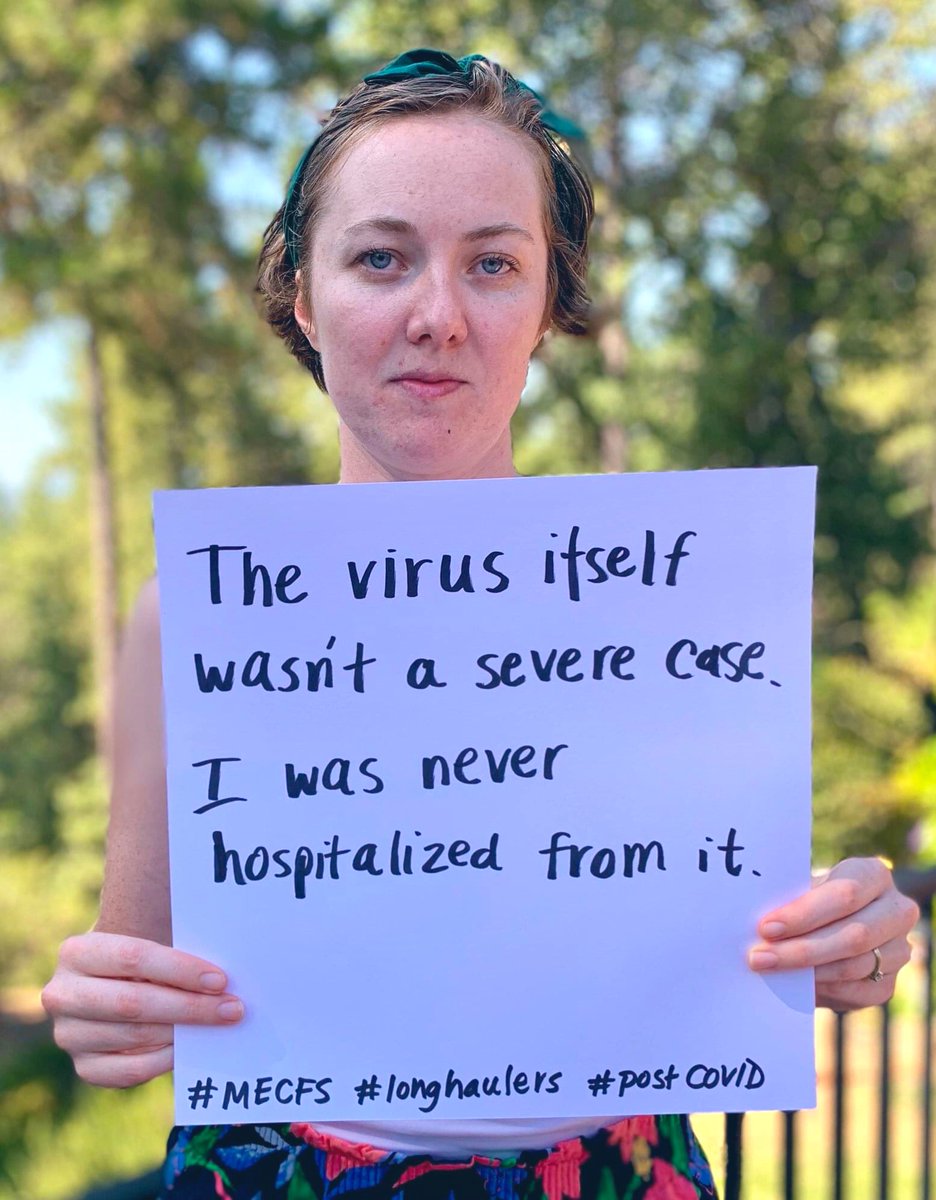
Peter Rowe on pediatric #LongCovid. Dr. Rowe studies ME/CFS at Johns Hopkins.
Shout-out to @davidtuller1 –– Dr. Rowe mentioned the press on this issue of #LongCovid in children.
Shout-out to @davidtuller1 –– Dr. Rowe mentioned the press on this issue of #LongCovid in children.

Dr. Rowe: orthostatic intolerance must be evaluated with standing test in the clinics when evaluating #LongCovid –– *ALL* #LongCovid patients he's saying.
Dr. Rowe: "We think joint hypermobility is part of the pathophysiology of the orthostatic intolerance."
New technique of measuring cerebral bloodflow is important. In #MECFS –– over threefold reduction in brain bloodflow compared to healthy controls.
New technique of measuring cerebral bloodflow is important. In #MECFS –– over threefold reduction in brain bloodflow compared to healthy controls.

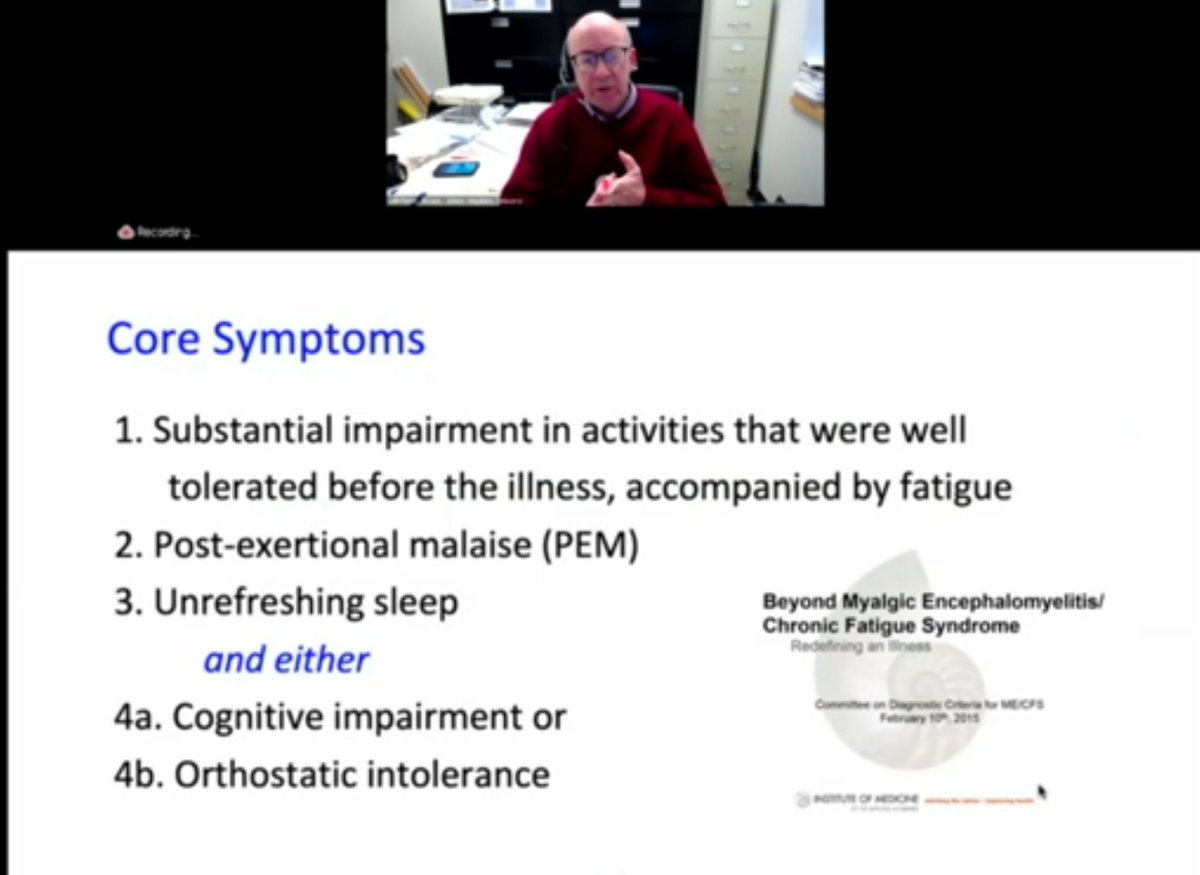
Dr. Rowe encouraging any provider new to #LongCovid to review Institute of Medicine report on #MECFS for diagnostic criteria. 
Dr. Rowe talking about wellness score. Mean wellness score in #MECFS: 50. Health patients: 90. #LongCovid patients: 40. 😳 (Wellness = 100 well, 0 unwell.) 

Dr. Rowe describing a case study: an adult female patient who is a PhD scientist. #LongCovid meant "she couldn't make sense of her bank statement" or "follow a TV show" anymore. A PhD scientist.
Goes on to describe that this patient experiences significant #PostExertionMalaise
Goes on to describe that this patient experiences significant #PostExertionMalaise

Dr. Rowe describes a 19-year-old univ. student who ran on cross country team. Now plays a backyard game of cornhole and gets 3 days of #PostExertionMalaise. 

Dr. Rowe: stop recommending GET. We must not make the same mistakes as we did decades ago with this, again with #LongCovid. 

Dr. Rowe knocked it out of the park with his segment just now. Wow. 👏
Oh, and Dr. Rowe made sure to clarify here: this patient's symptoms and #PostExertionMalaise started far before deconditioning could have been a consideration here. (Remember this patient was the cross country athlete before #COVID.)
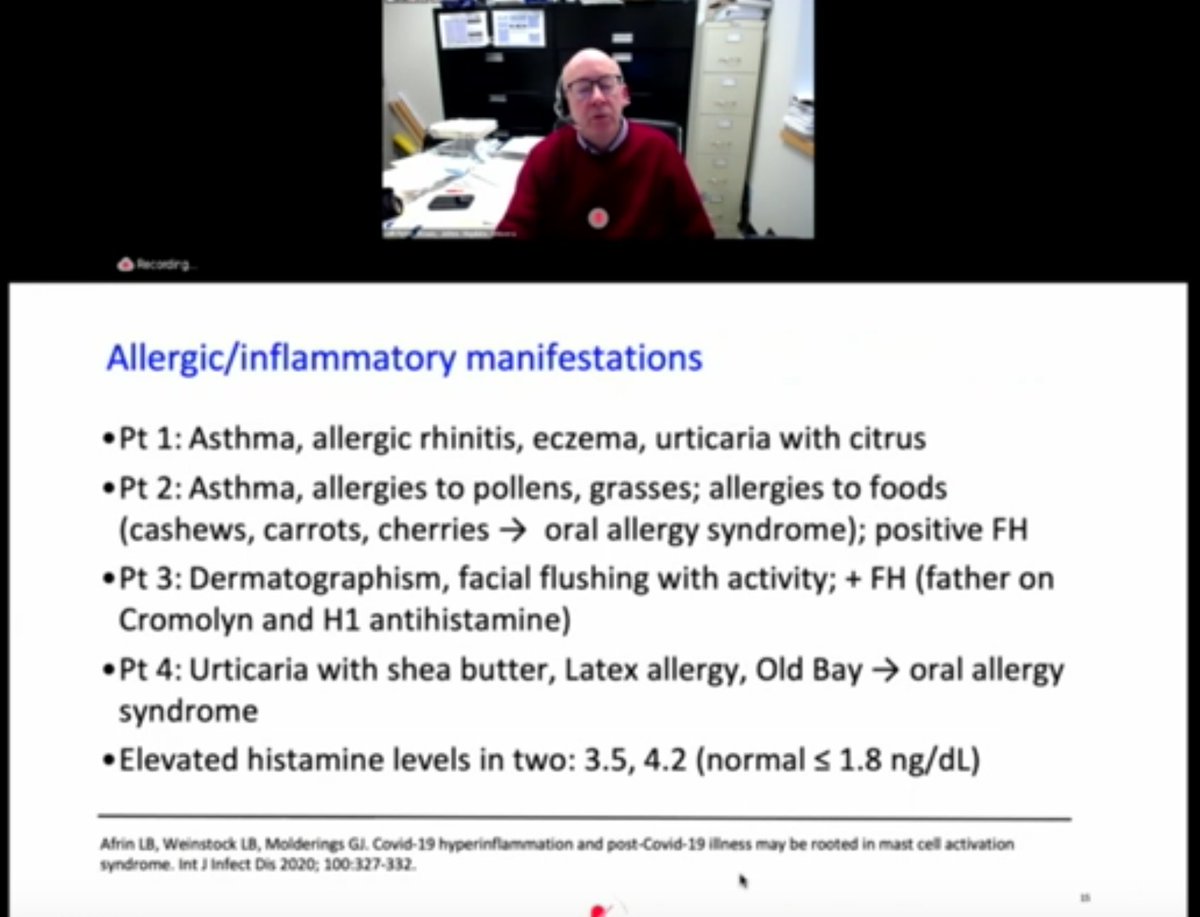
Dr. Rowe: on allergic manifestations of #LongCovid. Nod to Dr. Afrin's work on #MCAS. Need more research here. Mentioned trials on famotidine and antihistamines during acute COVID
Q&A session: are there studies on sleep disorders in #LongCovid? Both Dr. Nath and Terri Hough (OSU) say this is needed. Terri Hough says sleep issues do a great job knitting all the symptoms together. (Her quote was really good but I didn't catch the whole thing)
Q&A: answer on immunity from Judith James –– we need to expand looking at antibody responses. Acknowledges early antibody tests were not ideal. (@itsanginLA I thought of you here)
Q&A: Q for Dr. Judith James, rheum/immune. Dr. James: We need many large cohorts to study this area: We're seeing some individuals developing multiple antibodies, higher titer antibodies, or disease-specific antibodies...
...Con't Q&A on that answer: It's important that we follow those patients longitudinally to see if they develop other autoimmune diseases later.
Q&A: CPET question. Dr. Rowe: 2-day consecutive CPET has been used to document disability in #MECFS because they show a reduction of work capacity even though putting forward maximal effort. 2-day CPET may be a helpful tool in measuring #LongCovid
Watching today’s event + live tweeting the part I covered took all my energy today. It all happened so fast that I didn’t have time for image descriptions. If anyone wants to help with writing image descriptions for the slides I would really appreciate it!
• • •
Missing some Tweet in this thread? You can try to
force a refresh