“Should I call my [resident/fellow/attending]?”
“I don’t want to be a bother.”
“I don’t want them to think I’m dumb.”
Sound familiar?
I know these thoughts plagued me.
How can we prevent this?
This week’s #ClinicalTeaching topic: Be Available
Imposter syndrome is prevalent in medicine:
link.springer.com/article/10.100…
We should encourage team members to ask questions.
...And answer those questions.
Saying "look it up" is not always helpful
As a trainee, I found myself worrying about “bothering” people when I called.
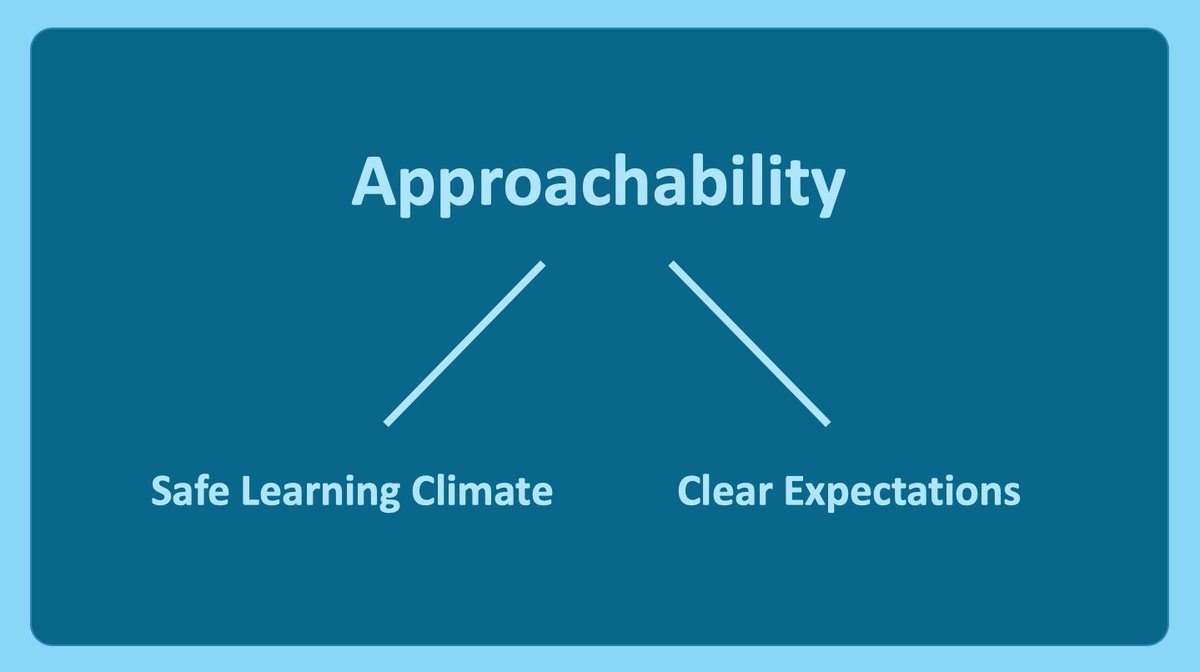
As attendings/fellows/residents, we should set the expectation that needing help is normal & reiterate that people should call if needed
I tell trainees they can contact me anytime when I’m awake (5:00 am – 9:00 pm), & ANYTIME for the following:
If a patient decompensates
If a patient tries to leave AMA
If a time-sensitive decision needs to be made
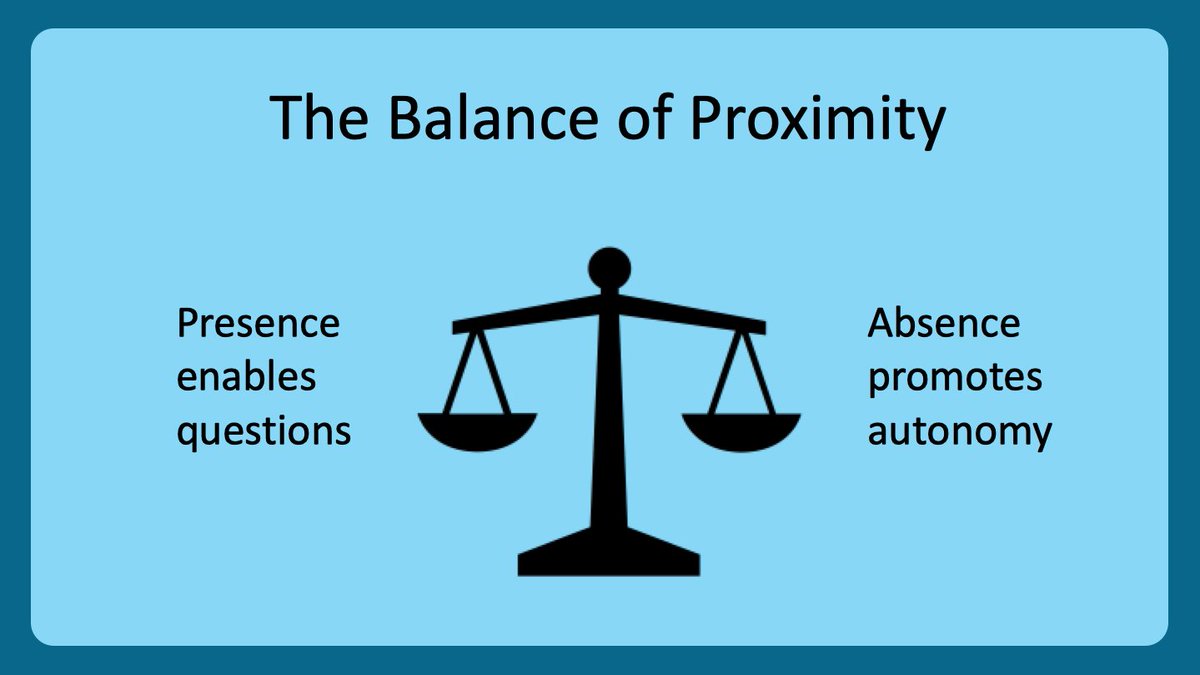
When I say proximity, I mean both:
👉 Physical proximity (i.e. in the same room, hospital, etc)
👉 Mental proximity (i.e. not staring at your phone, thinking of something else, etc)
Then, during rounds, pay attention.
✅ Use active learning techniques
✅ Use positive, open body language
✅ Avoid glancing at your phone
✅ Avoid looking at the patient's chart
And, if presentations are too long, then provide feedback instead of tuning out!
⭐️Fellows⭐️
Residents will write better consult notes b/c they are more likely to ask detail-oriented questions
⭐️Residents⭐️
Interns will appreciate you helping them with work; plus, you will know more about their workflow & efficiency
You have lots to teach.
And you can help the students shine on rounds.
Just set clear expectations with students to maximize learning & patient care
(more on this next week from @GStetsonMD!)
And check out the @MedEdTwagTeam if you want to see all of our threads in one place!
Thanks for joining, and we will see you next week!