This is an *excellent* piece by @math_rachel talking about the overlap of machine learning & medicine, & where it goes wrong, capturing such a wide range of issues.
This is required reading for ML folks, #MedTwitter, #LongCOVID, #NEISvoid, & everyone.
bostonreview.net/science-nature…
1/
This is required reading for ML folks, #MedTwitter, #LongCOVID, #NEISvoid, & everyone.
bostonreview.net/science-nature…
1/
It looks at flaws/biases in medical data (pulse oximeters are less accurate on POC, diagnoses of #EDS take 4 years for men but 16 YEARS for women), ML amplifies biases rather than counteracting them, algorithms that incorrectly cut health care with no method for recourse...
2/
2/
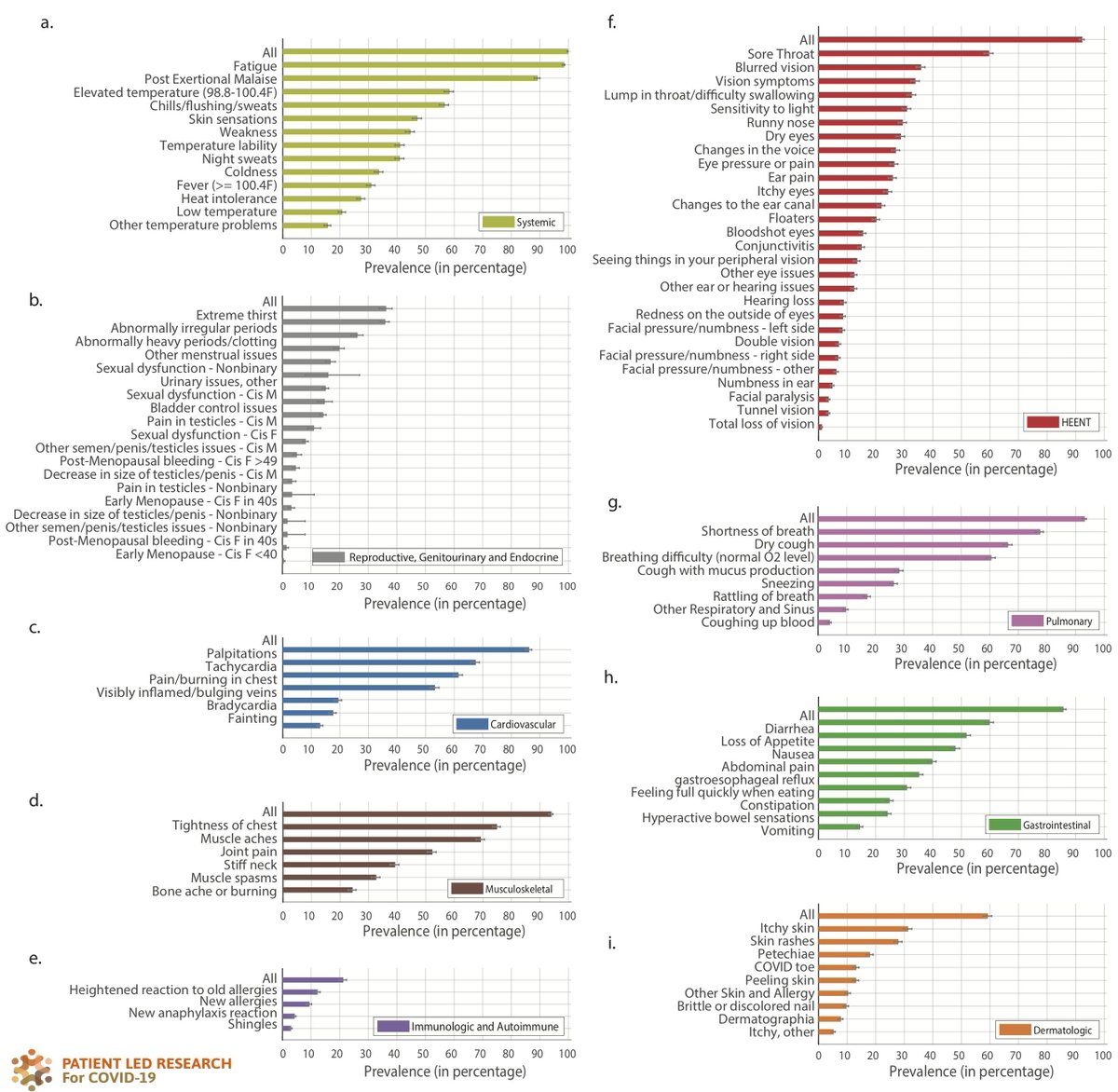
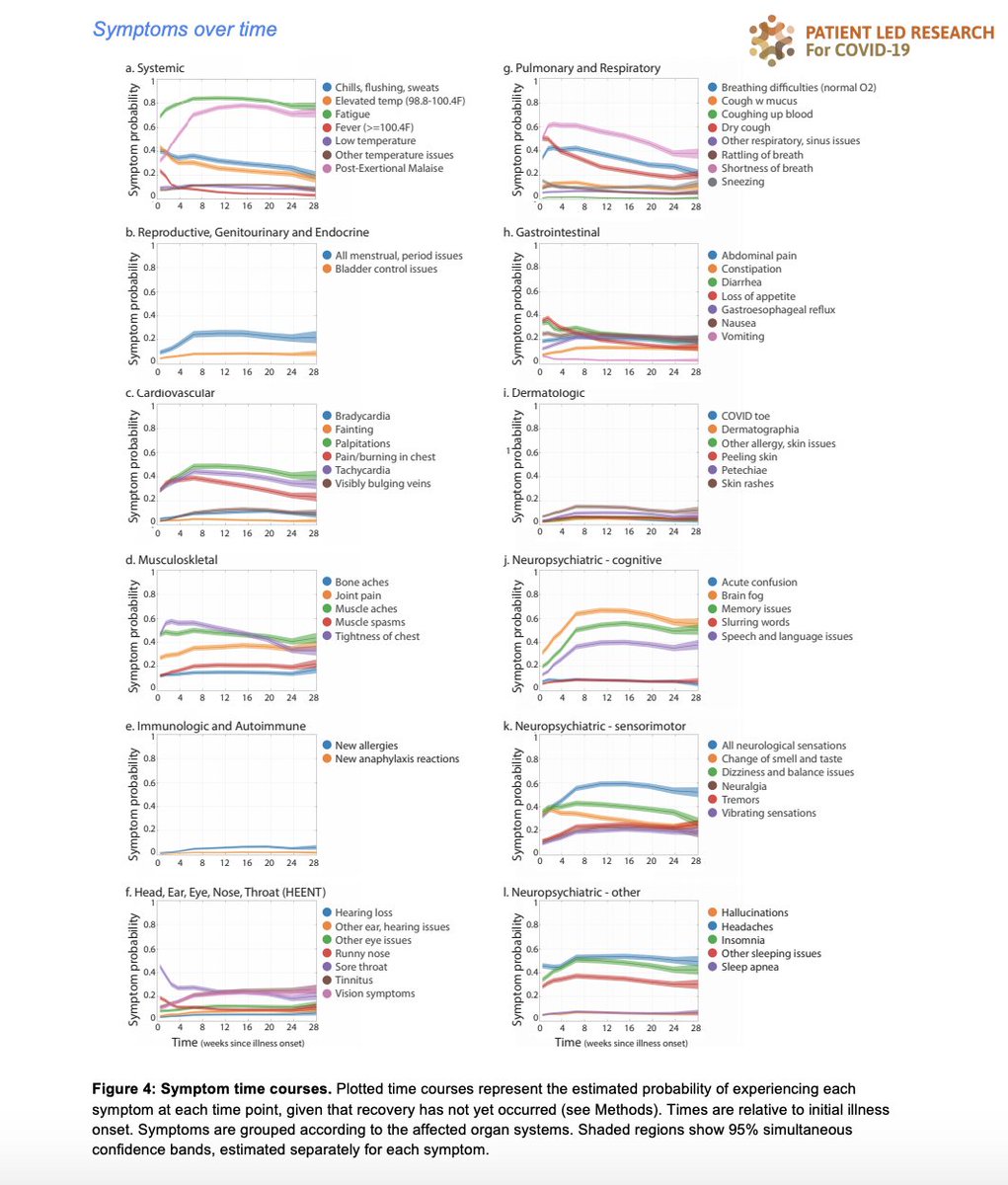
...ways that this has affected #LongCOVID patients (I'd add that the focus on hospitalized patients only, or respiratory symptoms only, will be a huge problem if anyone uses ML for #LongCOVID at this stage).
3/
3/
And she grounds it in her own experience of the system, being dismissed for a serious brain injury before eventually, days later and a different ER, getting the help she needed.
4/
4/
She mentions other like @aubreyhirsch (and #pwme, and many of us #LongCOVID patients, and activists like @ludawinthesky) have permanent damage from not being treated on time, due to being dismissed and not believed.
5/
5/
She highlights the big problem of doctors believing they're the only ones with experience, & the very related one of ML practitioners making datasets (such as radiology images) with inaccuracies - both assuming they don't need feedback from people w' lived experience.
6/
6/
This is also the problem with creating machine learning datasets based on records that use doctors' notes and diagnoses alone - because doctors often ignore what they think is not relevant, or what they don't understand.
7/
7/
(An aside that an easy-ish ML project/dataset that could be funded is have @jenbrea and crew tag radiology images of the spine with their unbelievable patient-led knowledge of #MESPINE issues - I've learned more from this group than anything I've found online).
8/
8/
Anyway, the piece is a necessary read. Mentioning work from @EricTopol, @herlifeinpixels, our own @patientled team, and others. Thank you Rachel!
9/
9/
• • •
Missing some Tweet in this thread? You can try to
force a refresh