1/ 💭 Thoughts of a trainee 💭
"I thought that rotation went well.
Why did I get straight 3s on my evaluation?
And how can I improve?
There aren't any written comments!"
Sound familiar?
How can we prevent this from happening?
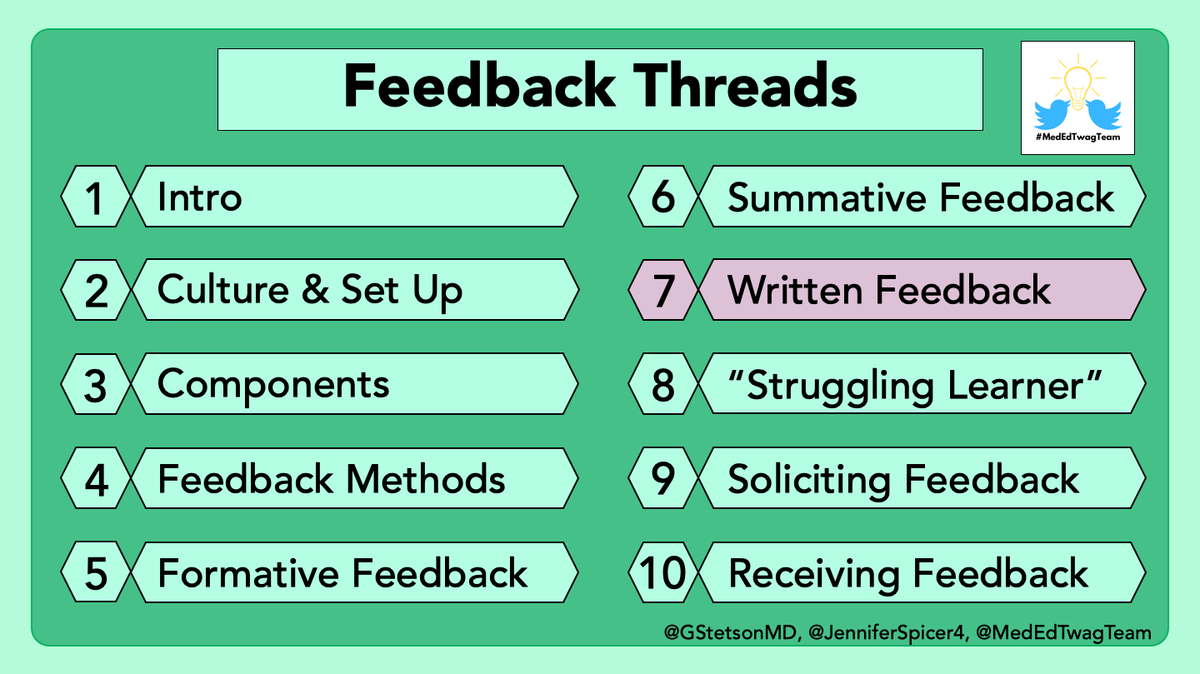
Read this week's #tweetorial: Written Feedback
"I thought that rotation went well.
Why did I get straight 3s on my evaluation?
And how can I improve?
There aren't any written comments!"
Sound familiar?
How can we prevent this from happening?
Read this week's #tweetorial: Written Feedback

2/ This week we will discuss how to give effective written #feedback.
In #MedEd, written feedback is most frequently given in the form of "end-of-rotation" evaluations (also known as "in-training evaluation reports" or ITERs).
In #MedEd, written feedback is most frequently given in the form of "end-of-rotation" evaluations (also known as "in-training evaluation reports" or ITERs).
3/ We all have a long to-do list. Why should we prioritize high-quality written evaluations?
✅ They impact trainees' grades.
✅ Comments can be used for LORs.
✅ Provide a tangible record of progress during training
✅ They impact trainees' grades.
✅ Comments can be used for LORs.
✅ Provide a tangible record of progress during training
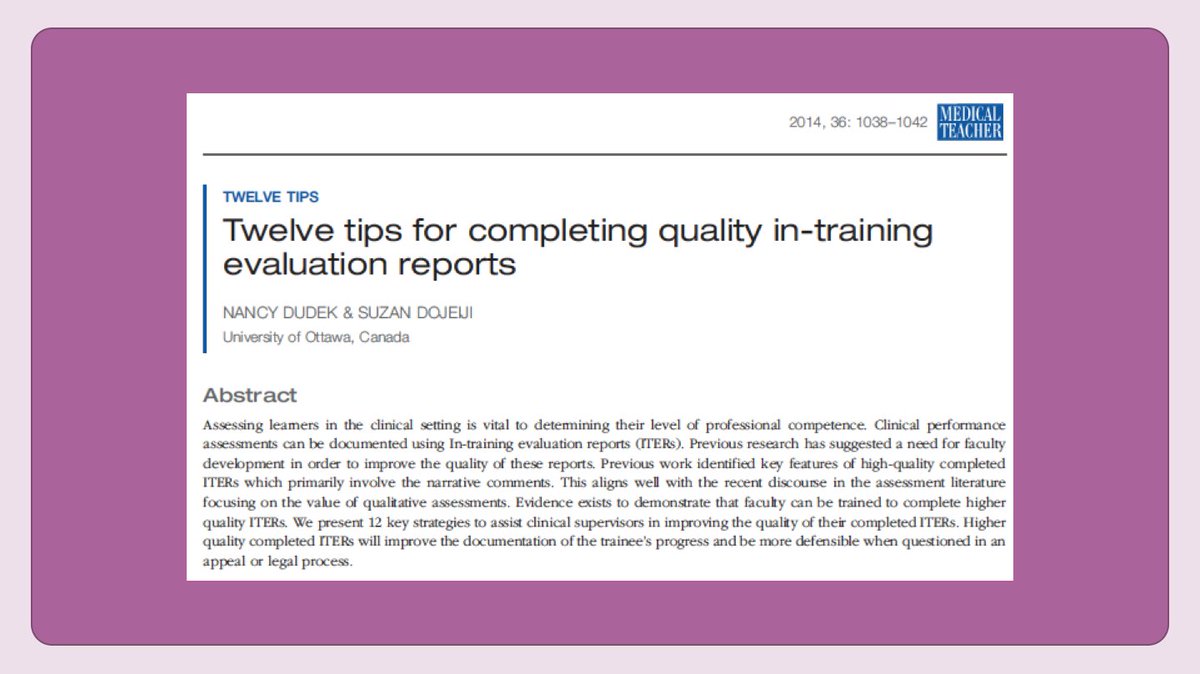
4/ This article in @MedTeachJournal has great tips, including:
✅ Know your institution's evaluation process
✅ Mirror in-person feedback
✅ Write comments before numerical ratings
✅ Include specific examples
✅ Match ratings to the comments
Let's discuss each in more depth
✅ Know your institution's evaluation process
✅ Mirror in-person feedback
✅ Write comments before numerical ratings
✅ Include specific examples
✅ Match ratings to the comments
Let's discuss each in more depth
5/ First, know your institution’s evaluation process.
*⃣Ask leaders the questions on this slide, which will help you make informed decisions regarding how to fill out evaluations.
*⃣Advocate for faculty to receive data regarding how their ratings compare to the "average.”
*⃣Ask leaders the questions on this slide, which will help you make informed decisions regarding how to fill out evaluations.
*⃣Advocate for faculty to receive data regarding how their ratings compare to the "average.”

6/ Second, mirror your in-person feedback.
Written feedback should be a summary of in-person feedback.
In fact, I often fill out my written eval, save it, then do in-person feedback, then edit if needed.
Remember, feedback should NEVER be a surprise!
Written feedback should be a summary of in-person feedback.
In fact, I often fill out my written eval, save it, then do in-person feedback, then edit if needed.
Remember, feedback should NEVER be a surprise!
https://twitter.com/JenniferSpicer4/status/1371863186459201536
7/ Third, write your comments first.
1⃣Written comments do the best job of "painting a picture" of the trainee.
2⃣The written comments can guide your ratings.
1⃣Written comments do the best job of "painting a picture" of the trainee.
2⃣The written comments can guide your ratings.
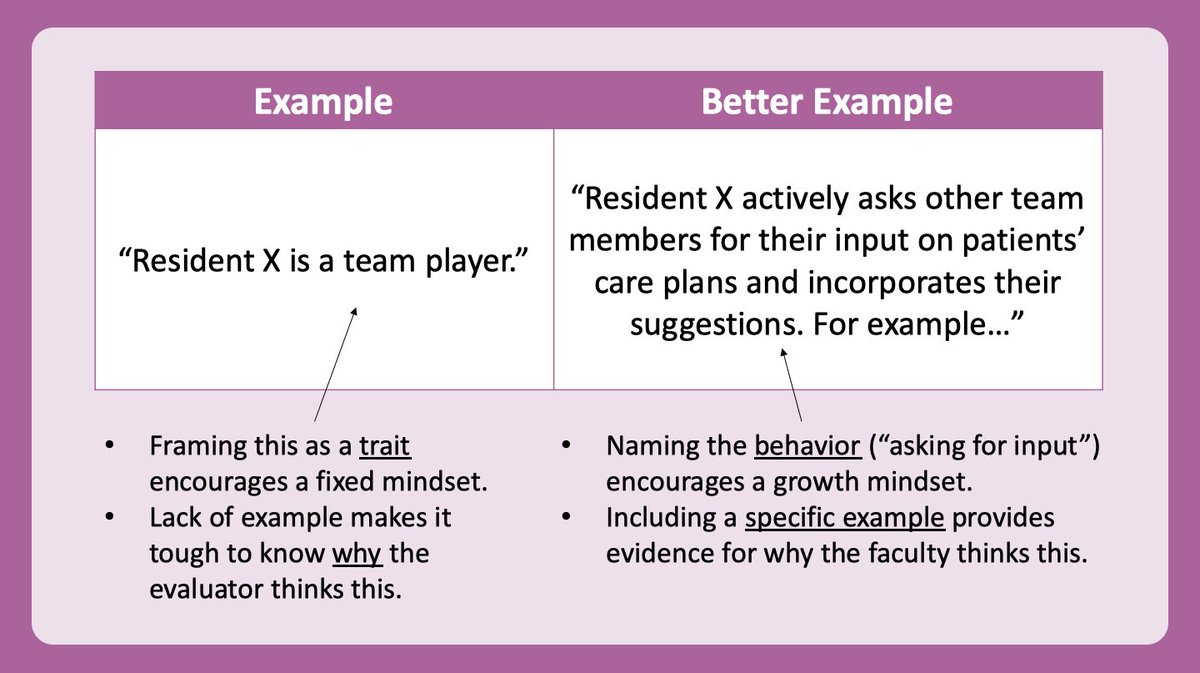
8/ Fourth, write detailed narratives.
Most of our comments are of moderate to low quality: pubmed.ncbi.nlm.nih.gov/25691242/
Improve written comments by:
✅Using the ACGME competencies as a framework
✅Commenting on behaviors NOT personal attributes
✅Including a specific example
Most of our comments are of moderate to low quality: pubmed.ncbi.nlm.nih.gov/25691242/
Improve written comments by:
✅Using the ACGME competencies as a framework
✅Commenting on behaviors NOT personal attributes
✅Including a specific example
9/ As a bonus, writing detailed narratives makes it incredibly easy to write excellent letters of recommendation in the future!
10/ Fifth, after writing your narratives comments, use those to guide your ratings on the quantitative scales.
Do NOT just give someone straight 4s – truly consider their performance in each area.
Do NOT just give someone straight 4s – truly consider their performance in each area.
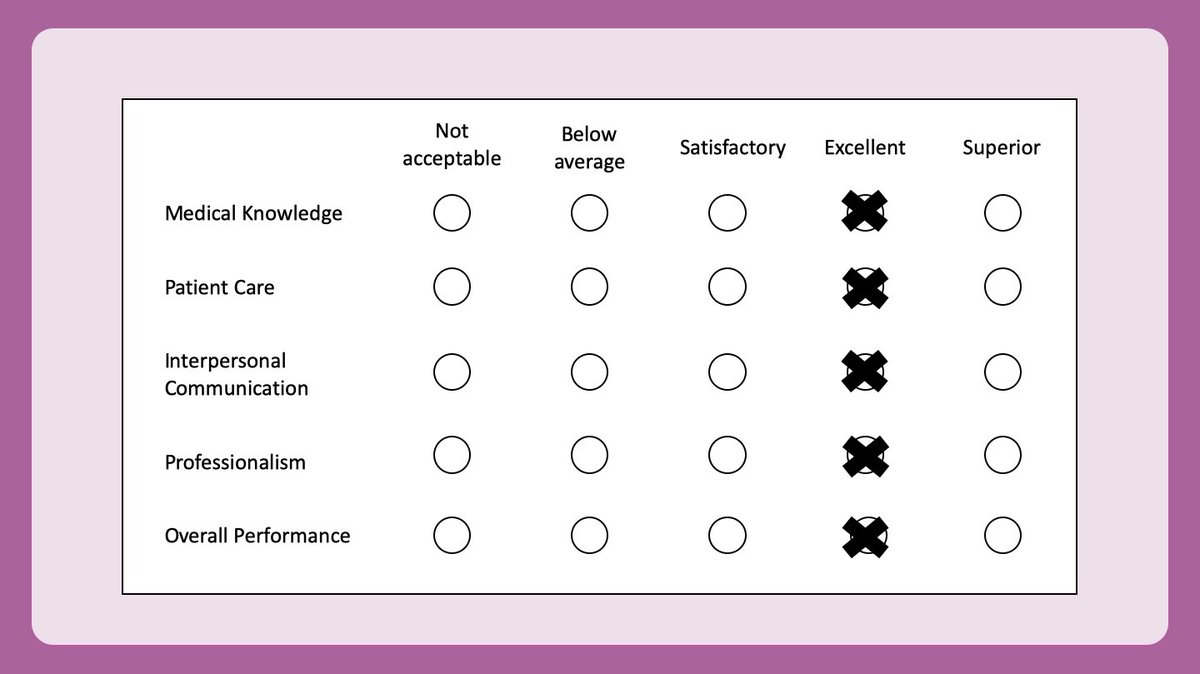
11/ Now, part of the reason we often give “straight 4s or 5s” is because our rating scales are less than ideal.
But changing our rating scales by creating specific, behavioral anchors can increase the variability of ratings, as shown in this paper:
pubmed.ncbi.nlm.nih.gov/27168886/
But changing our rating scales by creating specific, behavioral anchors can increase the variability of ratings, as shown in this paper:
pubmed.ncbi.nlm.nih.gov/27168886/

12/ And, an even better way of creating an evaluation is to eliminate terms like “satisfactory” & “excellent” and just have a description of the behavior.
See this example of a behaviorally anchored rating scale adapted from the excellent @EmoryInfectDis fellow evaluations.
See this example of a behaviorally anchored rating scale adapted from the excellent @EmoryInfectDis fellow evaluations.

13/ As faculty (or trainees), we can advocate for better written evaluations!
And this document from @UCSFMed has some excellent tips:
meded.ucsf.edu/sites/meded.uc…
And this document from @UCSFMed has some excellent tips:
meded.ucsf.edu/sites/meded.uc…
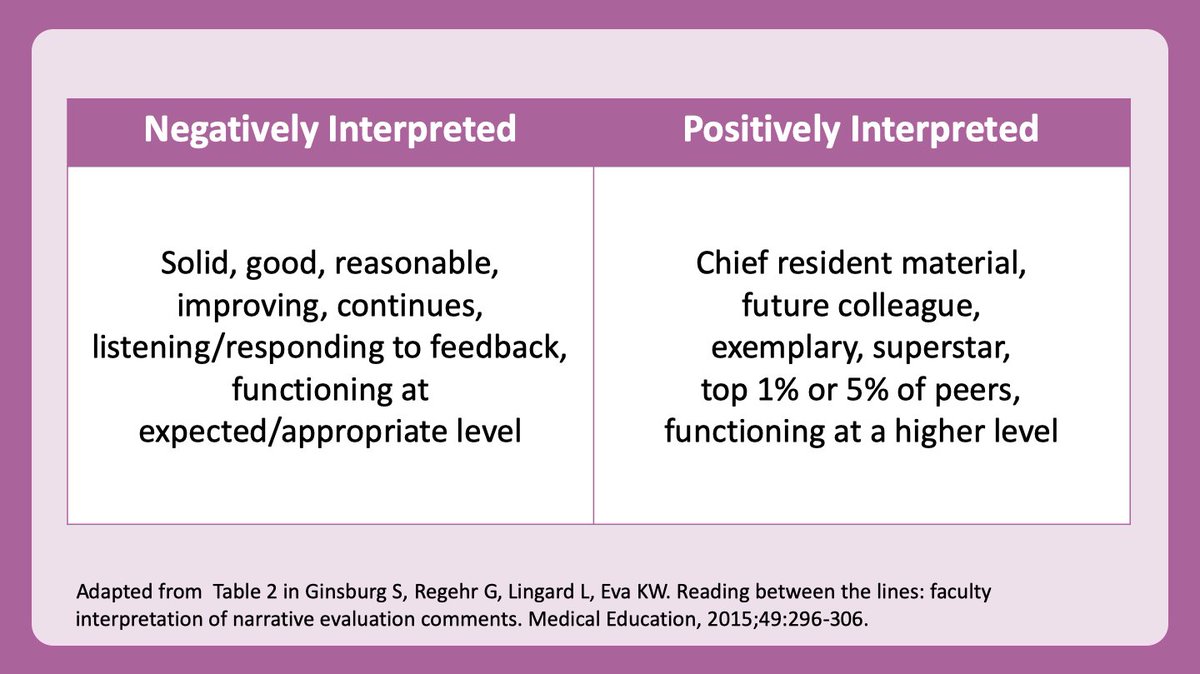
14/ Finally, I want to address the “hidden code” in evaluations.
We may intentionally (or unintentionally) communicate things in our narrative comments. This article outlines how we often use "coded language": pubmed.ncbi.nlm.nih.gov/25693989/
Be aware of how these terms are interpreted
We may intentionally (or unintentionally) communicate things in our narrative comments. This article outlines how we often use "coded language": pubmed.ncbi.nlm.nih.gov/25693989/
Be aware of how these terms are interpreted
15/ Studies show we perpetuate stereotypes/bias in our evaluations.
Before submitting an evaluation, scan it for unintended stereotypes.
See this handout from @UCSFMed
meded.ucsf.edu/sites/meded.uc…
Copy & paste into this website to check for gender bias: slowe.github.io/genderbias/
Before submitting an evaluation, scan it for unintended stereotypes.
See this handout from @UCSFMed
meded.ucsf.edu/sites/meded.uc…
Copy & paste into this website to check for gender bias: slowe.github.io/genderbias/

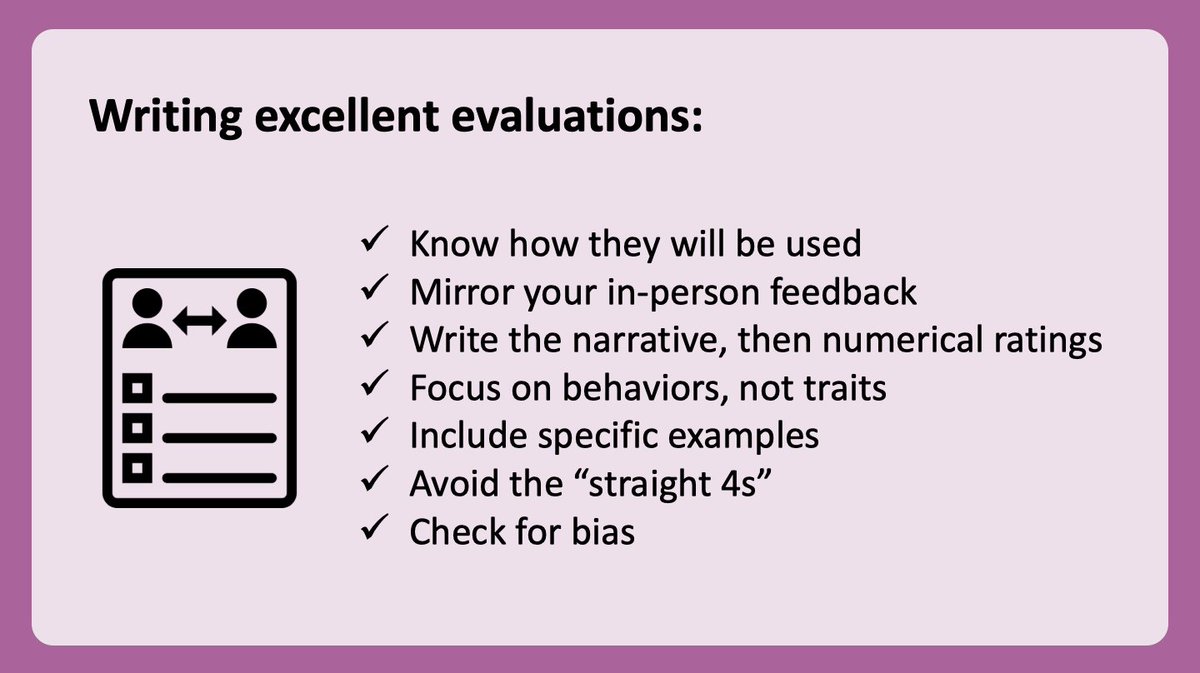
16/ Next time you sit down to complete an evaluation, consider this checklist.
Why?
Because others deserve our time & energy to provide them with specific, helpful feedback.
These principles are helpful for written evaluations of our supervisors too!
Why?
Because others deserve our time & energy to provide them with specific, helpful feedback.
These principles are helpful for written evaluations of our supervisors too!
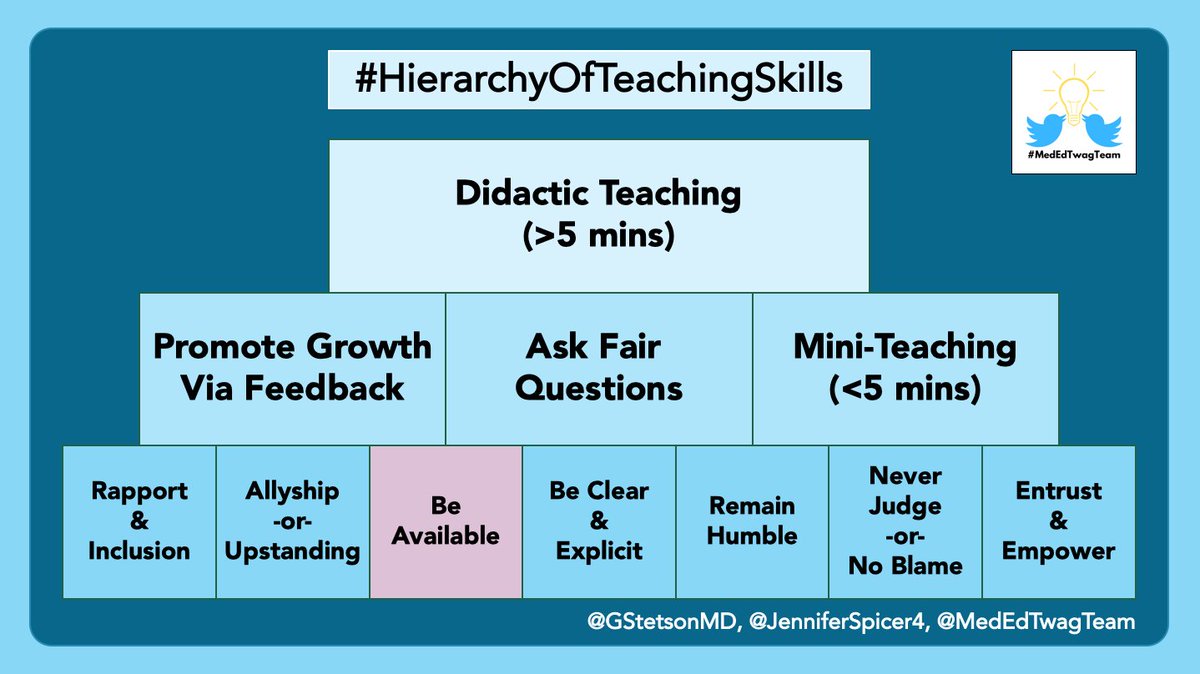
17/ Thanks for joining the @MedEdTwagTeam #TweetorialTuesday on #feedback.
Next week, follow @GStetsonMD for a focused thread on tips for coaching a learner who isn’t meeting expectations in a systematic and supportive manner.
Next week, follow @GStetsonMD for a focused thread on tips for coaching a learner who isn’t meeting expectations in a systematic and supportive manner.

• • •
Missing some Tweet in this thread? You can try to
force a refresh