Thread on interconnected #bioethics problems in #COVID19 vaccine allocation: (1) the Stanford med center allocation debacle, (2) Rupert Murdoch, and (3) high-profile calls for age-only (“oldest first”) allocation policies. If you like (3), unfortunately you get (1) and (2). 1/7
People are right to be upset w/Stanford: see @CarolineYLChen excellent piece
https://twitter.com/CarolineYLChen/status/1340046920631394310?s=20. But it’s not “algorithms”, it’s inputs. If your inputs are too simplistic (age-only, ignore exposure or medical risk), you get bad outcomes, e.g. no residents, senior WFH 1st 2/7
Same w/ Murdoch:
https://twitter.com/archiebland/status/1339943158961074177?s=20. People are right to be upset. But age-only priority like the UK (start w/85+ or 90+), ends up prioritizing Murdoch over a 60 yo bus driver. Who lives to 90? We know the answer: more often, wealthier people. Need to consider other risk 3/7
What’s the answer here? 3 things. Policies must grapple with conflicts between important aims (exposure risk vs. risk if infected). They need “granularity”-multiple principles, not age-only—to be ethically plausible
https://twitter.com/DrTomFrieden/status/1340131768217825287?s=20. And they need to be transparent. 4/7
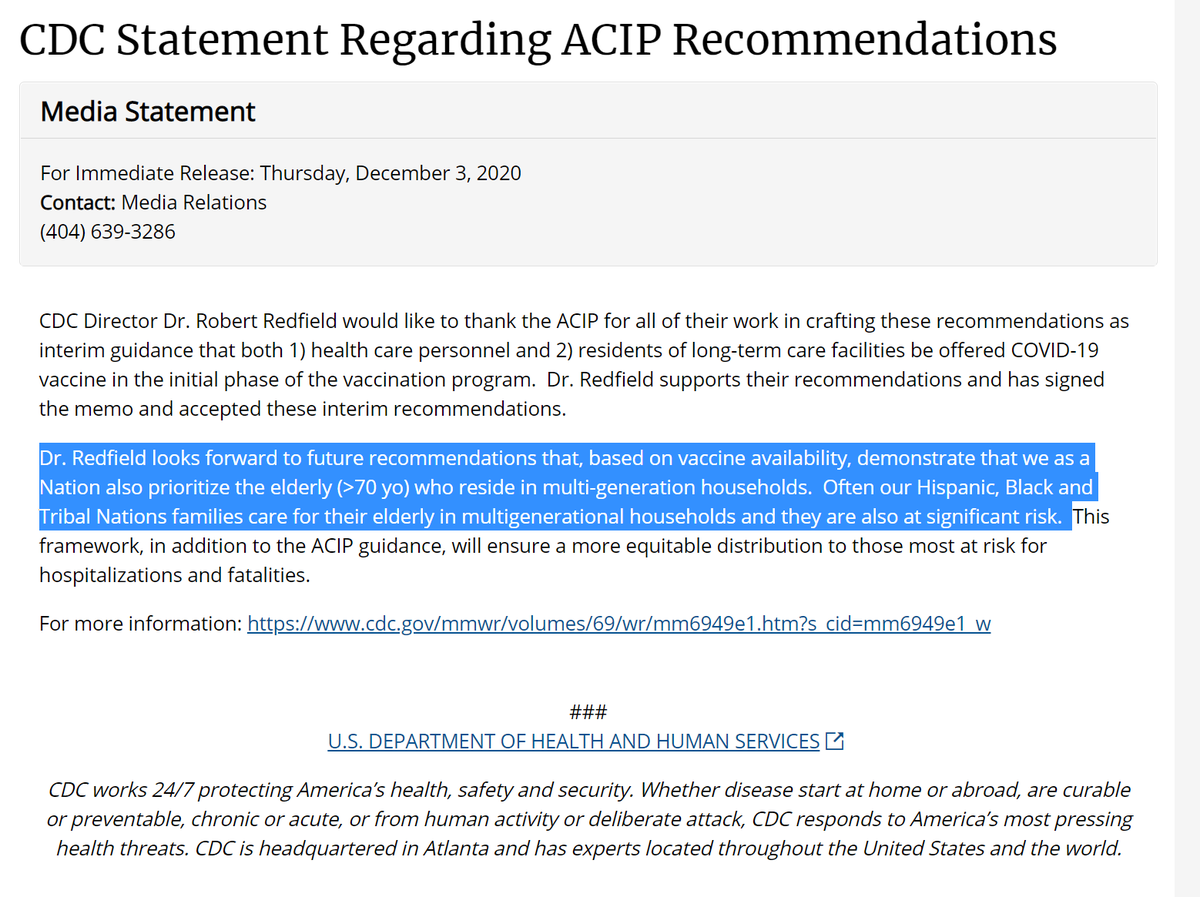
Ethically tenable policies would consider OVERLAPPING risks as @TomFrieden argues. Age+frontline. Age+congregate housing (as the LTCF priority is already doing and @CDCDirector called for cdc.gov/media/releases…). Frontline worker+medical vulnerability. Frontline+SVI/poverty. 5/7
So I disagree w/ enthusiasm for age-only, oldest-first from @mattyglesias @NateSilver538 & others. Especially given current, sensible long-term-care priority. I get worries about “gameability"/complexity. But 1 variable won't capture nuance of what people rightly care about. 6/7
A nice recent piece on different #bioethics values underlying phase 1A priority by @crane_johanna & others is here:
https://twitter.com/hastingscenter/status/1339332226572546050?s=20. This thread inspired by seeing posts from @CohenProf @nicholas_bagley @kelleher_ @WF_Parker, and ongoing collab w/@DrMonicaPeek . 7/7
Glad so many found the thread useful! Going to bed but a grumpy coda about the way critics (and sadly journalists) have generated uncessary drama here, plus a dash of hypocrisy:
https://twitter.com/GovindPersad/status/1340558539853447168?s=20
A bit more now that #ACIP released its updated thoughts - my concerns about age cutoffs vs. age-plus & overlapping risk still stands:
https://twitter.com/GovindPersad/status/1340710113187774465?s=208/7
• • •
Missing some Tweet in this thread? You can try to
force a refresh