So proud of this work led by @vincentjmajor & Erwin Wang w/@NicoleAdlerMD @hauck_kevin @AustrianMd
@yindalon @nyulangone in @nejmcatalyst. This is how to do thoughtful, collaborative integration of #AI into clinical care to create a learning health system catalyst.nejm.org/doi/full/10.10…
@yindalon @nyulangone in @nejmcatalyst. This is how to do thoughtful, collaborative integration of #AI into clinical care to create a learning health system catalyst.nejm.org/doi/full/10.10…
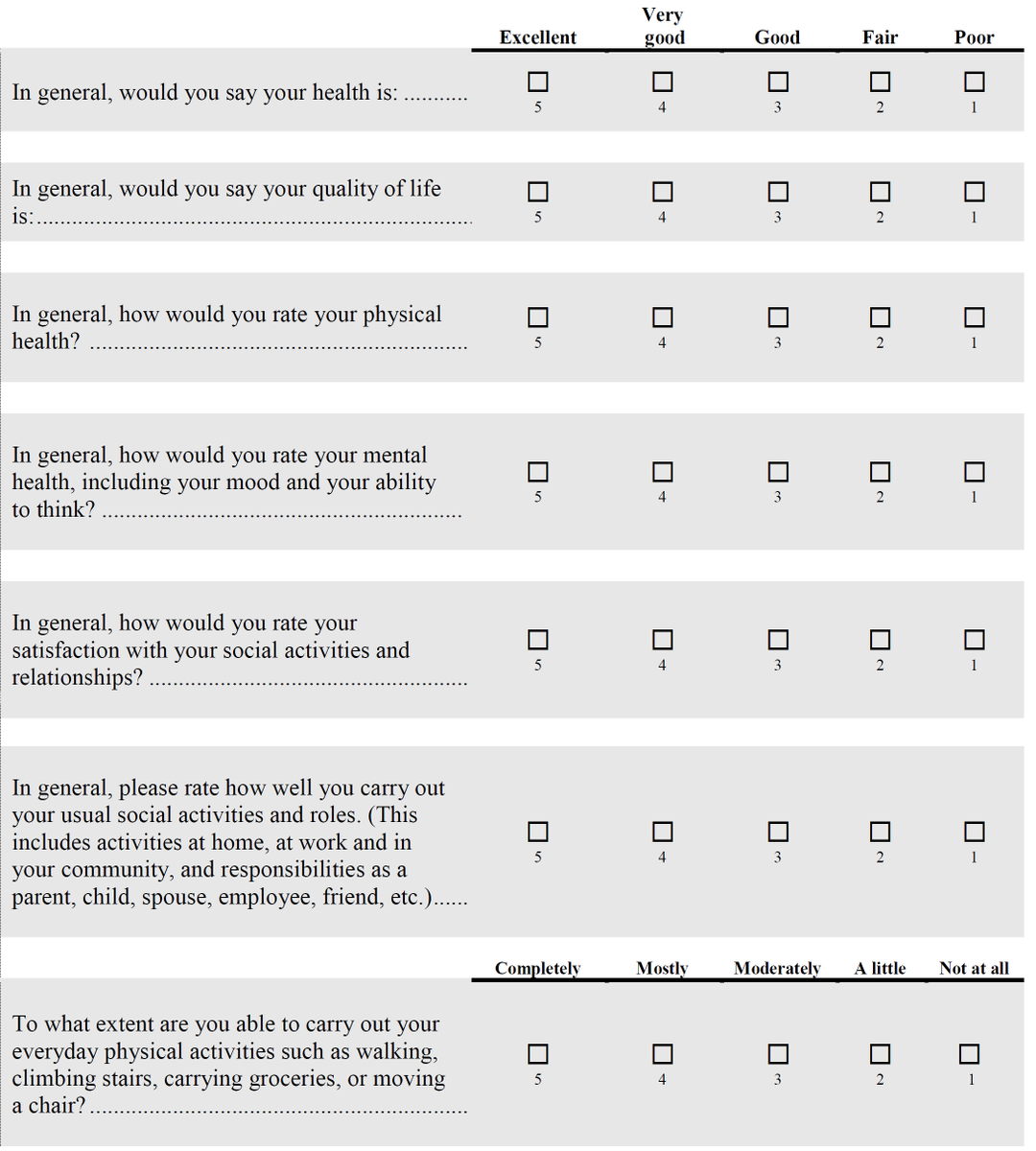
At baseline, only 16% of our patients hospitalized within 6 months of death had documentation of advanced care planning. @vincentjmajor & clin colleagues developed 3 predictive models for 2 month mortality, set appropriate threshold (75% PPV), and integrated into the EHR. 

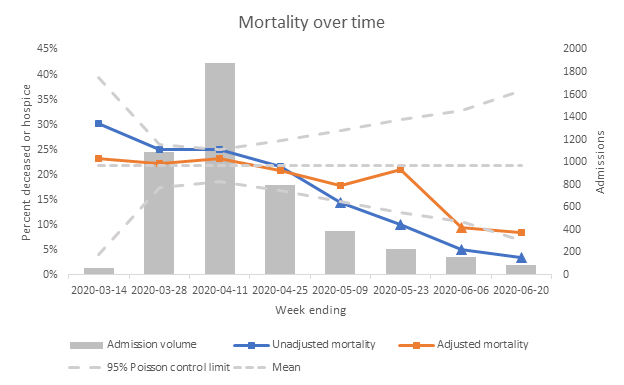
The alert was shown a max of twice, only to attending physicians. 71% agreed with the alert: 72% of those patients had advanced care planning, vs 34% of those where docs disagreed, so overall 66% of alerted patients had ACP performed. How does that compare to others? Next... 

Alerted patients (even including the disagreements) had a MUCH higher rate of advanced care planning discussions than the ones that just missed the threshold for alert (34%), and even than all those who ultimately died (52%). We improved patient-centered care at end of life. 

In fact, actual 60-day survival among alerted patients was higher than the predicted 25% even among those with alert agreement (panel B), suggesting either model overestimated risk or avoidance of high intensity care at end of life extended survival (or both). 

Finally, note that only 0.5% of patients met alert threshold, ensuring a highly targeted intervention that avoided alert fatigue.
• • •
Missing some Tweet in this thread? You can try to
force a refresh