Watching day 2 of @NIAIDNews #LongCovid workshop. Right now: breakout sessions. I'm watching the neuro breakout session, led by Dr. Komaroff. @ahandvanish is there representing #LongCovid patients with @itsbodypolitic. Tune in: videocast.nih.gov/livew.asp?live…
@NSU_INIM's Dr. Klimas spoke about early in the meeting about the history of #MECFS and challenges in developing diagnostic criteria for #MECFS without biomarkers, and the similarities and differences to #LongCovid. I felt represented by her discussion as a #PwME
@NSU_INIM's Dr. Klimas also emphasized the need for separating
- hospitalized COVID patients with organ damage that is causing neuro symptoms after COVID
vs.
- #LongCovid which typically is in non-hospitalized cases
- hospitalized COVID patients with organ damage that is causing neuro symptoms after COVID
vs.
- #LongCovid which typically is in non-hospitalized cases
Dr. Walitt from #MECFS and #LongCovid NIH study echoed that in the interviews the are doing for #LongCovid, they are hearing that these patients are appearing to recover after acute COVID, and then the #LongCovid symptoms start later. Then up and down with symptoms.
He said that we will need to pay attention to this in designing research to study #LongCovid.
Dr. Klimas briefly just mentioned theory of "oxidative stress causing neuroinflammation." Could be that people age 40+ are depleted in antioxidants. (#LongCovid patients should definitely check out her youtube video on post-COVID treatment where she talks about this.) @NSU_INIM
Definitely a lot of mention of #MECFS today on this breakout. Also mention of #brainfog, cognitive dysfunction, discussion: is this active virus or after? (Consensus seems to be after.)
Dr. Perlman, who has worked on coronaviruses for decades, said that we didn't see something like #LongCovid in SARS and MERS. He suspects immune activation and/or vasculitis may be part of #LongCovid.
Dr. Perlman: I don't know if this is something where COVID comes and hits and leaves (they keep referring to this as hit-and-run during this workshop), or if it's a longer process. It's definitely different than after SARS and MERS.
Dr. Nath: Do you think the reason we don't find the virus in the other organ systems is because there's no viremia at all?
Dr. Komaroff, leading the breakout: A lot of support that this is largely an endothelial cell function disease. Does anyone disagree?
Eva Feldman: Talking about #dysautonomia presenting with fatigue, brain fog, headache etc. Please let's not neglect that there may be a lot of #dysautonomia contributing to these symptoms. Let's be careful not to put all of these into one box.
What do you think mediates the dysautonomia, Dr. Feldman? Dr. Feldman asked Dr. Nath if they had autopsies from @NIHClinicalCntr. (Dr. Nath has been leading the #MECFS @IRPatNIH study which also looked at dysautonomia at NIH clinical center.)
(I missed live tweeting some of Dr. Nath's response because I had to stop to drink some @liquidiv because my #POTS is not happy I'm up this early using my brain)
CDC Dr. Sejvar: How does COVID cause neurologic disease –– we're currently limited to testing CSF right now. CDC is trying it's best to psuedo-standardize some assays right now. Question to group: how do we go about looking at the virus in the CSF from PCR/antibody perspective?
Answer: (I can't see who's talking, they must be off screen): Look for proteins instead of active virus. We need to spend more time in proteomic studies.
This from a doctor with experience in acute and post-acute COVID.
This from a doctor with experience in acute and post-acute COVID.
Dr. Komaroff (leading breakout group): are there animal models that should be used with post-COVID neurologic disease?
Dr. Perlman: My lab has spent a lot of time looking at coronaviruses and neural infection with them. [Summarizing:] We are working on it.
Dr. Perlman: My lab has spent a lot of time looking at coronaviruses and neural infection with them. [Summarizing:] We are working on it.
Dr. Perlman: Nothing we can hang our hats on yet. No perfect models yet.
With SARS-COV2, it's clearly different than SARS.
With SARS-COV2, it's clearly different than SARS.
Dr. Klimas is excited about Dr. Perlman's work. In #MECFS, we have yet to establish an animal model in 30 years of trying. It would be very interesting with this particular infection (COVID), if it drove systemically or neurologically, it could be a good animal model for #MECFS.
Dr. Klimas: the animals give us the opportunity to understand the #LongCovid in the 2 years, 3 years, 5 years modeled out. People with #MECFS in the first 3 years have a different signature than people 3+ years.
Please think about how you might intervene early with #LongCovid
Please think about how you might intervene early with #LongCovid
Dr. Walitt (NIH): about animal models themselves –– we're talking about infecting animals to see what happens. But do we have testing to capture #LongCovid in these animals? Can we do autonomic testing, peripheral neuropathy testing on animals? How to test brain fog in a rodent?
Dr. Feldman said they can do that at their lab (which is NIH funded.) But question is, we don't know what animal model to use? (Like, which animal.)
Dr. Perlman: this is evolving. A few months ago people said hamsters and non-human primates are best.
Dr. Perlman: this is evolving. A few months ago people said hamsters and non-human primates are best.
Dr. Perlman cont'd: mice had to be manipulated so they could be infected. He said we're getting closer.
In 2007, he remembers working on brain infections with SARS and there wasn't much interest because people didn't think it was possible.
In 2007, he remembers working on brain infections with SARS and there wasn't much interest because people didn't think it was possible.
Dr. Klimas has an immunology question for Dr. Perlman: Do we have to start from a COVID model? Is there a better infection to use?
Dr. Perlman: For this kind of study, I think you want to start with SARS-COV2.
Dr. Perlman: For this kind of study, I think you want to start with SARS-COV2.
Dr. Klimas asks Dr. Perlman: What about COVID reactivating viruses? (We've heard this happening in @itsbodypolitic with EBV, CMV, shingles in #LongCovid.)
Dr. Perlman said they haven't looked at this.
Dr. Perlman said they haven't looked at this.
Dr. Morgello: she is trying to figure out where the viral shedding is coming from. Is it coming from GI? It's hard to understand with patients who have documented long viral shedding times, where it's coming from. She doesn't think it's from the brain
Dr. Perlman: It can be really hard to find viral RNA in the brain.
Dr. Klimas: talking about CDC funded study with @NSU_INIM
They are going to text message 50,000 COVID patients via public health department to focus on post-COVID illness. The focus here is #LongCovid / #MECFS-like illness. Longitudinally follow several thousand people
They are going to text message 50,000 COVID patients via public health department to focus on post-COVID illness. The focus here is #LongCovid / #MECFS-like illness. Longitudinally follow several thousand people
A subset of those people will be invited for in-person for deep phenotyping and biomarker surveys, clinical assessments, neurocognitive assessments.
Dr. Feldman at UofMichigan with NIH funding –– they are looking at initial trajectory and set of inflammatory markers. Now they are being called back 3-7 months after infection and getting deep phenotyping. Autonomic testing, electrophysiological testing, Echocardiograms, ...
Renal ultrasound, and more. They will follow every 6 months. They are looking at a cohort of about 300 patients.
Dr. Komaroff asked: Dr. Feldman, will the questions you are asking of the patients in that cohort, allow you to determine if these patients meet the criteria for #MECFS? The answer: yes.
Laura Jehi with Cleveland Clinic also has NIH funding to work on this. They are looking at what patients are at highest risk of developing neurological complications by using a registry at Cleveland Clinic. Matching COVID positive with demographic/age etc. matched controls
Quality of life, depression screenings are included in the data they are looking at.
They've also built models to calculate risk of COVID progression to ICU, hospitalization. They can build off of that work also.
They've also built models to calculate risk of COVID progression to ICU, hospitalization. They can build off of that work also.
They've also built a COVID biobank. They will combine genomics data plus biobank.
One strength, they have data on these patients prior to COVID. So they can see how baseline changes prior to COVID to post COVID. They have this longitudinal data for a decent number of patients.
One strength, they have data on these patients prior to COVID. So they can see how baseline changes prior to COVID to post COVID. They have this longitudinal data for a decent number of patients.
Dr. Koralnik: they are also measuring cognition at his clinic for memory, attention, executive function, processing speed) in his clinic. (Northwestern, I think.) He is interested in seropositive vs. seronegative #LongCovid.
Dr. Koralnik said they may be finding T Cells similar between seropositive vs. seronegative #LongCovid patients, so that may be one way to help prove infection in seronegative (lots of testing barriers for these patients.)
Dr. Koralnik: there is a significant need from @NIH for funding for looking at neurological #LongCovid. There is not enough currently.
(I think #PwME would agree with you, Dr. Koralnik)
(I think #PwME would agree with you, Dr. Koralnik)
Laura Jehi - Cleveland clinic. She said for their large registry, they have I think she said several hundreds of thousands of patients. And ~300 data points on each of them.
But the funding for #LongCovid, is just from a supplemental funding source. It's limited to neuro issues.
But the funding for #LongCovid, is just from a supplemental funding source. It's limited to neuro issues.
They could look at additional areas beyond neuro with additional funding because the pipelines is already built.
Vicky Whittemore at NINDS said they are discussing funding for this research. There were a *lot* of questions from researchers in the zoom chat, Dr. Komaroff said, about how to get funding for this. @NINDSfunding
Dr. Komaroff asked if there are any studies happening looking at #LongCovid in existing neuro patients. @ahandvanish mentioned @patientled research –– stay tuned for their preprint.
Breakout sessions over now; here's a photo of neuro one. As a person w/ post-viral #MECFS I feel hopeful by the conversation that just happened. Now I really hope that gov't can provide additional funding, as there are a lot of researchers ready & willing to work on #LongCovid 

Dr. Komaroff summarizing neuro breakout session:
- how variable the answer to the question "What's the prevalence of neuro diseases in #COVID in the literature?" Different studies were studying very different kinds of patients. And some studies were well-done prospective studies
- how variable the answer to the question "What's the prevalence of neuro diseases in #COVID in the literature?" Different studies were studying very different kinds of patients. And some studies were well-done prospective studies
...with standard neuro exam. Whereas some were retrospective looking at whatever was in medical chart. These can produce different answers
Neuro topics Dr. Komaroff's breakout group on #LongCovid focused on:
- cognitive deficits
- vascular mediated complications, both ischemic & hemorrhagic
- neuropsychiatric disorders
- neurogenic respiratory failure (Ondine's curse)
- #dysautonomia –– a *lot* of this (disabling)
- cognitive deficits
- vascular mediated complications, both ischemic & hemorrhagic
- neuropsychiatric disorders
- neurogenic respiratory failure (Ondine's curse)
- #dysautonomia –– a *lot* of this (disabling)
Consensus:
- not a lot of evidence of virus in the brain or ACE2 receptors in the brain
- probably response to the virus is what causes the morbidity
- not a lot of evidence of virus in the brain or ACE2 receptors in the brain
- probably response to the virus is what causes the morbidity
The one clear theme in the brain (and probably other organs) is the endothelial dysfunction probably triggered by viral infection of the endothelial cells.
Endothelial dysfunction is important to the neuropathology of #LongCovid.
Endothelial dysfunction is important to the neuropathology of #LongCovid.
We need good studies looking on neurological disorders in #LongCovid. We will need these to identify the long-term history of the neurologic deficits are going to be in this illness. Will it be #MECFS?
Challenge for studying: waxing and waning course in #LongCovid patients.
Challenge for studying: waxing and waning course in #LongCovid patients.
Some of these studies already in progress. There is a significant need for more funding.
- @IRPatNIH with Dr. Nath
- @NSU_INIM with Dr. Klimas' CDC grant
- @ClevelandClinic
- Univ. of Michigan
- Dr. Koralnik's at Northwestern
Others I can't remember bc #brainfog
- @IRPatNIH with Dr. Nath
- @NSU_INIM with Dr. Klimas' CDC grant
- @ClevelandClinic
- Univ. of Michigan
- Dr. Koralnik's at Northwestern
Others I can't remember bc #brainfog
Cardiovascular breakout summary:
- does acute treatment affect #LongCovid? Important to follow patients who enrolled in acute clinical trials for treatments, to see if it impacts #LongCovid later
- how to differentiate PTSD/psychiatric from cardiovascular damage symptoms
- does acute treatment affect #LongCovid? Important to follow patients who enrolled in acute clinical trials for treatments, to see if it impacts #LongCovid later
- how to differentiate PTSD/psychiatric from cardiovascular damage symptoms
Cardiovascular breakout summary:
- racial disparities in acute COVID infections could exacerbate existing cardiovascular disease
- a lot of question about clinical significance of abnormalities of cardiac MRI and echocardiogram during acute and #LongCovid
- racial disparities in acute COVID infections could exacerbate existing cardiovascular disease
- a lot of question about clinical significance of abnormalities of cardiac MRI and echocardiogram during acute and #LongCovid
Cardiovascular breakout summary:
- a lot of questions about exercise recommendations, how to clear COVID patients for exercise (both professional athletes and not)
- how might immune system be affected by stress of COVID
- partnerships: how do we reach diverse communities?
- a lot of questions about exercise recommendations, how to clear COVID patients for exercise (both professional athletes and not)
- how might immune system be affected by stress of COVID
- partnerships: how do we reach diverse communities?
Cardiovascular breakout summary:
- lot of Cardiac MRI abnormalities discussion. Need more detail and to understand importance
- need to study biomarkers and genomic predictors
- CPET to differentiate pulmonary vs. cardiac causes of shortness of breath
- lot of Cardiac MRI abnormalities discussion. Need more detail and to understand importance
- need to study biomarkers and genomic predictors
- CPET to differentiate pulmonary vs. cardiac causes of shortness of breath
Cardiovascular breakout summary:
- heart rate variability for autonomic measure
- a bunch more tests I missed (she's talking quickly, sorry!)
- menstrual cycles in relation to #LongCovid deserves more study
- need longitudinal studies
- wearable devices for studies
- heart rate variability for autonomic measure
- a bunch more tests I missed (she's talking quickly, sorry!)
- menstrual cycles in relation to #LongCovid deserves more study
- need longitudinal studies
- wearable devices for studies
Cardiovascular breakout summary:
- self-referral into research studies to engage community
- importance of patient representatives in research
- opportunities to improve data analytics (like AI going thru EMR's)
- self-referral into research studies to engage community
- importance of patient representatives in research
- opportunities to improve data analytics (like AI going thru EMR's)
Dr. Lerner from NIAID, organizer of this workshop, agrees that addressing racial disparities is important.
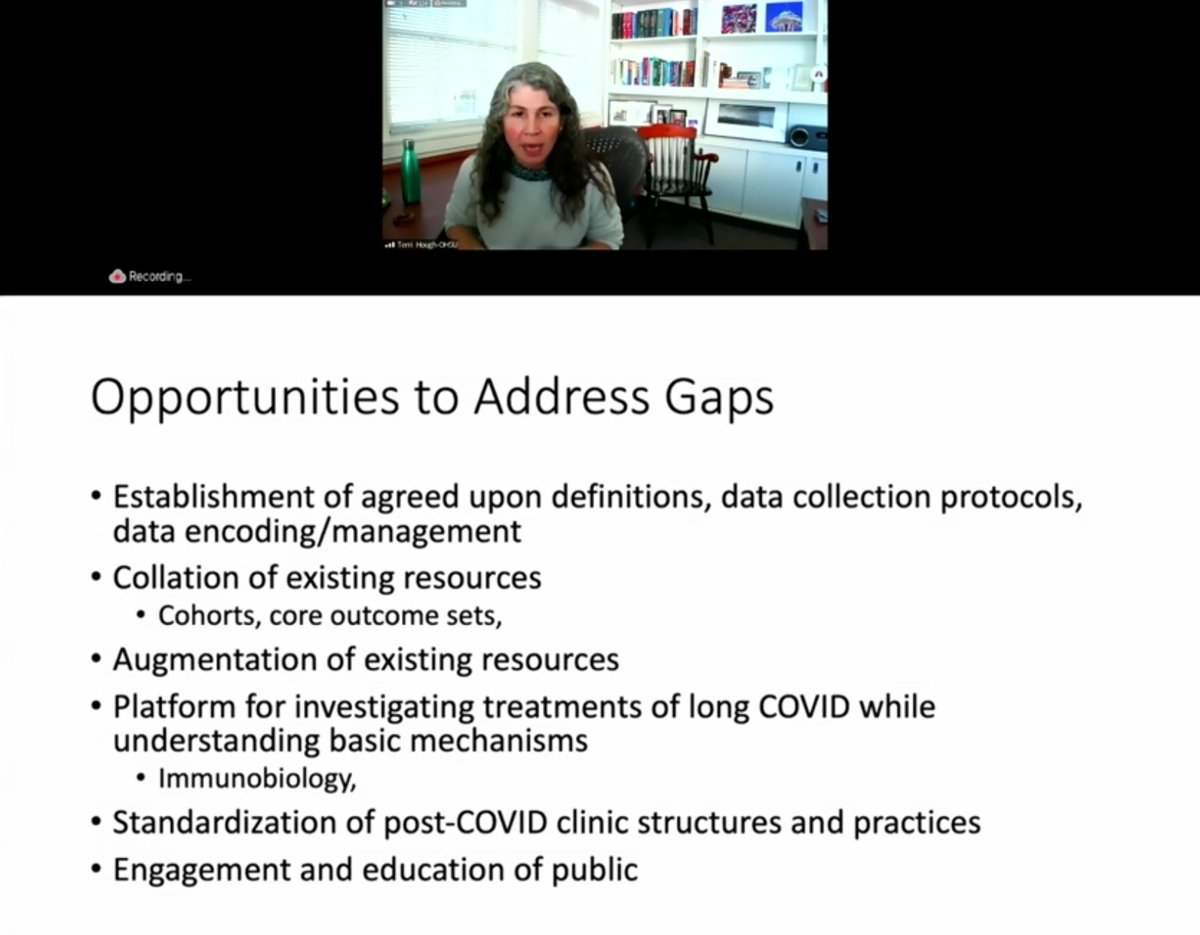
Dr. Hough OHSU on pulmonary breakout:
- representation from nursing, rehab scientists, basic scientists, emergency med docs, inpatient and outpatient and more
- important questions to ask:
- representation from nursing, rehab scientists, basic scientists, emergency med docs, inpatient and outpatient and more
- important questions to ask:
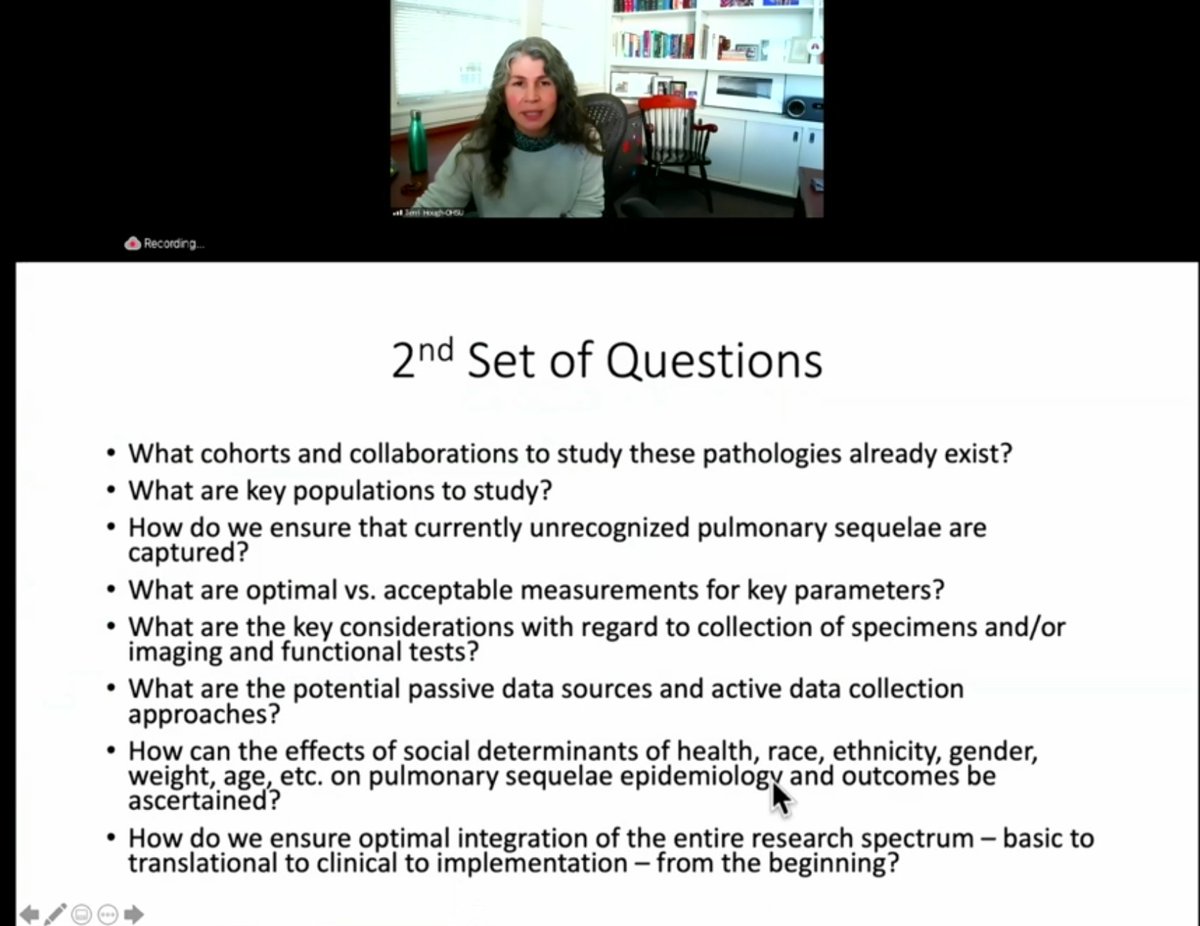
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- need to agree on language to describe this (what do we name this?)
- not enough research on first few days of COVID infection
Key identified gaps below in image:
- need to agree on language to describe this (what do we name this?)
- not enough research on first few days of COVID infection
Key identified gaps below in image:
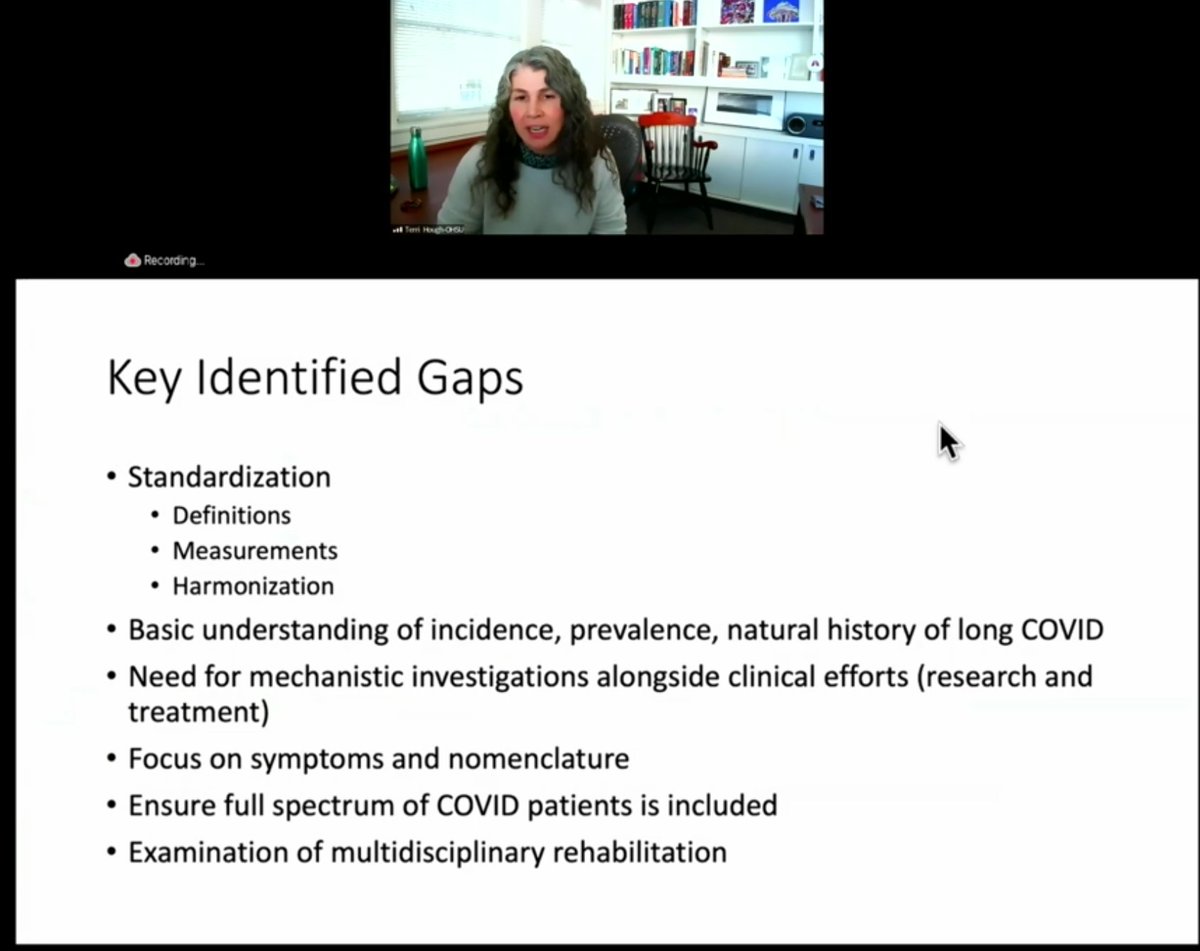
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- need to work together on agreed upon definitions of #LongCovid, as well as data collection and ways to harmonize data
- need to work together on agreed upon definitions of #LongCovid, as well as data collection and ways to harmonize data
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- need to focus on best approaches to collecting data on social determinants of health. This needs to be built in the beginning of the research, not added on in the end.
- need to focus on best approaches to collecting data on social determinants of health. This needs to be built in the beginning of the research, not added on in the end.
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- we need immediate work on significant life-altering #dyspnea after #COVID19.
- we need to start studying treatments for this
- we need immediate work on significant life-altering #dyspnea after #COVID19.
- we need to start studying treatments for this
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- Consider trials platform. Instead of us all making up what the best treatments are for dyspnea, chronic cough, we can start to actually answer these questions. Also think a platform would be great for nested cohorts studies
- Consider trials platform. Instead of us all making up what the best treatments are for dyspnea, chronic cough, we can start to actually answer these questions. Also think a platform would be great for nested cohorts studies
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- how to leverage post-COVID clinics for rolling out interventional work
- importance of studying delivery of care during post-COVID
- how to leverage post-COVID clinics for rolling out interventional work
- importance of studying delivery of care during post-COVID
Dr. Hough OHSU on pulmonary breakout on #LongCovid:
- important: we know COVID experience is so rapidly evolving. Remember that one cohort of March 2020 may well not describe in later cohorts, as the virus evolves, as patients are different, as treatments are different.
- important: we know COVID experience is so rapidly evolving. Remember that one cohort of March 2020 may well not describe in later cohorts, as the virus evolves, as patients are different, as treatments are different.
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic:
- first, he did a shout-out directly to @itsbodypolitic 's own Lauren Nichols who participated in the breakout session. Dr. H said Lauren's personal story with #LongCovid was really impactful on the breakout group.
- first, he did a shout-out directly to @itsbodypolitic 's own Lauren Nichols who participated in the breakout session. Dr. H said Lauren's personal story with #LongCovid was really impactful on the breakout group.
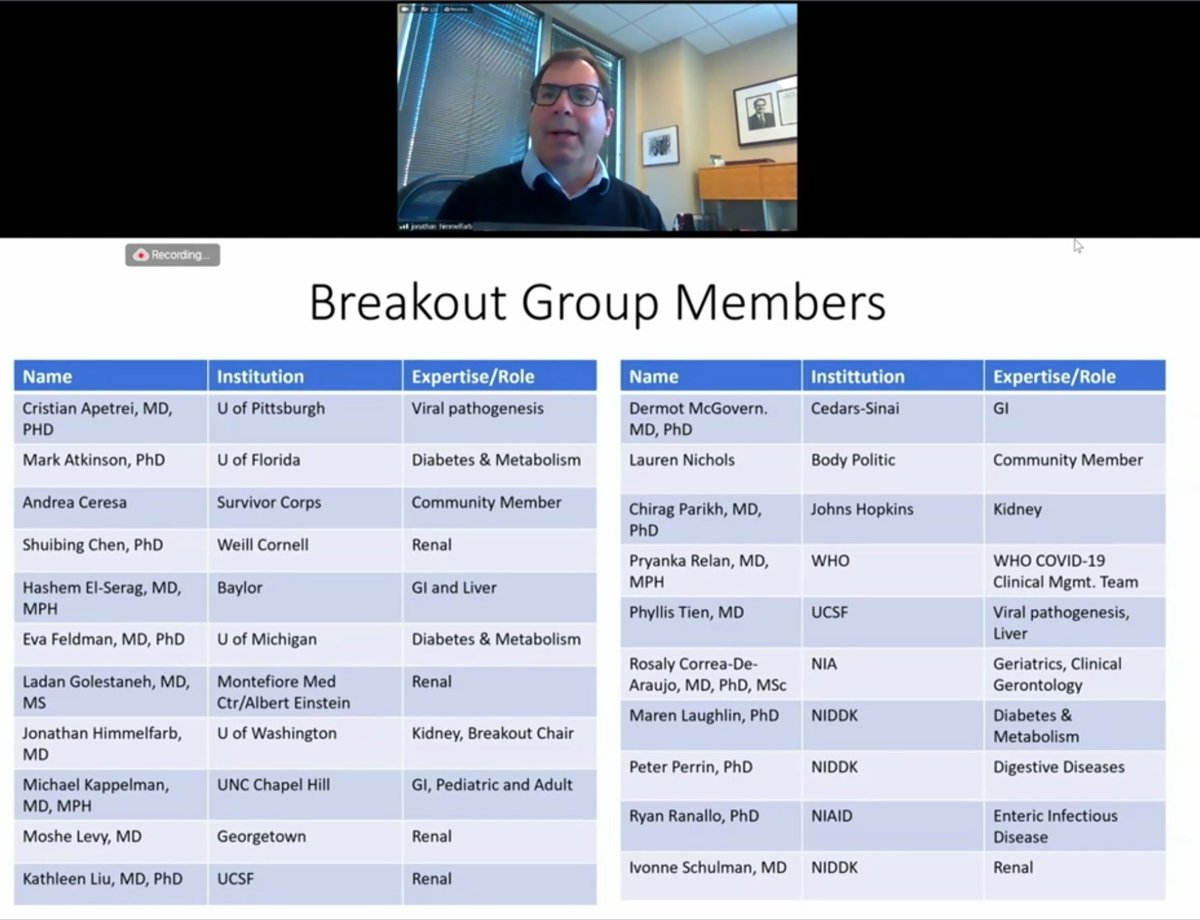
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid:
- kidney disease discussions relevant to diverse, multiple populations
- kidney complex organ. different injuries to kidney with likely different long-term complications
- kidney disease discussions relevant to diverse, multiple populations
- kidney complex organ. different injuries to kidney with likely different long-term complications
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid:
- need to look at social determinants of health
- Slide below: likely long-term renal consequences. A lot of text –– will try to add image description after live tweet
- need to look at social determinants of health
- Slide below: likely long-term renal consequences. A lot of text –– will try to add image description after live tweet
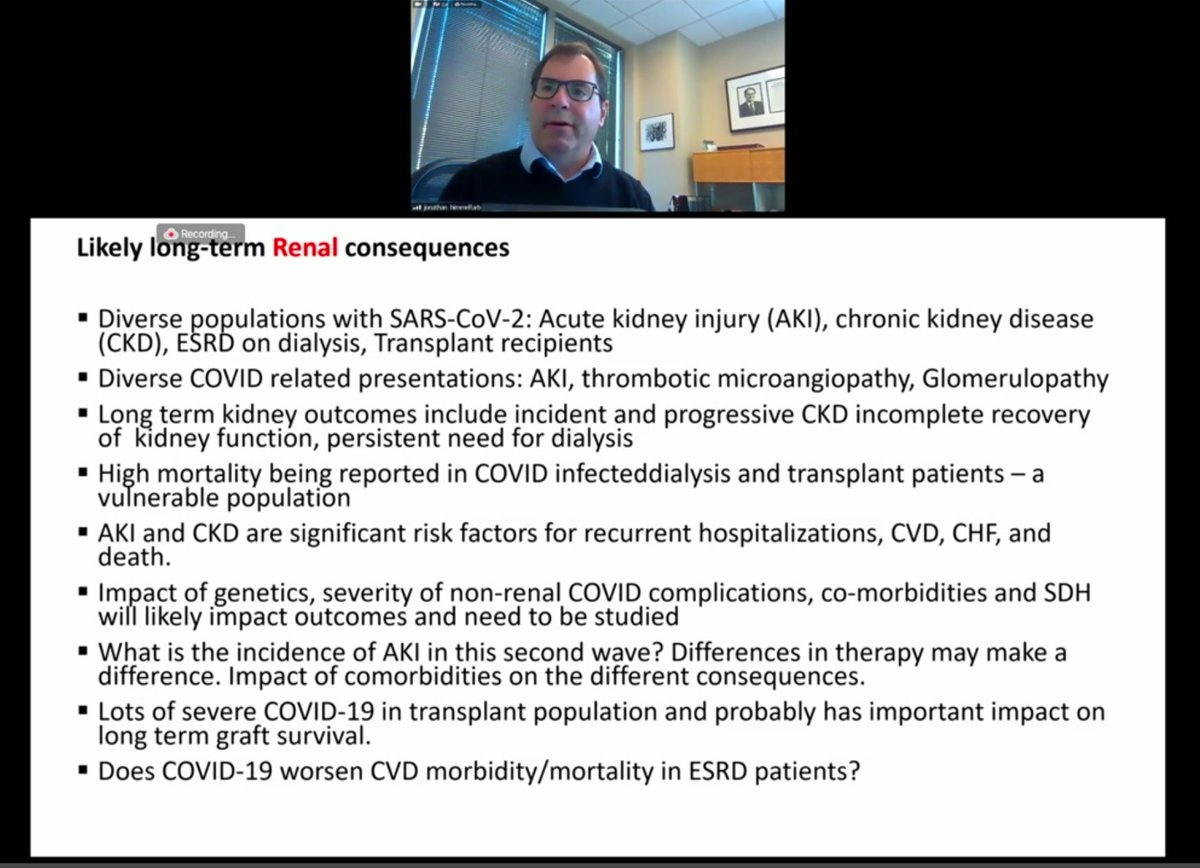
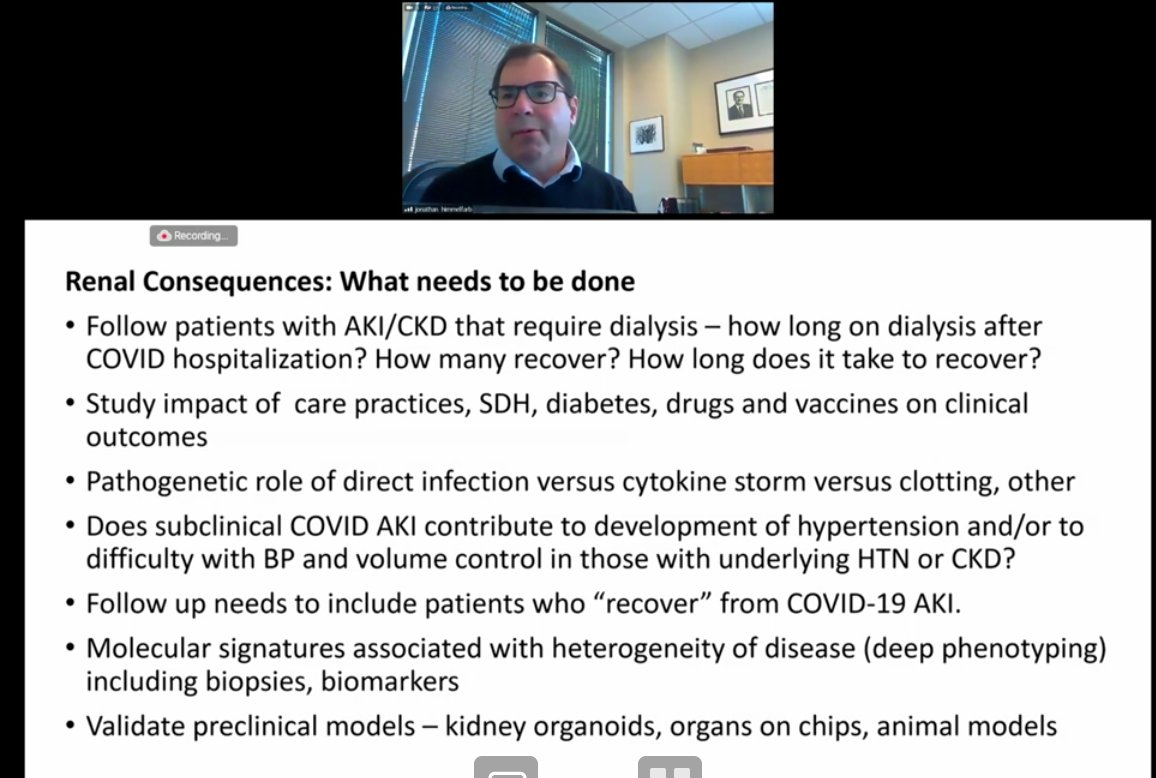
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid:
- Renal consequences: what needs to be done
(Slide with text bullet points on this)
- Renal consequences: what needs to be done
(Slide with text bullet points on this)
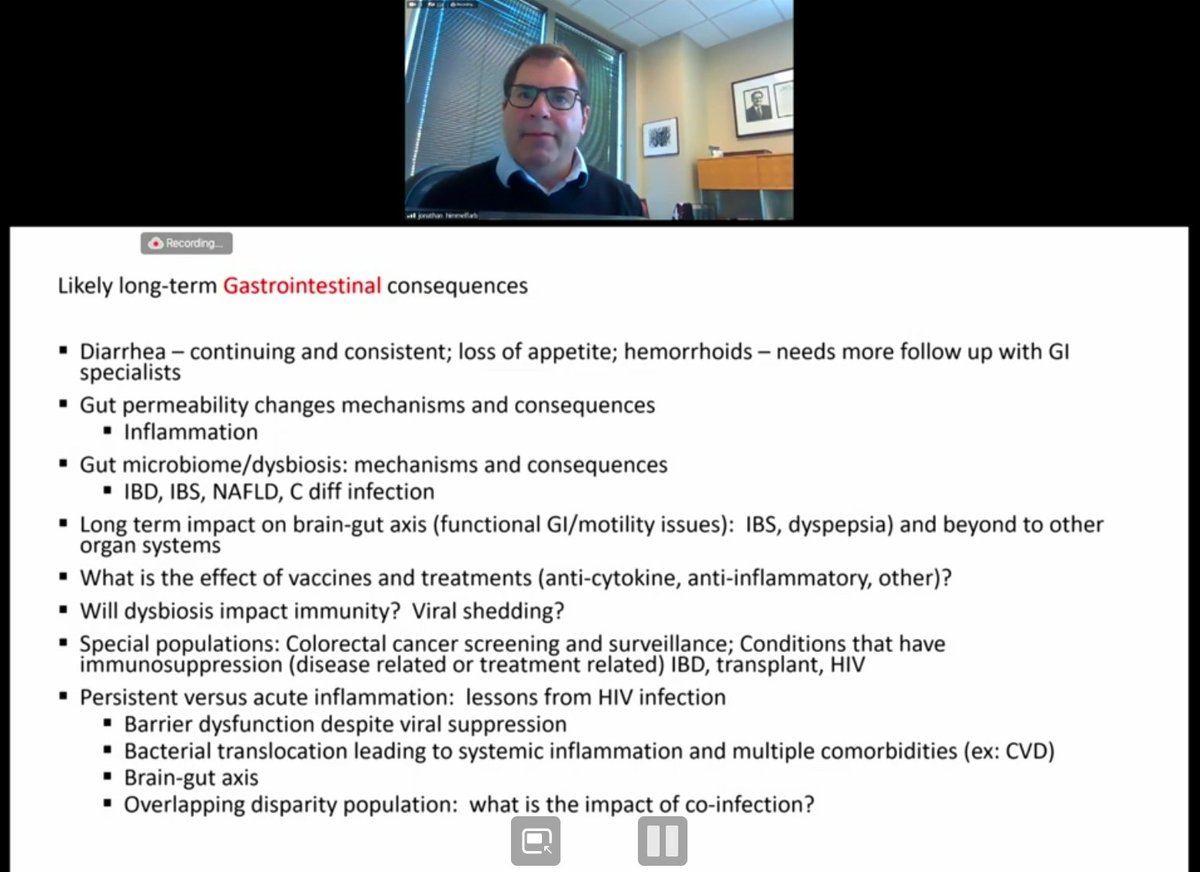
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid:
- Long-term gastrointestinal consequences
- diarrhea, gut permeability changes
- gut microbiome/dysbiosis
- viral shedding in GI tract. how will that impact on population basis as well as individuals?
- Long-term gastrointestinal consequences
- diarrhea, gut permeability changes
- gut microbiome/dysbiosis
- viral shedding in GI tract. how will that impact on population basis as well as individuals?
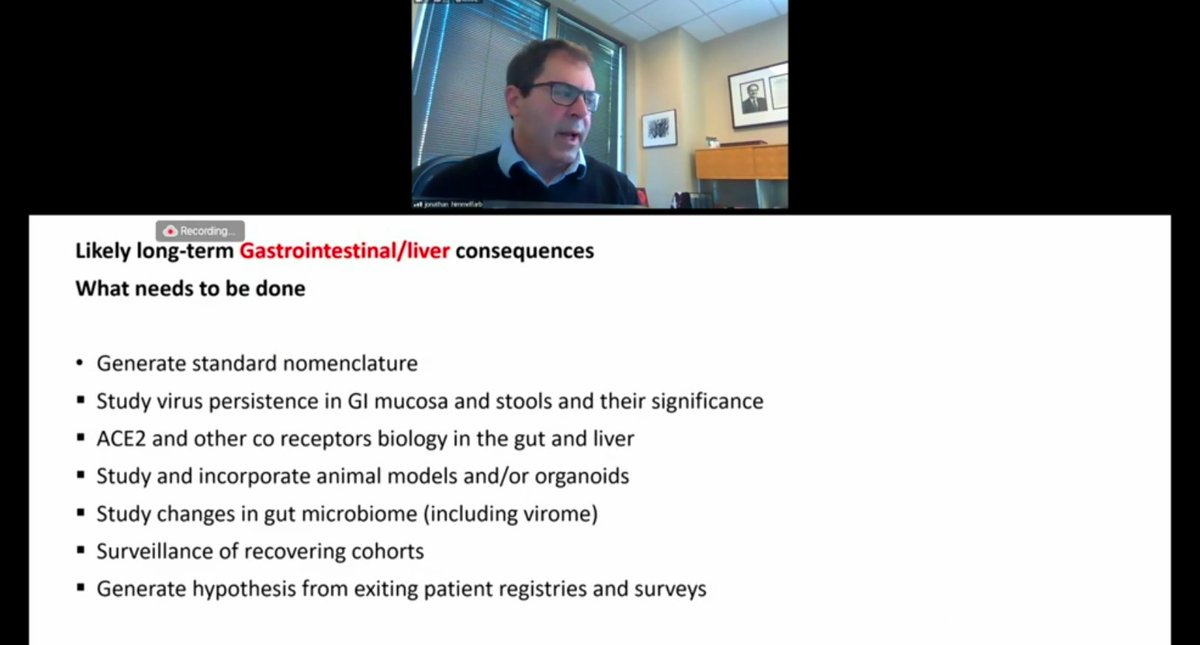
Dr. Jonathan Himmelfarb (UW) on GI of #LongCovid.
What needs to be done:
- we need to generate standard nomenclature.
- need to study viral persistence in GI mucosa and stools
- ACE2 receptors in gut and liver
- study changes in gut microbiome
- more on slide below
What needs to be done:
- we need to generate standard nomenclature.
- need to study viral persistence in GI mucosa and stools
- ACE2 receptors in gut and liver
- study changes in gut microbiome
- more on slide below
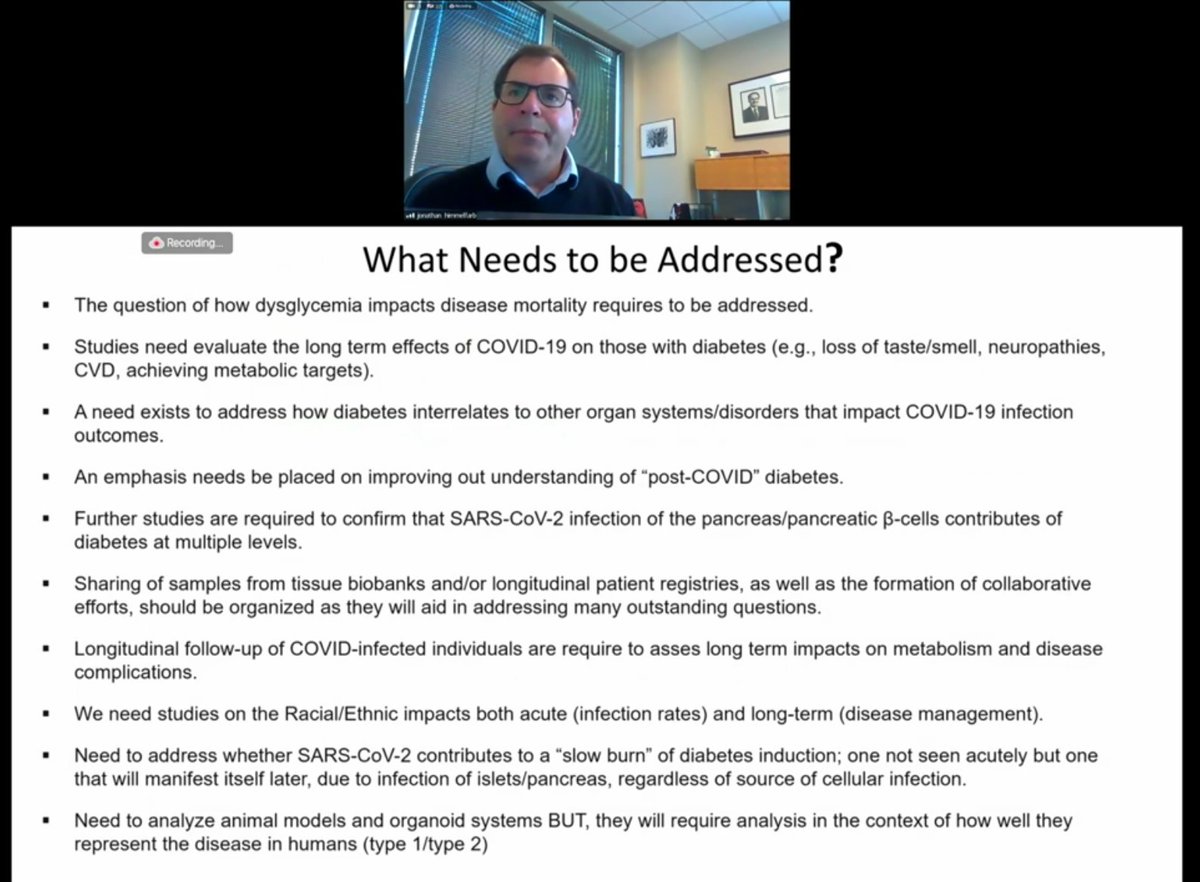
Dr. Jonathan Himmelfarb (UW) on metabolic of #LongCovid:
- #T1D and #T2D in relation to COVID
- In people without prior dx of Diabetes in #LongCovid, is it transitory? New syndrome?
- #T1D and #T2D in relation to COVID
- In people without prior dx of Diabetes in #LongCovid, is it transitory? New syndrome?

Dr. Jonathan Himmelfarb (UW) on metabolic of #LongCovid:
- will loss of taste/smell impact diabetes management in relation to diet?
- what needs to be addressed? Info below on slide (they are talking so fast; can't keep up)
- social determinants of health and racial impacts
- will loss of taste/smell impact diabetes management in relation to diet?
- what needs to be addressed? Info below on slide (they are talking so fast; can't keep up)
- social determinants of health and racial impacts
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid.
Cross cutting issues between GI+renal+ metabolic and other systems:
- role of social determinants of health
- need for a common vocab/nomenclature for #LongCovid
- pathogenesis: direct infection vs. inflammation
Cross cutting issues between GI+renal+ metabolic and other systems:
- role of social determinants of health
- need for a common vocab/nomenclature for #LongCovid
- pathogenesis: direct infection vs. inflammation

Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid.
Cross cutting issues between GI+renal+ metabolic and other systems:
- look to #HIV research as a model
- need rigorous multi-center data, hopefully including longitudinal follow-up to determine long term outcomes
Cross cutting issues between GI+renal+ metabolic and other systems:
- look to #HIV research as a model
- need rigorous multi-center data, hopefully including longitudinal follow-up to determine long term outcomes
Dr. Jonathan Himmelfarb (UW) on GI/renal/metabolic of #LongCovid.
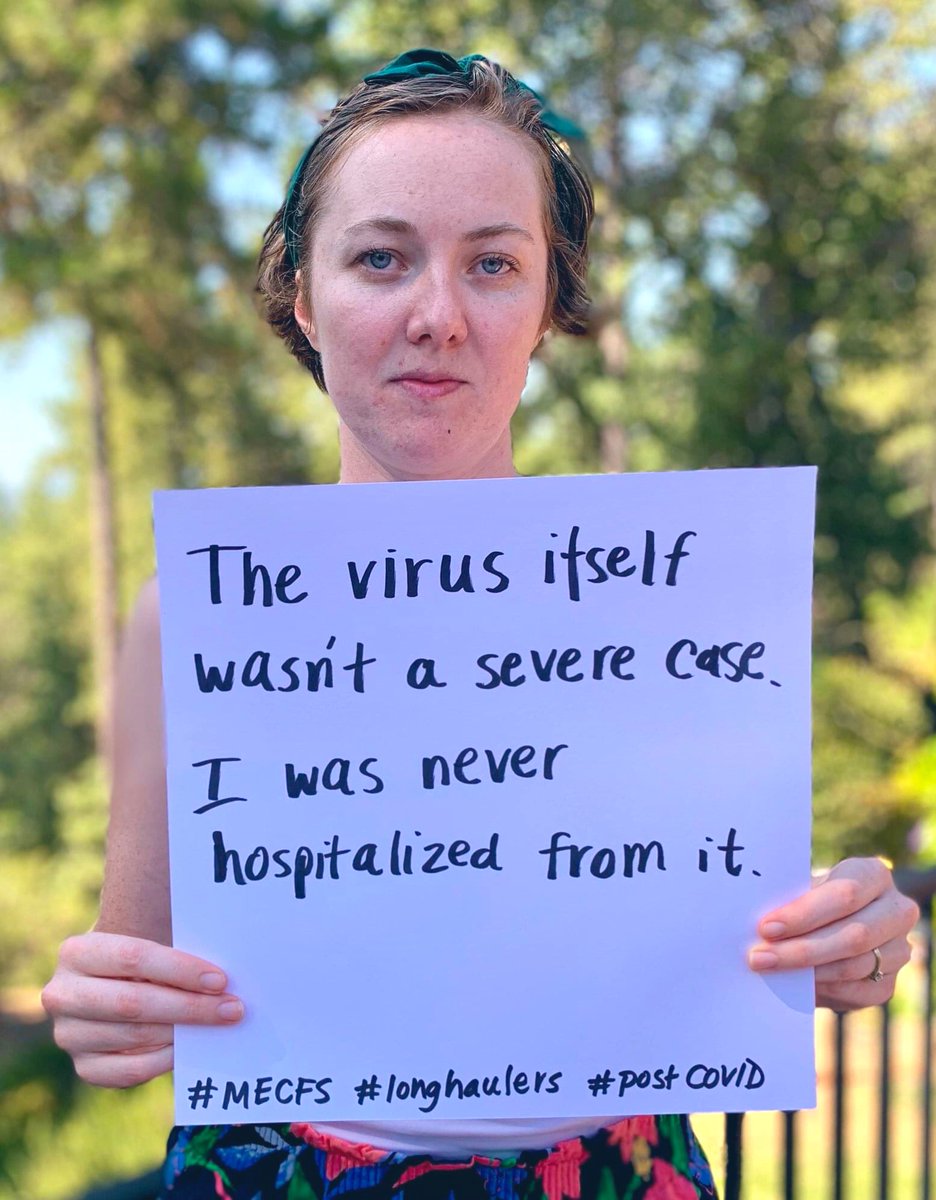
- false negatives are a problem. Lauren from @itsbodypolitic emphasized the testing barriers patients face and that clinical Dx should be considered for study eligibility even without positive test result
- false negatives are a problem. Lauren from @itsbodypolitic emphasized the testing barriers patients face and that clinical Dx should be considered for study eligibility even without positive test result
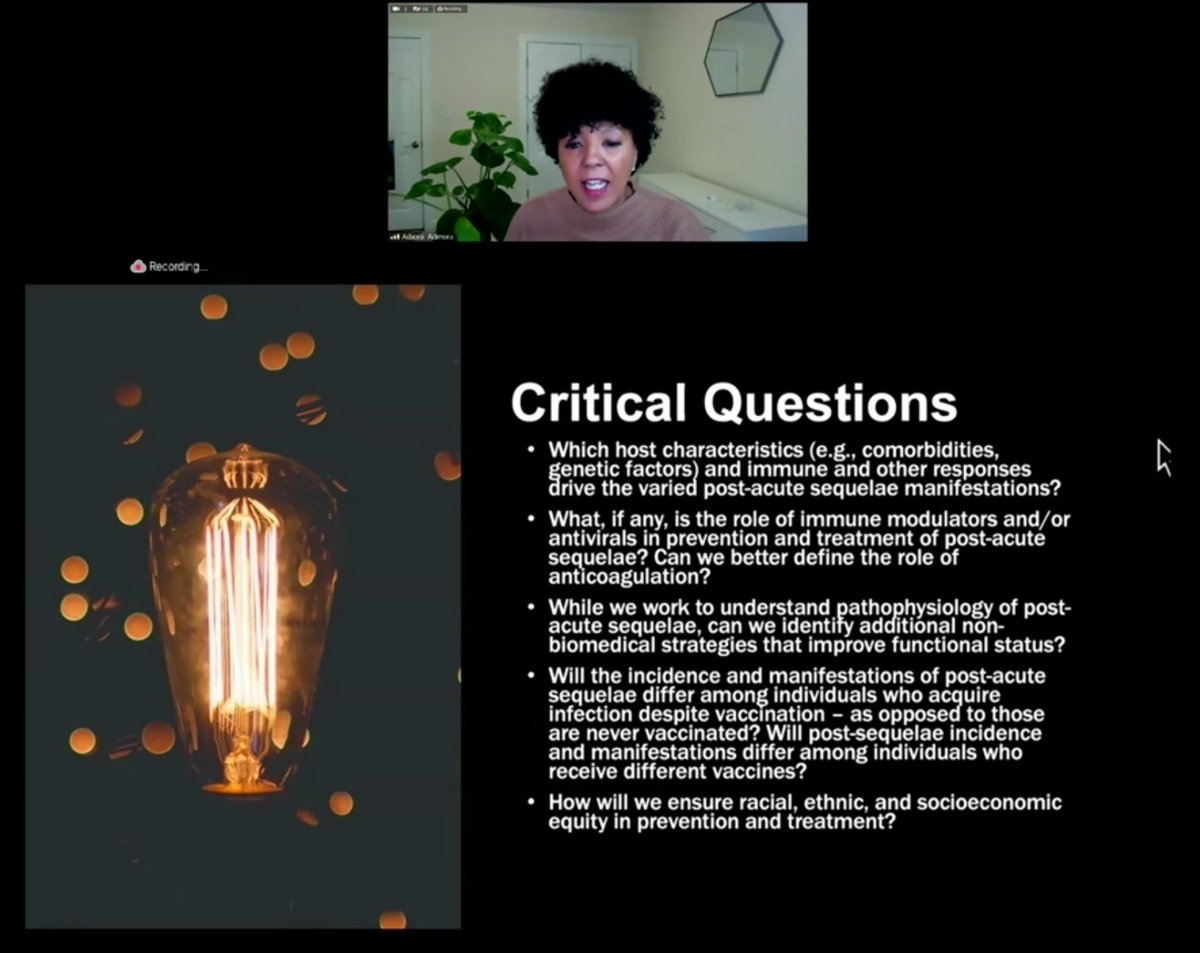
Immunologic/rheumatologic breakout group on #LongCovid:
- Dr. Rafi Ahmed (Emory) Director of Emory vaccine center
- Dr. Julie McElrath (Fred Hutch Cancer Research Center)
- Dr. Rafi Ahmed (Emory) Director of Emory vaccine center
- Dr. Julie McElrath (Fred Hutch Cancer Research Center)
Immunologic/rheumatologic breakout group #LongCovid:
- prospective cohorts are needed. Starting from the beginning would be helpful. Ideally study persons at risk prior to infection to establish baseline parameters
- What are key clinical signs & symptoms? Need expert team on it
- prospective cohorts are needed. Starting from the beginning would be helpful. Ideally study persons at risk prior to infection to establish baseline parameters
- What are key clinical signs & symptoms? Need expert team on it
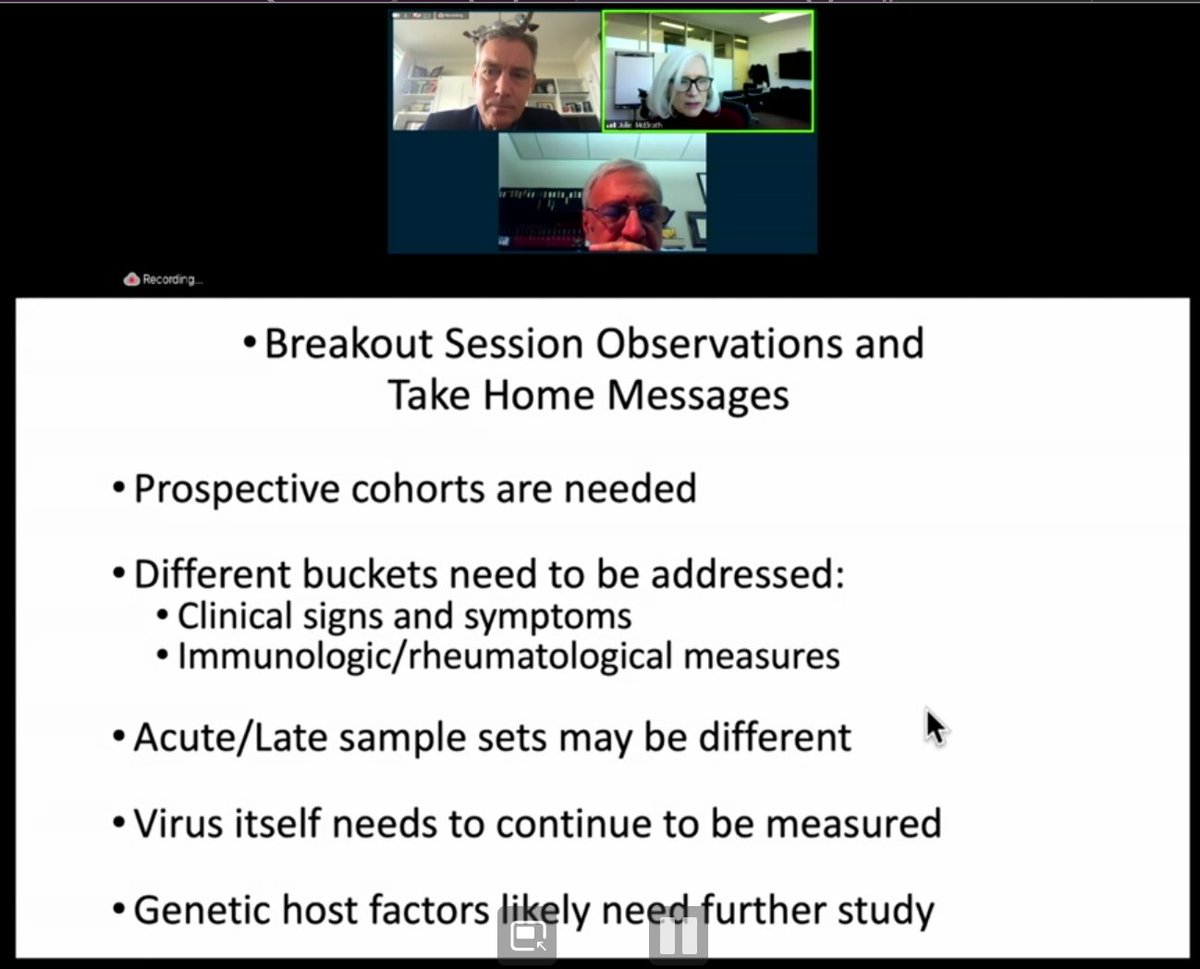
Immunologic/rheumatologic breakout group on #LongCovid:
- Different group should work on immunologic and rheum paramaters to define the very critical measures you would want to know from beginning to end. How should they be analyzed? Immediate/fresh or archived sample?
- Different group should work on immunologic and rheum paramaters to define the very critical measures you would want to know from beginning to end. How should they be analyzed? Immediate/fresh or archived sample?
Immunologic/rheumatologic breakout group on #LongCovid:
- There may be different components examined acutely vs. later on. Emphasis on importance of innate immune response as potentially shaping the disease course of COVID over time, in addition to adaptive immune response
- There may be different components examined acutely vs. later on. Emphasis on importance of innate immune response as potentially shaping the disease course of COVID over time, in addition to adaptive immune response
Immunologic/rheumatologic breakout group on #LongCovid:
- The importance of continuing to measure the virus. Nasal PCR, saliva, stool –– where is virus persisting? What is impact of that persistence on #LongCovid?
- what genetic factors might be relevant?
- The importance of continuing to measure the virus. Nasal PCR, saliva, stool –– where is virus persisting? What is impact of that persistence on #LongCovid?
- what genetic factors might be relevant?
Immunologic/rheumatologic breakout group on #LongCovid:
- Perhaps piggyback on studies already happening and funded with large number of people (like vaccine studies)
- third to half of participants in those studies are placebo. Consider nesting in prospective studies in those
- Perhaps piggyback on studies already happening and funded with large number of people (like vaccine studies)
- third to half of participants in those studies are placebo. Consider nesting in prospective studies in those
Immunologic/rheumatologic breakout group on #LongCovid:
- there are also prophylaxis clinical trials. consider piggybacking on those bc clinical record will be there and sample will be stored. This may be efficient and cost saving way to answer some of research questions here.
- there are also prophylaxis clinical trials. consider piggybacking on those bc clinical record will be there and sample will be stored. This may be efficient and cost saving way to answer some of research questions here.
Immunologic/rheumatologic breakout group on #LongCovid:
- there are other viruses with late sequelae; look to those to help us understand this. EBV, CMV, RSV have info we could be thinking about in the setting of designing these potential cohort analyses
- there are other viruses with late sequelae; look to those to help us understand this. EBV, CMV, RSV have info we could be thinking about in the setting of designing these potential cohort analyses
Immunologic/rheumatologic breakout group on #LongCovid:
- need to engage patient advocacy groups, especially those that would help them include diverse patients. + knowledge advocacy groups have gained with their respective diseases in framing clinical questions and assessments
- need to engage patient advocacy groups, especially those that would help them include diverse patients. + knowledge advocacy groups have gained with their respective diseases in framing clinical questions and assessments
Immunologic/rheumatologic breakout group on #LongCovid:
- what kind of samples should be collected from individuals? Particularly blood. Vaccine placebo group could be important there bc they have blood sample from before COVID, that could be compared to after infection
- what kind of samples should be collected from individuals? Particularly blood. Vaccine placebo group could be important there bc they have blood sample from before COVID, that could be compared to after infection
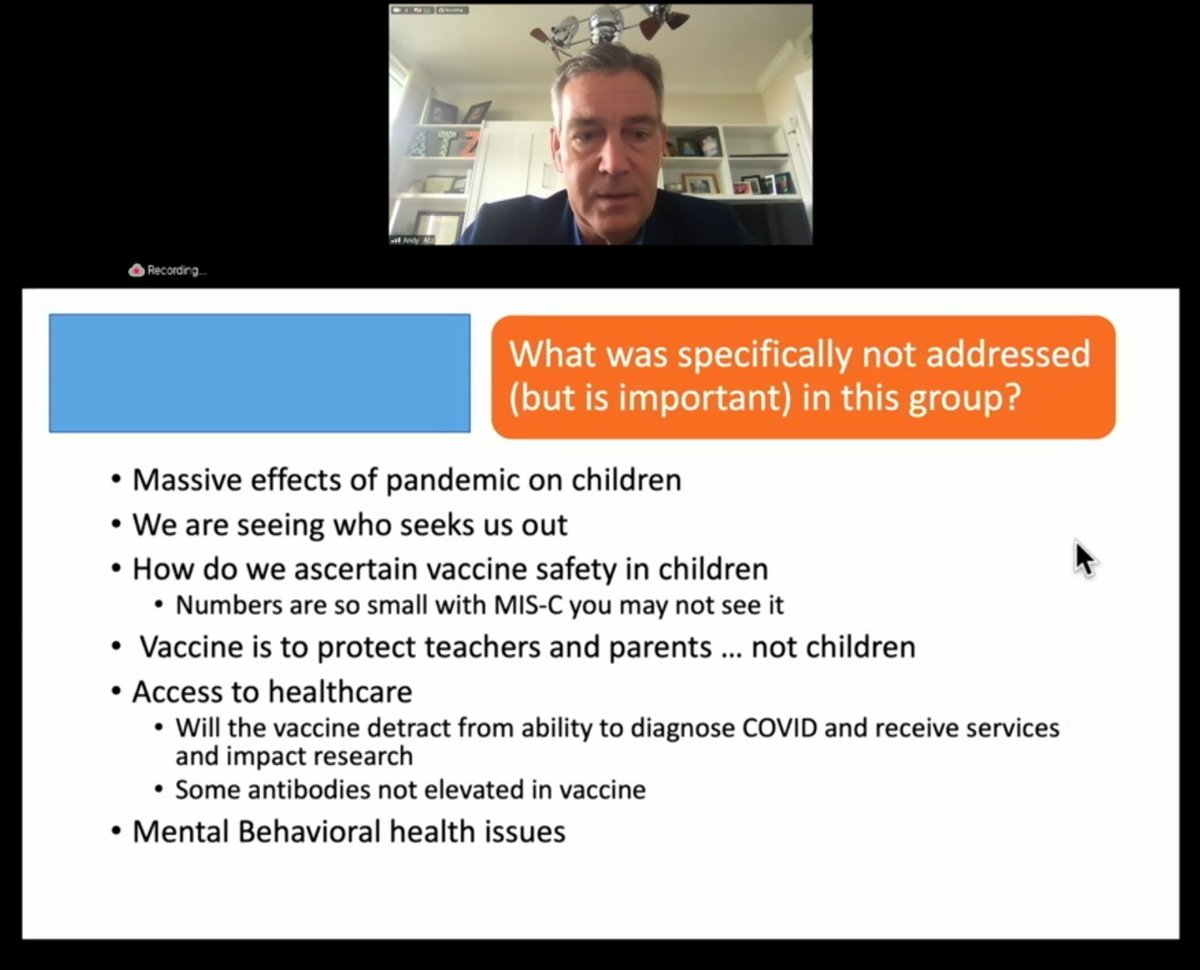
Pediatric breakout group on #LongCovid led by Dr. Andrew Atz, pediatric cardiologist (MUSC):
- 20 people participated: pediatricians, critical care, cardiologists, pulmonary, physical med rehab, ME/CFS.
- a homework joke bc pediatricians (lol)
- preferred #LongCovid as name
- 20 people participated: pediatricians, critical care, cardiologists, pulmonary, physical med rehab, ME/CFS.
- a homework joke bc pediatricians (lol)
- preferred #LongCovid as name

Pediatric breakout group on #LongCovid:
- Observational long term studies. (MUSIC, PRISM, NeuroCOVID, OVERCOMING COVID are several happening now)
- He says #LongCovid probably doesn't even start until first month
- How do we assess for quality of life, functional disability
- Observational long term studies. (MUSIC, PRISM, NeuroCOVID, OVERCOMING COVID are several happening now)
- He says #LongCovid probably doesn't even start until first month
- How do we assess for quality of life, functional disability
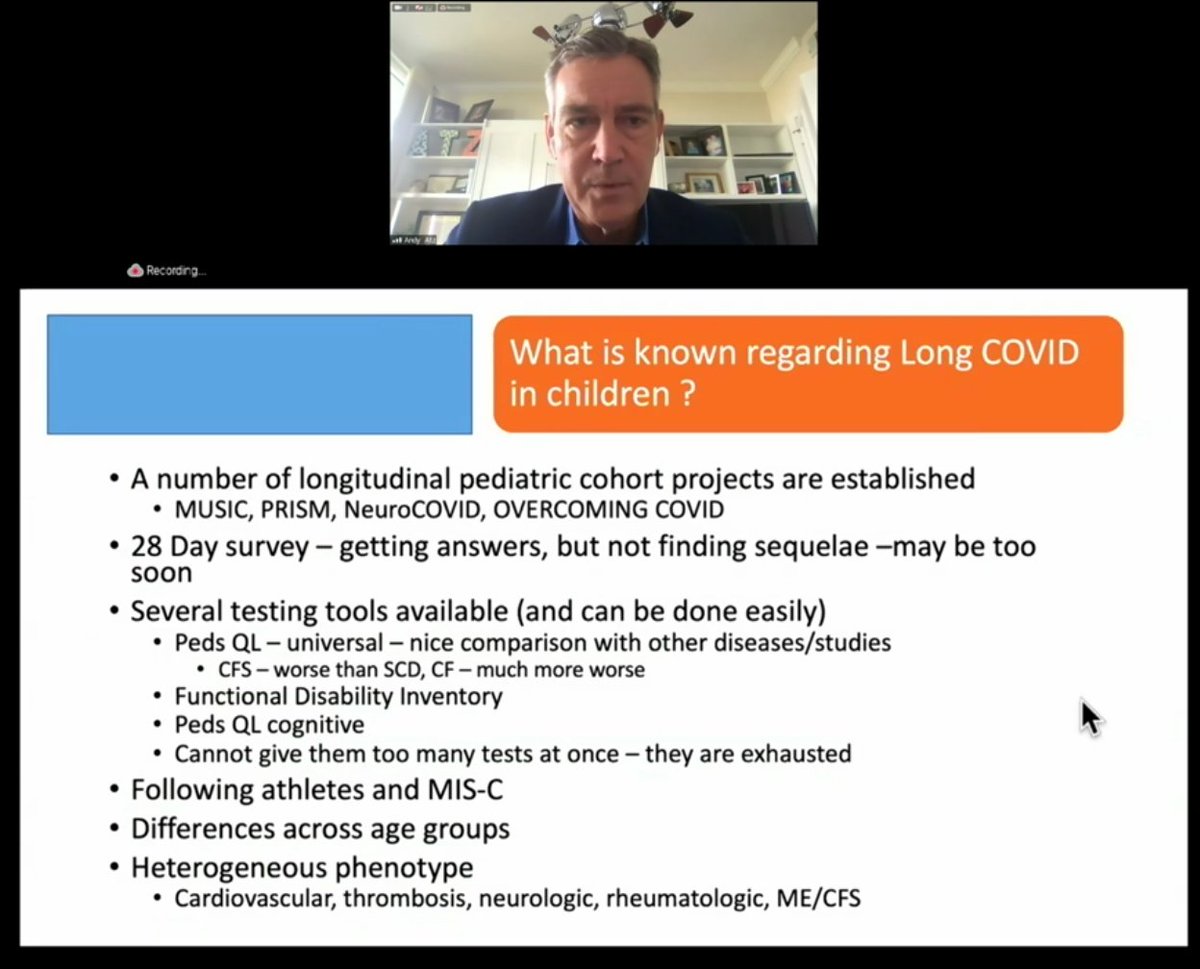
Pediatric breakout group:
(same slide as above)
- On MIS-C: we may learn more about #LongCovid from these studies
- Differences across age groups across pediatric spectrum. Adolescents perform like adults; young children have different immunobiology makeup and are different
(same slide as above)
- On MIS-C: we may learn more about #LongCovid from these studies
- Differences across age groups across pediatric spectrum. Adolescents perform like adults; young children have different immunobiology makeup and are different

Pediatric breakout group on #LongCovid:
- different phenotypes (#MECFS, brain fog, #dysautonomia mentioned here)
New slide below
- gaps in testing that will pose a research challenge for #LongCovid
- what questions should they ask? Ped patients often can't speak for themselves
- different phenotypes (#MECFS, brain fog, #dysautonomia mentioned here)
New slide below
- gaps in testing that will pose a research challenge for #LongCovid
- what questions should they ask? Ped patients often can't speak for themselves
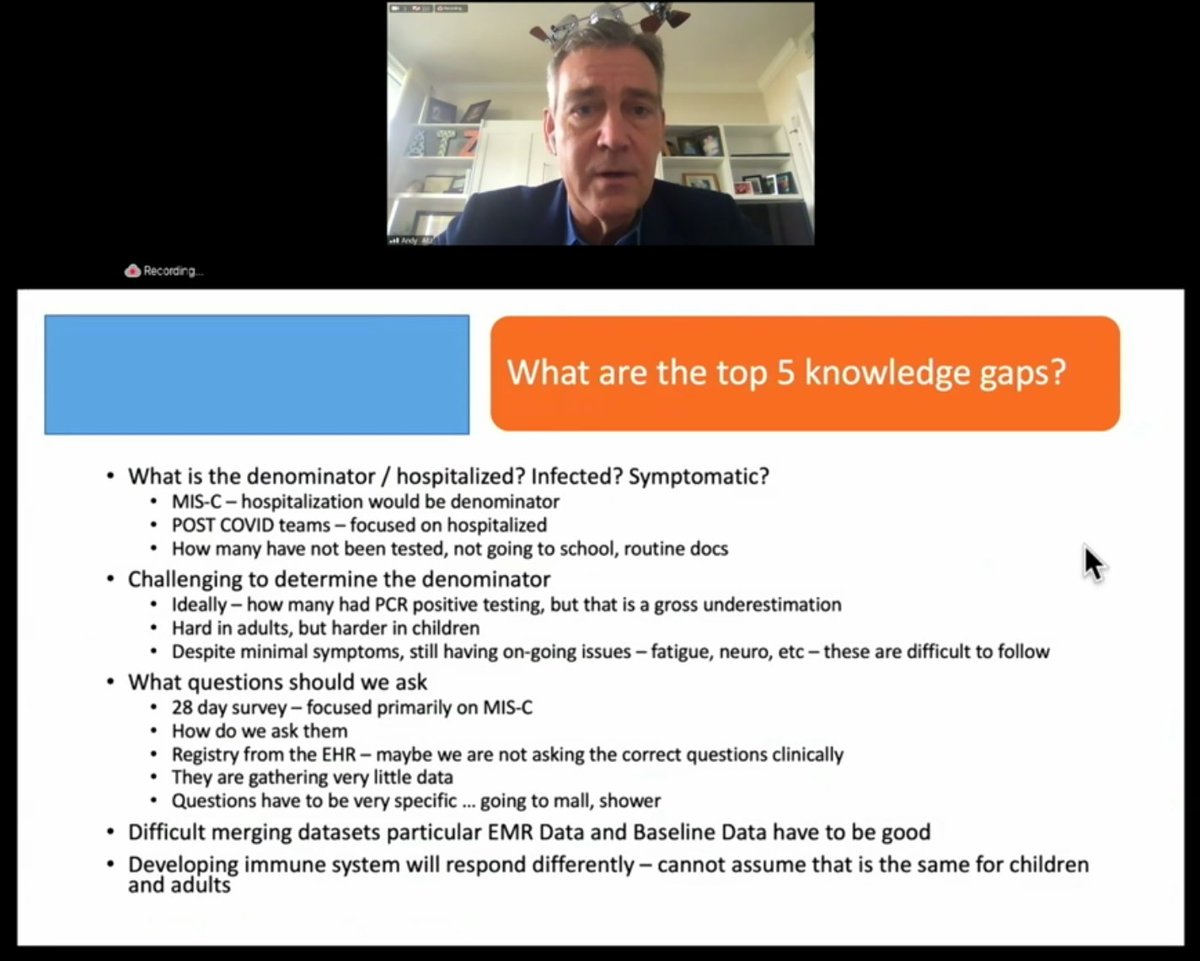
Pediatric breakout group on #LongCovid:
- If we wait for EMR studies, it will take a long time before these systems to talk to each other. We need to move faster than what that can do.
- If we wait for EMR studies, it will take a long time before these systems to talk to each other. We need to move faster than what that can do.
Pediatric breakout group on #LongCovid:
- there needs to be well-recognized neurocognitive outcomes. Can we repurpose from other areas?
- They think #LongCovid symptoms in children are rarer than in adults, but need case controls to analyze for accurate data
- there needs to be well-recognized neurocognitive outcomes. Can we repurpose from other areas?
- They think #LongCovid symptoms in children are rarer than in adults, but need case controls to analyze for accurate data
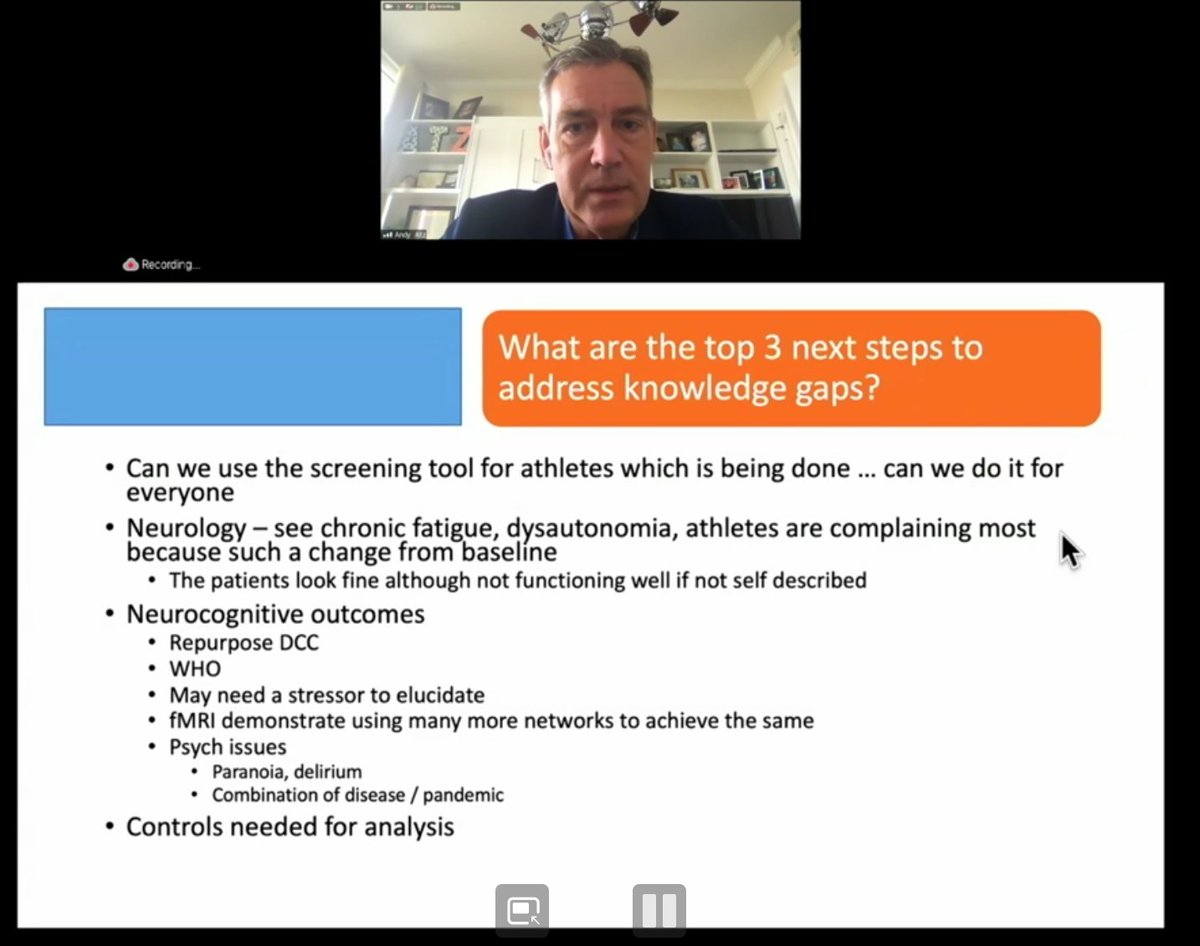
Pediatric breakout group on #LongCovid:
- Children "still live in the same unfortunate aspect that their zipcode determines more than their genetic code."
- Children needing to be hospitalized may face barriers depending on location
- Children "still live in the same unfortunate aspect that their zipcode determines more than their genetic code."
- Children needing to be hospitalized may face barriers depending on location

Pediatric breakout group on #LongCovid:
- allocation of resources is mismatched. Dr. Peter Rowe is only pediatric #MECFS specialist in the country
- allocation of resources is mismatched. Dr. Peter Rowe is only pediatric #MECFS specialist in the country
Pediatric breakout group on #LongCovid:
- pandemic is impacting children significantly outside of #LongCovid
- how to separate #LongCovid from other challenges children face with pandemic impacts
- pandemic is impacting children significantly outside of #LongCovid
- how to separate #LongCovid from other challenges children face with pandemic impacts
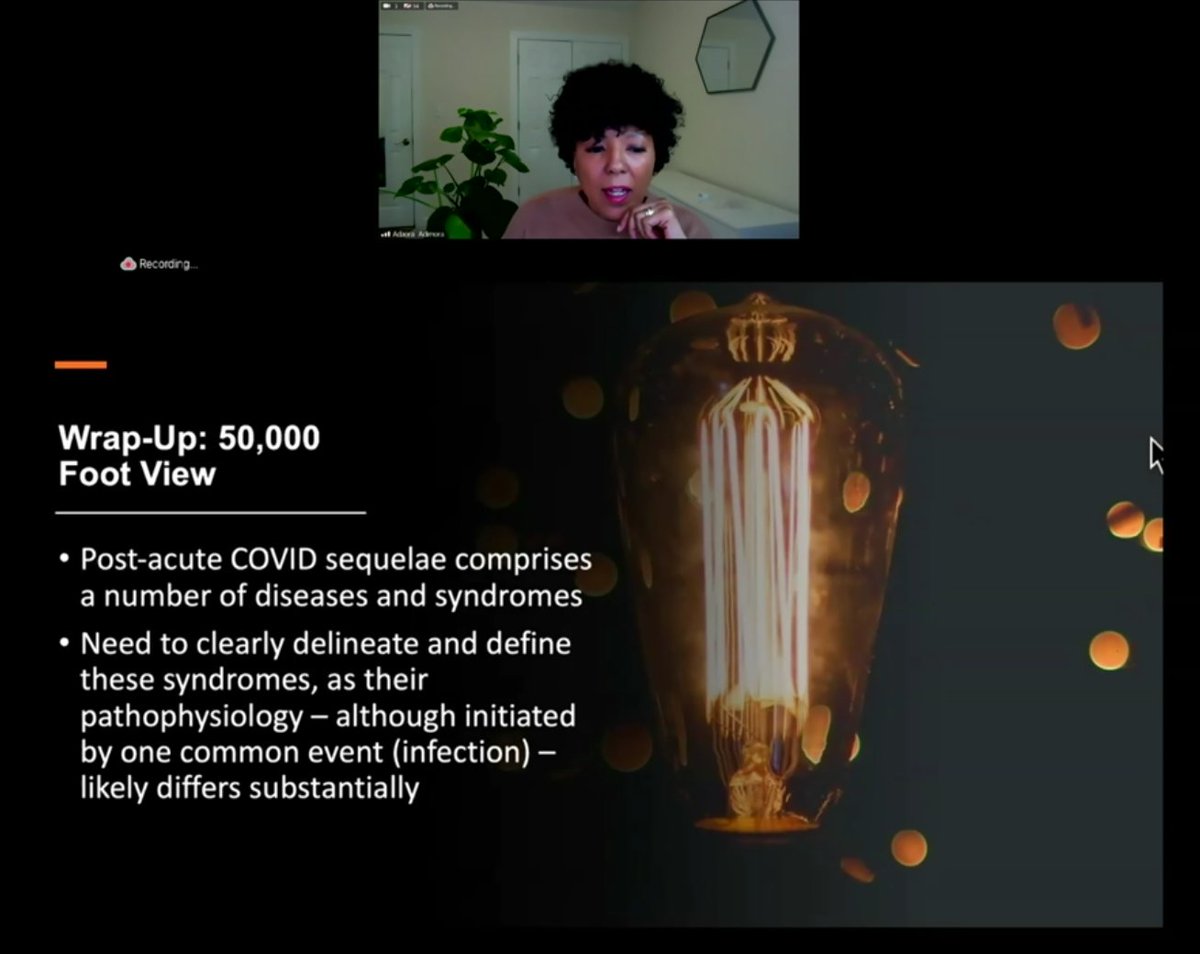
Summary of @NIH workshop on #LongCovid today:
- #LongCovid is an opportunity to learn about post-infectious sequelae (paging #MECFS & #PwME)
- need multidisciplinary, integrated care
- must engage at-risk communities to communicate risk of #LongCovid (thanks @chiluvs1 for this)
- #LongCovid is an opportunity to learn about post-infectious sequelae (paging #MECFS & #PwME)
- need multidisciplinary, integrated care
- must engage at-risk communities to communicate risk of #LongCovid (thanks @chiluvs1 for this)
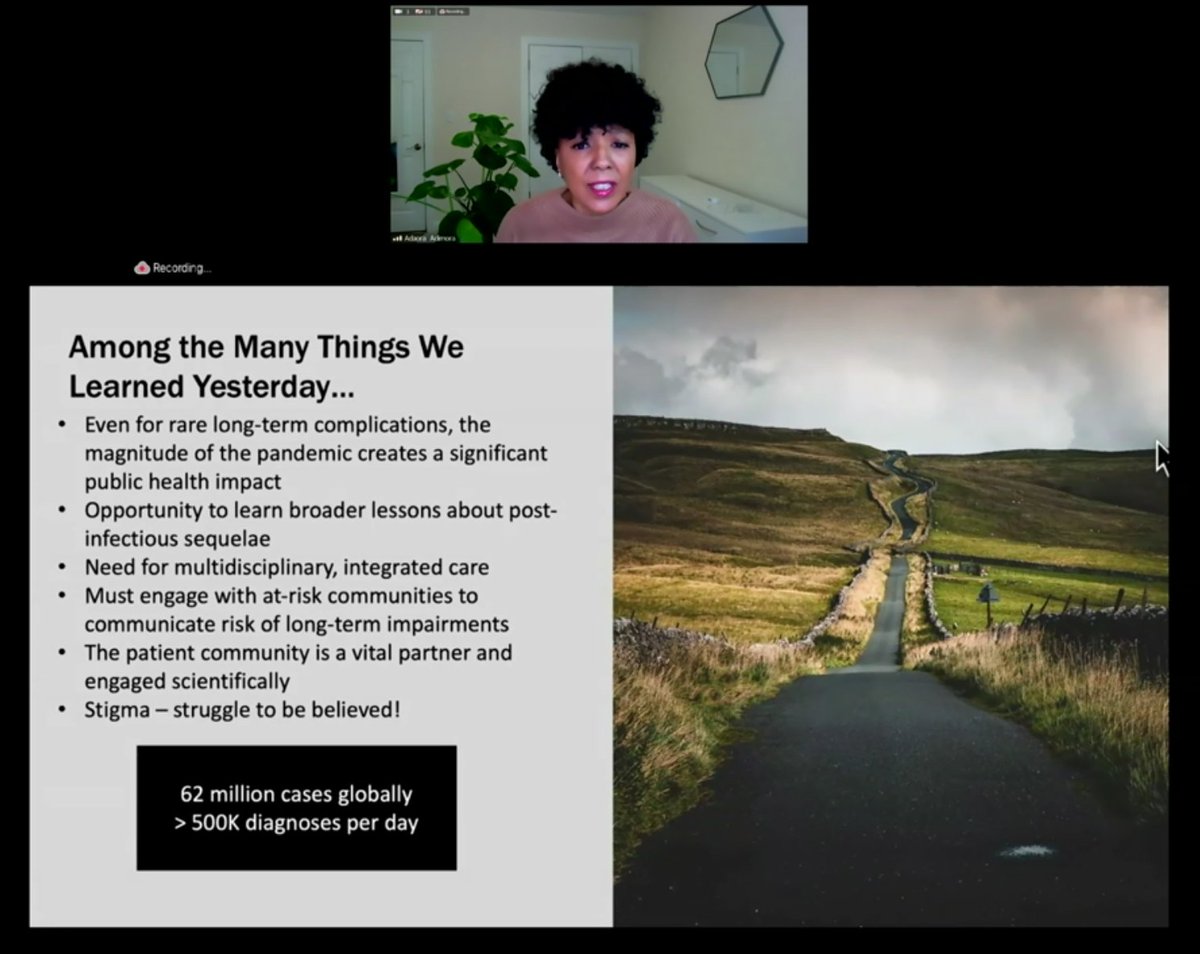
Summary of @NIH workshop on #LongCovid today.
What are the best strategies for research on #LongCovid?
What are the best strategies for research on #LongCovid?

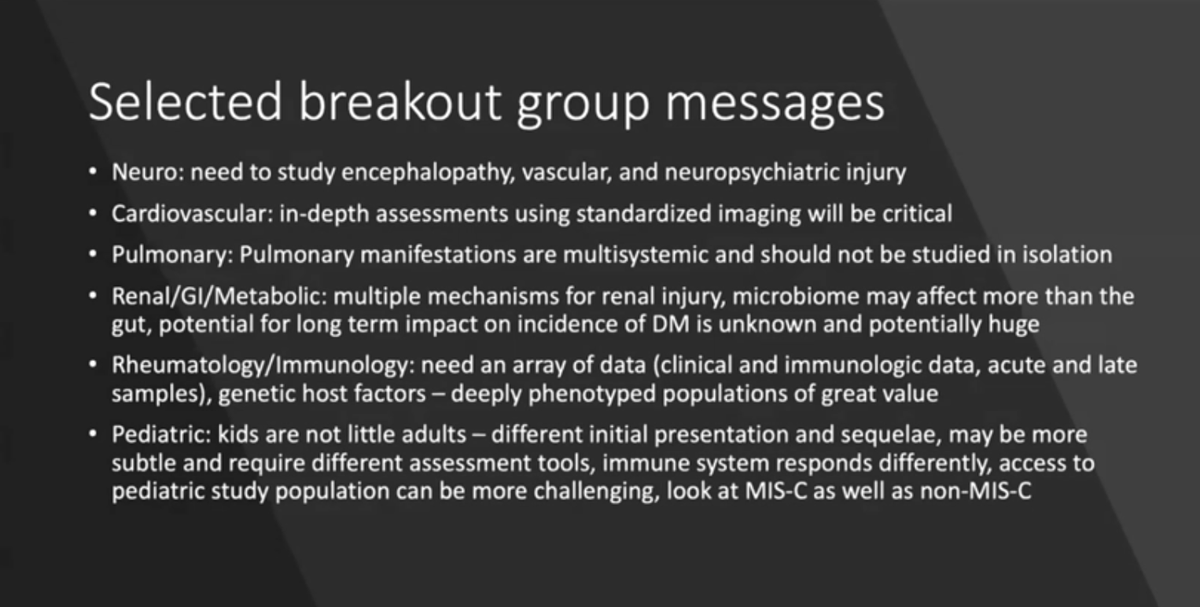
Summary of @NIH workshop on #LongCovid today, of breakout group sessions. (I have more details on these above.) 
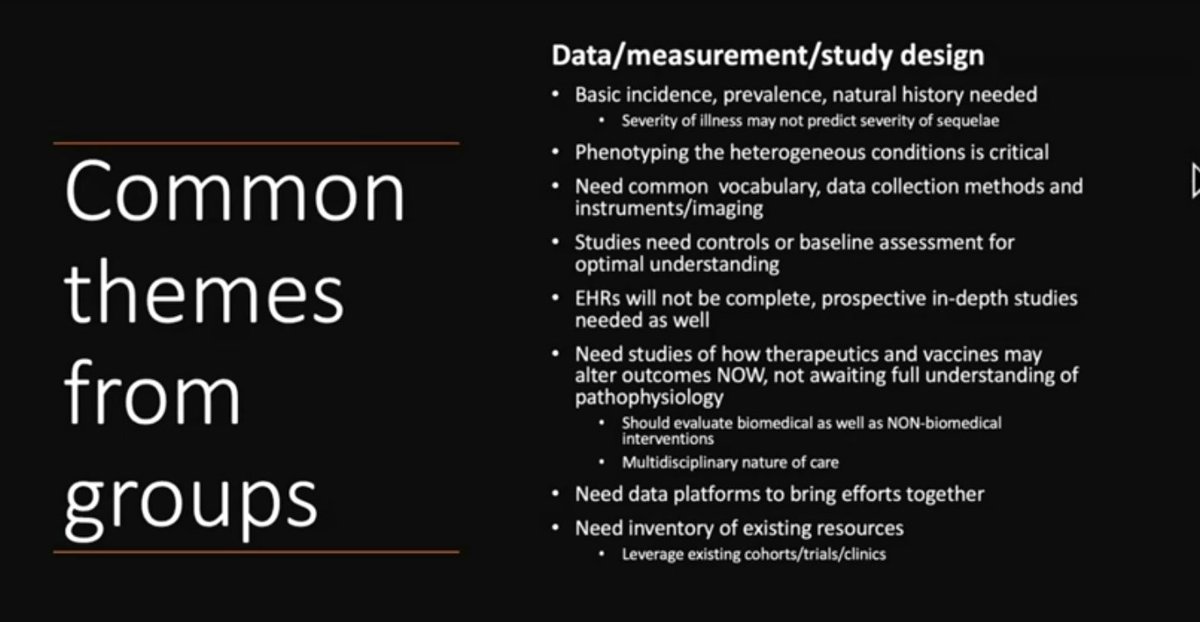
Summary of @NIH workshop on #LongCovid today. Common themes from breakout groups on data, measurement and study design. 
Summary of @NIH workshop on #LongCovid today: next steps. They will compile gaps identified from the workshop and work with @CDCgov @WHO and other stakeholders (may I suggest @itsbodypolitic ?) to come to consensus on how to define this and collaborate going forward. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh