📞 Nurse: Patient has a blood pressure of 226/118 mmHg!
📞 Resident: Nifedipine 30 mg STAT!
.....
📞 Me: About that last call, please hold Nifedipine until we assess the patient
A 🧵of some cases of Inpatient Hypertension 👇 1/15
📞 Resident: Nifedipine 30 mg STAT!
.....
📞 Me: About that last call, please hold Nifedipine until we assess the patient
A 🧵of some cases of Inpatient Hypertension 👇 1/15
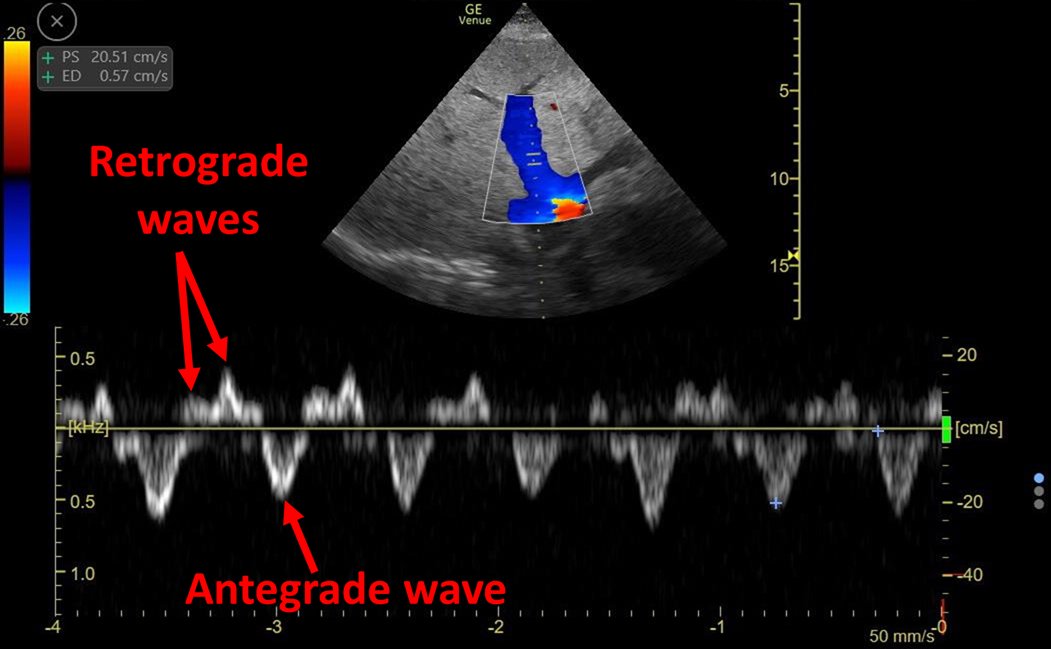
🔎🖥️..This was a pt w ARDS on IMV. Other vitals 🆗. Previous BP= normal, no recent change in sedation, vent 🆗, no asynchronies. UOP = 0 for 2 hrs 🤔. Exam: Distended bladder!
After foley catheter change, BP normalised 😎
Why do we have this reflex to treat acute high BP? 2/15
After foley catheter change, BP normalised 😎
Why do we have this reflex to treat acute high BP? 2/15

A big component is the perceived expectation that we must do something! (In our minds, Are we trying to prevent organ injury?)
A great example can be seen here 👇 3/15
A great example can be seen here 👇 3/15
https://twitter.com/DrMcInnisDIT/status/1269320470526132225?s=20
However it is important to understand fist how is it that acute hypertension can lead to organ injury:
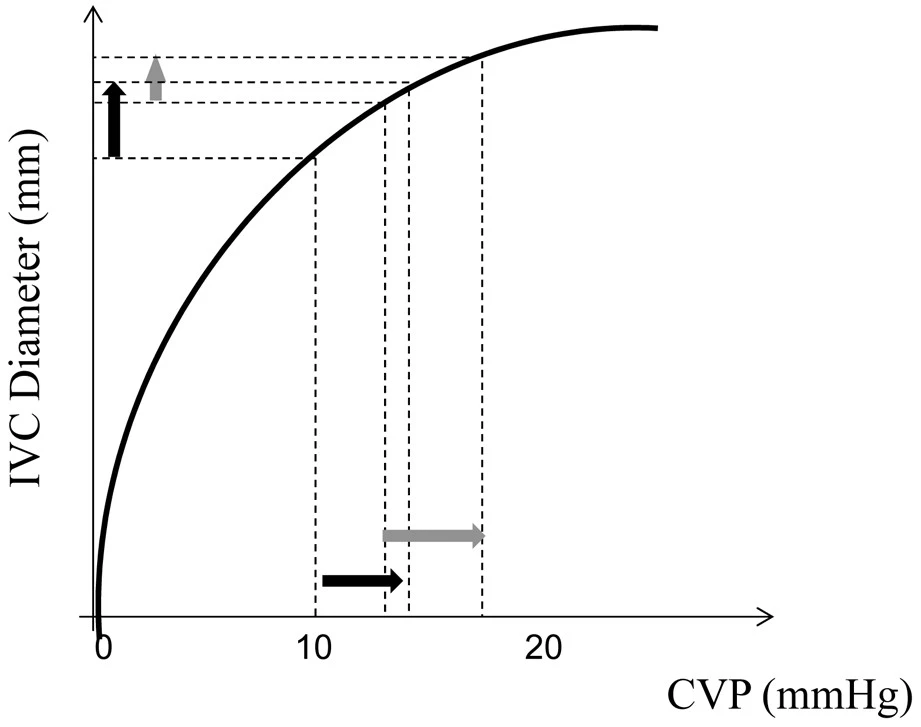
1⃣Sudden increase in afterload (🫁♥️):
➡️ heart failure with pulmonary edema.
➡️ Increased myocardial O2 demand leading to supply/demand mismatch... 4/15
1⃣Sudden increase in afterload (🫁♥️):
➡️ heart failure with pulmonary edema.
➡️ Increased myocardial O2 demand leading to supply/demand mismatch... 4/15

2⃣Failure of auto-regulation (🧠):
🔷visual disturbance
🔷seizure
🔷delirium
#POCUS of optic nerve might help support this diagnosis!
(The level of BP at which auto-regulation fails varies and it is modulated by preexistent chronic hypertension)
5/15

🔷visual disturbance
🔷seizure
🔷delirium
#POCUS of optic nerve might help support this diagnosis!
(The level of BP at which auto-regulation fails varies and it is modulated by preexistent chronic hypertension)
5/15


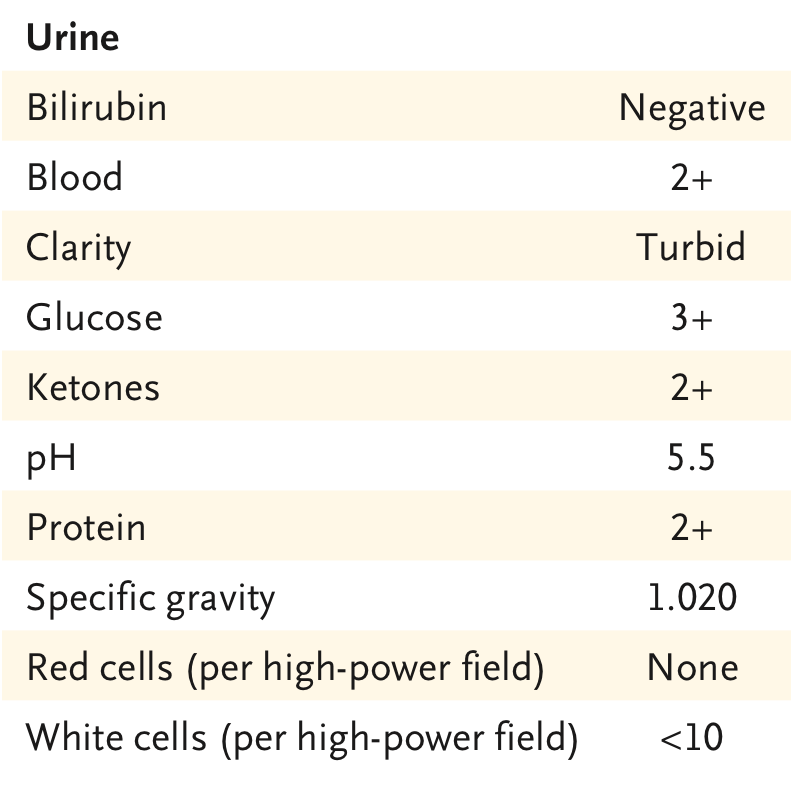
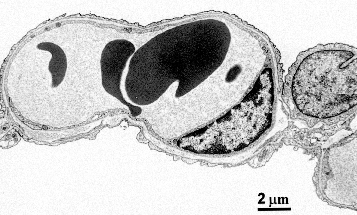
Is AKI really a hypertensive emergency? I actually don't believe so..
A really juicy🧃 debate: Does acute hypertension cause endothelial damage and TMA or does TMA cause endothelial damage and HTN as a result?
Interesting perspectives 👇 6/15
A really juicy🧃 debate: Does acute hypertension cause endothelial damage and TMA or does TMA cause endothelial damage and HTN as a result?
Interesting perspectives 👇 6/15
https://twitter.com/kdjhaveri/status/1217459664910213120?s=20
So, the evaluation of acute inpatient HTN should include a detailed interrogation + physical + EKG + #POCUS of🫁♥️👁️ +/- chemistries
An excellent discussion on the approach and management of hypertensive emergencies by @PulmCrit can be found here: emcrit.org/ibcc/hypertens… 7/15
An excellent discussion on the approach and management of hypertensive emergencies by @PulmCrit can be found here: emcrit.org/ibcc/hypertens… 7/15
For acute hypertension to become an emergency🚨, there has to be ORGAN INJURY
There is no such thing as a "hypertensive urgency" 🤮
Acutely treating ISOLATED inpatient hypertension is actually associated with worse outcomes! 8/15
jamanetwork.com/journals/jamai…
There is no such thing as a "hypertensive urgency" 🤮
Acutely treating ISOLATED inpatient hypertension is actually associated with worse outcomes! 8/15
jamanetwork.com/journals/jamai…
A very elegant discussions by @thecurbsiders on the nuances of treating asymptomatic inpatient hypertension can be found here:
thecurbsiders.com/podcast/144-ne… 9/15
thecurbsiders.com/podcast/144-ne… 9/15
As an example of a case that DID need emergent tx:
I was 📞 to see a 👵 w chest pain during hematopoietic stem cell infusion. BP = 209/120. EKG 👇.
This pattern (diffuse ST depression with STE in AvR) = global subendocardial ischemia = supply/demand mismatch!
10/15
I was 📞 to see a 👵 w chest pain during hematopoietic stem cell infusion. BP = 209/120. EKG 👇.
This pattern (diffuse ST depression with STE in AvR) = global subendocardial ischemia = supply/demand mismatch!
10/15

💉IV nitroglycerin resolved the pain and EKG changes!
This patient had a clear cause for acute HTN: It is a very well reported side effect of HSCs infusion.
Risk factors include volume of infusion, granulocyte content and DMSO concentration (PMID: 29891441)
11/15
This patient had a clear cause for acute HTN: It is a very well reported side effect of HSCs infusion.
Risk factors include volume of infusion, granulocyte content and DMSO concentration (PMID: 29891441)
11/15

Finally, a case that humbled me regarding this subject:
This was a pt w SLE + nephritis flare who I was about to discharge home
📞 Nurse: Pt has a BP of 160/100!
📞 Me: Don't worry, I will adjust her outpatient BP meds!
Later, as I go to the 🛌, she begins seizing 😱 12/15
This was a pt w SLE + nephritis flare who I was about to discharge home
📞 Nurse: Pt has a BP of 160/100!
📞 Me: Don't worry, I will adjust her outpatient BP meds!
Later, as I go to the 🛌, she begins seizing 😱 12/15

Pt had chronic hypertension and BP was not that high. So I was surprised!
I ruled out other causes of seizures and MRI confirmed PRES
She did well with benzodiazepines + acute IV treatment of HTN 😅
(Also, nurse gave me her "I told you so" face ☹️)
13/15
I ruled out other causes of seizures and MRI confirmed PRES
She did well with benzodiazepines + acute IV treatment of HTN 😅
(Also, nurse gave me her "I told you so" face ☹️)
13/15

Turns out SLE is an important risk factor for PRES, even with mild HTN!
This patient had all the risk factors for this complication:
🔷SLE activity
🔷Renal disease
🔷Immunosuppressive therapy
🔷High dose Corticosteroids
14/15
sciencedirect.com/science/articl…
This patient had all the risk factors for this complication:
🔷SLE activity
🔷Renal disease
🔷Immunosuppressive therapy
🔷High dose Corticosteroids
14/15
sciencedirect.com/science/articl…
So...while most asymptomatic inpatients with acute HTN do not seem to need STAT treatment (worse outcomes)
...there may be cases that benefit from individualising the decision to treat urgently, probably based on risk factors for complications: e.g. severe HF, SLE, etc..
15/15
...there may be cases that benefit from individualising the decision to treat urgently, probably based on risk factors for complications: e.g. severe HF, SLE, etc..
15/15
• • •
Missing some Tweet in this thread? You can try to
force a refresh