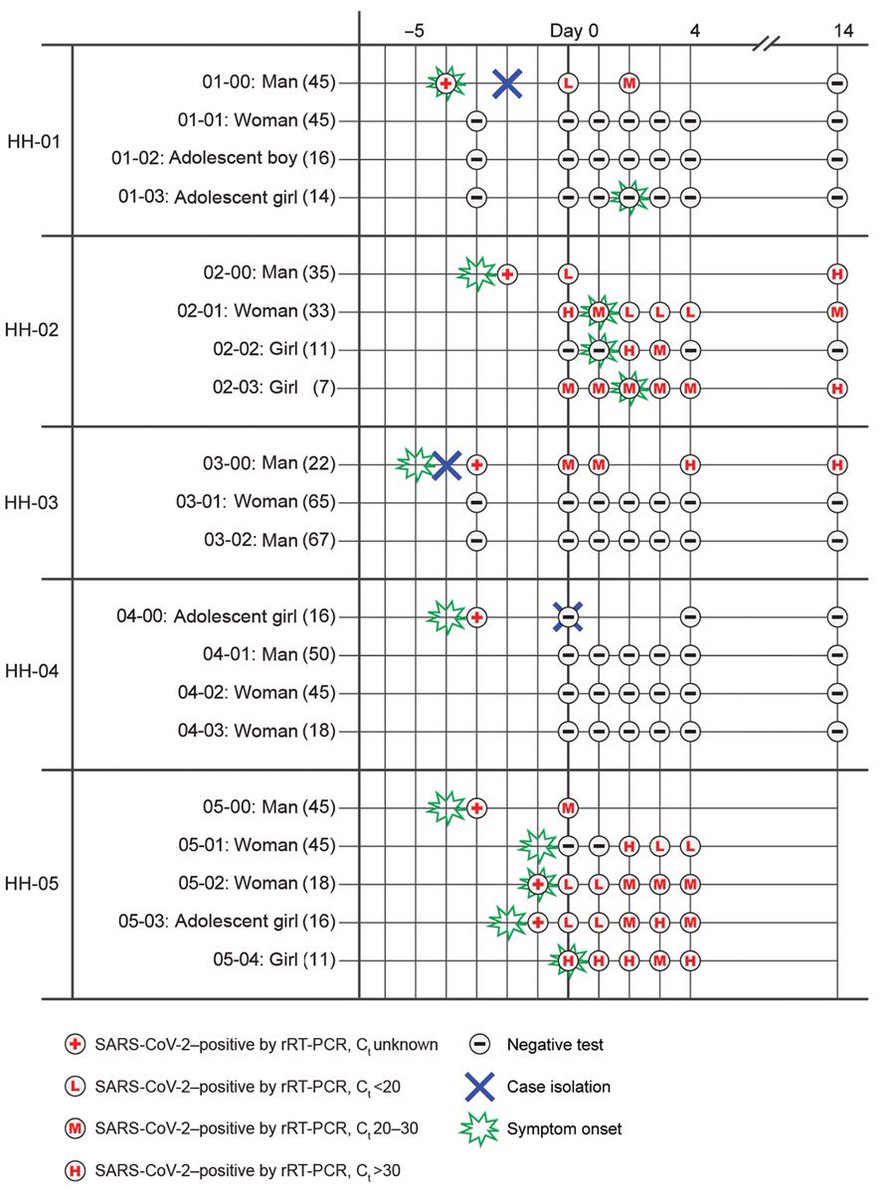
The latest round of random testing in the UK shows both children and teenagers are now more likely to be infected than adults.
1 in 48 teenagers and 1 in 58 children tested positive.
Infections are decreasing in adults, but increasing in children.
Red bar = most recent round.
1 in 48 teenagers and 1 in 58 children tested positive.
Infections are decreasing in adults, but increasing in children.
Red bar = most recent round.
The proportion of people testing positive by age group is as follows:
5-12: 1.7%
13-17: 2.1%
18-24: 1.0%
25-34: 1.0%
35-44: 0.8%
45-54: 0.8%
55-64: 0.7%
65+: 0.4%
5-12: 1.7%
13-17: 2.1%
18-24: 1.0%
25-34: 1.0%
35-44: 0.8%
45-54: 0.8%
55-64: 0.7%
65+: 0.4%
In the accompanying media release the researchers note cases are no longer decreasing overall and:
“School-age children are ... the most affected age group, which could be linked to schools remaining open during lockdown.”
Link to media release & report: imperial.ac.uk/news/210873/co…
“School-age children are ... the most affected age group, which could be linked to schools remaining open during lockdown.”
Link to media release & report: imperial.ac.uk/news/210873/co…
Addendum: these data are for England, rather than the UK as a whole.
People living in Scotland, Wales, and Northern Ireland are not tested as part of this study.
People living in Scotland, Wales, and Northern Ireland are not tested as part of this study.
• • •
Missing some Tweet in this thread? You can try to
force a refresh