1/ Welcome to the first part of a #Tweetorial series on #VenousDisease.
🩸To begin how about we talk about the main player in the game- C.L.O.T. (and why you should care about it)
#Cardiotwitter #Irad #fellows #fellowtwitter #medthread #clot #medtwitter #clottwitter
🩸To begin how about we talk about the main player in the game- C.L.O.T. (and why you should care about it)
#Cardiotwitter #Irad #fellows #fellowtwitter #medthread #clot #medtwitter #clottwitter
2/ But first a question- Is there a difference between arterial and venous clot??
#Clot #cardiology #DVT #irad #VenousDisease #medthread #tweetorial #fellows @HadyLichaaMD @VladLakhter @agtruesdell @AntoniousAttall @TheNarulaSeries @t_intheleadcoat @ShariqShamimMD
#Clot #cardiology #DVT #irad #VenousDisease #medthread #tweetorial #fellows @HadyLichaaMD @VladLakhter @agtruesdell @AntoniousAttall @TheNarulaSeries @t_intheleadcoat @ShariqShamimMD
4/ Arterial clots➡️ platelet rich, Venous clots➡️ clotting factors.
However, there is evidence that this dichotomy is likely to be an oversimplification. We have seen this with left atrial appendage thrombus and in acute MI (fibrin rich thrombus)
#medtwitter #clottwitter
However, there is evidence that this dichotomy is likely to be an oversimplification. We have seen this with left atrial appendage thrombus and in acute MI (fibrin rich thrombus)
#medtwitter #clottwitter
5/ Major differences between arterial and venous #thrombosis.
(A) Arterial= high shear flow when platelet rich thrombi are formed around ruptured at plaques+damaged endothelium.
(B) DVT= low shear flow. Intact endothelial wall. Fibrin rich, large amount of RBCs+ platelets
(A) Arterial= high shear flow when platelet rich thrombi are formed around ruptured at plaques+damaged endothelium.
(B) DVT= low shear flow. Intact endothelial wall. Fibrin rich, large amount of RBCs+ platelets

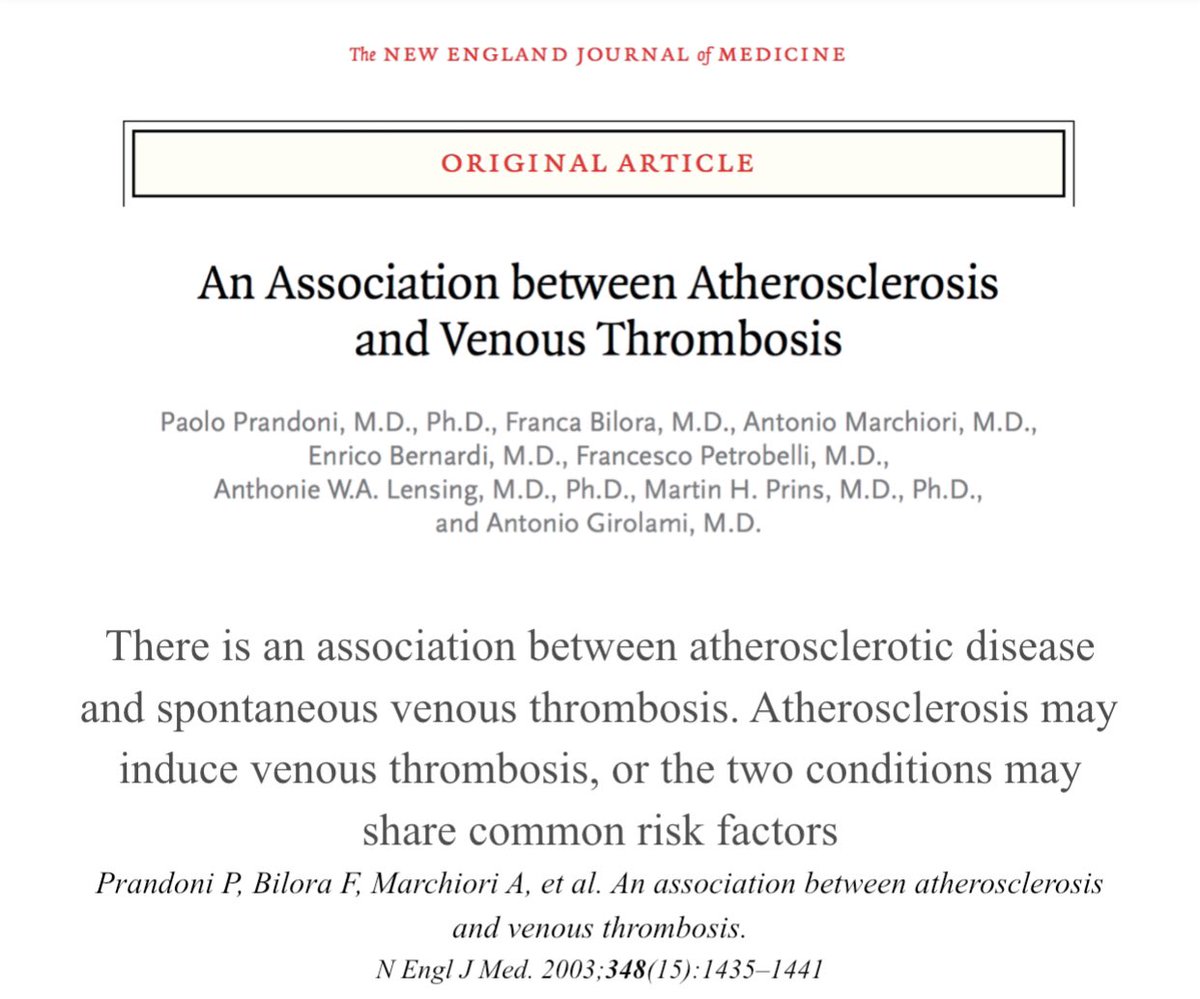
6/ Is there a connection b/w DVT and atherosclerosis?
2003 NEJM
multivariate analysis taking into account risk factors for atherosclerosis, the OR for carotid dz in pts with unprovoked as compared to 2° DVT and controls was found to be 2.4, (highly statistically significant)
2003 NEJM
multivariate analysis taking into account risk factors for atherosclerosis, the OR for carotid dz in pts with unprovoked as compared to 2° DVT and controls was found to be 2.4, (highly statistically significant)
7/ Another study from Lancet
Pts with DVT, the RR varied from 1.60 for MI (95% CI 1.35–1.91) to 2.19 (1.85–2.60) for CVA in the 1st yr after DVT. Pts with PE, the RR in that yr were 2.60 (2.14–3.14) for MI and 2.93 (2·34–3·66) for CVA. 20–40% increases in risk for events >20 yrs
Pts with DVT, the RR varied from 1.60 for MI (95% CI 1.35–1.91) to 2.19 (1.85–2.60) for CVA in the 1st yr after DVT. Pts with PE, the RR in that yr were 2.60 (2.14–3.14) for MI and 2.93 (2·34–3·66) for CVA. 20–40% increases in risk for events >20 yrs

8/ What's the connection? We still don’t completely know, but my hypothesis: Inflammation +residual obs (positive feedback loop).
As a #cardiologist u should be interested in venous dz. It will affect your pts, I guarantee it. Thank u #Vascsurg and #IRAD for setting the stage
As a #cardiologist u should be interested in venous dz. It will affect your pts, I guarantee it. Thank u #Vascsurg and #IRAD for setting the stage

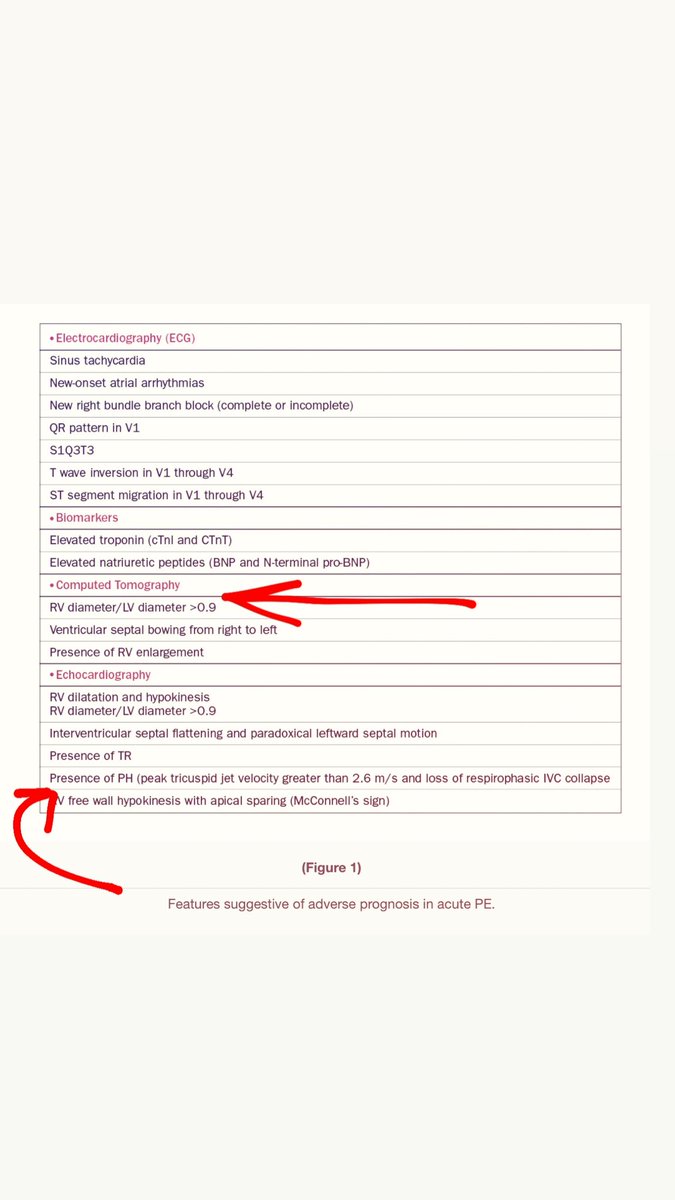
9/ Ok...now that you see the importance of #CLOT. Let's talk about how they present:
#Arterial-usually presents acutely (within 48 hours)
#Venous- varies, but often days to weeks later.
This is important because time matters!
#Arterial-usually presents acutely (within 48 hours)
#Venous- varies, but often days to weeks later.
This is important because time matters!

11/ Here is some very interesting histopathology data from Silver et al. demonstrating that only 28% of DVTs and 21% of PEs were composed of fibrin thrombus.
Timing matters! So how we pick treatment should matter too! #VTE #Clot #medtwitter
Timing matters! So how we pick treatment should matter too! #VTE #Clot #medtwitter

12/ If #ChronicClot is collagenous what treatments do you think will work best?? #clot #lysis #thrombectomy #medtwitter
13/ Despite optimal anticoagulation, > 30% of pts with a hx of DVT will develop post-thrombotic syndrome (#PTS), likely due to chronic venous occlusion, suboptimal collaterals, and venous valvular dysfunction. Up to 1/3 of these patients will develop severe debilitating symptoms 

14/ Treatment:
First line- Medical therapy
Refractory symptoms with
Proximal clot- Catheter treatment
So far we have multiple catheter modalities. These are the 4 I have the most familiarity with
#VTE #clot #clottwitter
First line- Medical therapy
Refractory symptoms with
Proximal clot- Catheter treatment
So far we have multiple catheter modalities. These are the 4 I have the most familiarity with
#VTE #clot #clottwitter

15/ it’s important to remember that patients often present days after the onset of symptoms, which is why we have struggle with advanced interventional therapy #Thrombectomy #lysis #clot #medtwitter 

17/ So what have we learned so far…
❤️🩹Clot is a nidus for more clot.
🦴Clot turns collagenous quickly.
😢Residual obstruction is bad and drastically decreases a patient's quality of life.
❓We have multiple treatment options, but how do we make the choice between them? #VTE
❤️🩹Clot is a nidus for more clot.
🦴Clot turns collagenous quickly.
😢Residual obstruction is bad and drastically decreases a patient's quality of life.
❓We have multiple treatment options, but how do we make the choice between them? #VTE
18/ CAVENT (Catheter-Directed Venous Thrombolysis in Acute Iliofemoral Vein Thrombosis)
multi-center, RCCT 209 Pts with 1st time acute DVT
Perfusion catheters+alteplase
CDT--> clinical benefit during follow-up for up to 5 yrs, However, therapy ❌quality of life #VTE
multi-center, RCCT 209 Pts with 1st time acute DVT
Perfusion catheters+alteplase
CDT--> clinical benefit during follow-up for up to 5 yrs, However, therapy ❌quality of life #VTE

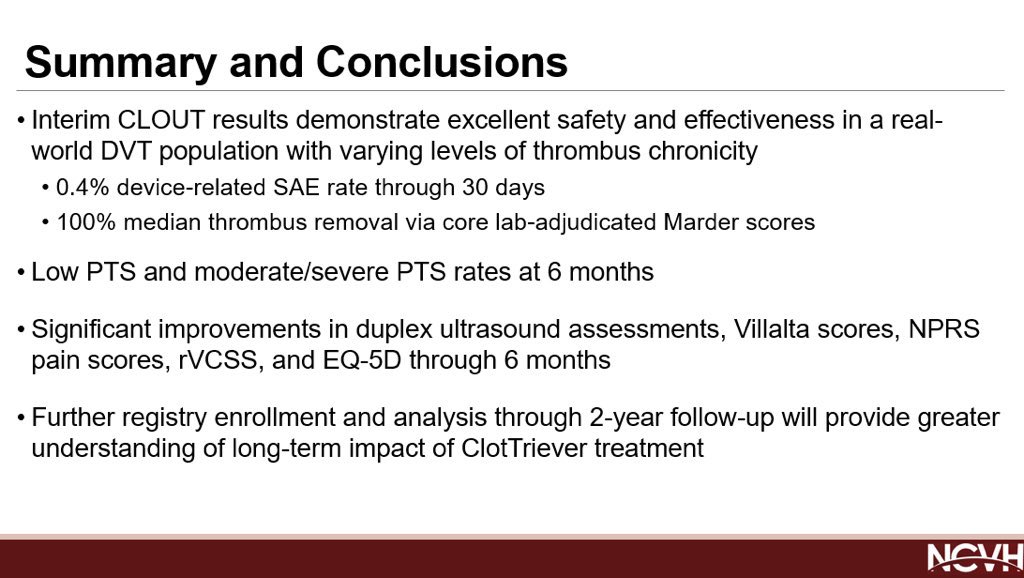
20/ CLOUT- 30-day f/u, the number of patients with PTS had significantly decreased (P<0.01). Additionally, quality of life scores ( Villalta, revised Venous Clinical Severity, EQ-5D, and Numeric Pain Rating Scale), showed statistically significant improvement at 30 days. #VTE 
21/ No major trials for @PenVascular in the acute DVT space, but hopefully one is coming ⚡️and will hopefully continue to support mechanical thrombectomy for ilofemoral DVT #VTE 

22/ So how do you pick?
Inari- good for prox DVT; has a role in chronic tx
Penumbra- can be used for soft thrombus; has a role to tx distal inflow segments
CDT- Allows for pre treatment of clot, in my mind is now an adjuvant therapy to thrombectomy.
Guidelines are mixed
Inari- good for prox DVT; has a role in chronic tx
Penumbra- can be used for soft thrombus; has a role to tx distal inflow segments
CDT- Allows for pre treatment of clot, in my mind is now an adjuvant therapy to thrombectomy.
Guidelines are mixed

23/ In all reality, there still is no consensus for the best treatment option.
I think if you want to treat venous disease you need to be well versed in all available options for treatment.
At the end of the day we need to use the technology we have to do what’s best for pts
I think if you want to treat venous disease you need to be well versed in all available options for treatment.
At the end of the day we need to use the technology we have to do what’s best for pts
24/ There is still a lot of work to do in this space. We are now only realizing that patients benefit from escalation of care and also that certain modalities (i.e #IVUS) are essential in order to achieve good outcomes. #VTE #DVT 

24/ I hope this review was beneficial for many of you new to the venous disease space. As a #cardiologist I urge all you #fellows and new attendings to embrace this space and help us push the field forward with new developments.
25/ I wish I had more exposure to #DVT treatment as a fellow. So over the next few months I am going to cover a few more high yield topics for all those interested! Stay tuned! #Vte #Clottwitter #cardiotwitter #irad #vascular #venous #DVT #PE
@NadeenFaza @bcostelloMD @CMichaelGibson @DocSavageTJU @pravinp8 @hpatel824 @onco_cardiology @DocStrom @venkmurthy @SureshSharmaMD @MusaSharkawi @Rahul2282Sharma @NirmanBhatia @ekgpdx @RezaEmaminia @echocardiac @ASE360 @robertomlang @ChinnaiyanMD @purviparwani
@PinakShahMD @Pooh_Velagapudi @DrMarthaGulati @mmamas1973 @MDMankad @SVRaoMD @dr_chirumamilla @willsuh76 @DrSuzyFeigofsky @rwyeh @yourheartdoc1 @DrJRicci @iamritu @DeeDeeWangMD @DrCJBradley @AkhilNarangMD @tarun_jain93 @maquinonesmd @agtruesdell @jameschilee @KhandelwalMD
@HeartOTXHeartMD @sarahhudsonuk @avolgman @rahatheart1 @DavidWienerMD @SunnyVMD @MonSangh @FeelingThePulse @AChoiHeart @AkshitSharmaMD @adcaTicTocDoc @jeredcookmd @RezaEmaminia @MartyTamMD @True_EP @sheelakrishmd @skilicmd @ekgpdx @chadialraies @mirvatalasnag
@jameschilee @Babar_Basir @DrHooksDO @chadialraies @ZaherFanari @motownpaesano @GindiRyan @AKassier @AlQarqazM @BobRabbaniMD @SachinParikhMD @TiberioFrisoli @DrAdaStefanescu @dr_chirumamilla @noshreza @UjjwalRastogiMD @majazayeri @SanChris999 @skilicmd
@rajdoc2005 @VMJ_SVM @TopHeartDocs @SVM_tweets @UoMVascSurgery @AorticDissectUS @escardio @ACCinTouch @MichiganACC @EricTopol @GARCIAEDINSON95 @yourheartdoc1 @drjohnm @Medscape @JAMACardio @InvasiveCardiol @cardioPCImom @ferdikiem @keaglemd @JACCJournals @CardiacConsult
@trivaxheartmd @CVCTForum @AbbottNews @HeartFailureTip @heartdocandcrew @HeartDocSharon @heartdoc101 @Heartdoc530 @heartdoc32 @cardioPCImom @JAMACardio @CN_publishing @CardioBot @TomLuscher @CardioMEMS @MedEdChat @CCMedEd @MedEduLab @MedEd_Journal @MedEdConference
@Dr_DanMD @GARCIAEDINSON95 @RonaldWinokurMD @DrYanLiu @RonaldWinokurMD @MarquandPatton @DrAmatangelo @alaa_gabi @bchTicTocDoc @cardioPCImom @CanucksFan80 @RBP0612 @ReentrantDani @ChiznerRyan @ManualOMedicine @grepmeded @TheVeggieMD @pfarrugiamd
@majazayeri @AjayPMD @GuruKowlgi @JorgeP15 @phil_wiener @ZainAsadEP @AmrFBarakat @m_ahsan7 @ShanbhagAnusha @DrDapo @RaidSaco @ikutkutMD @DrDHarmon @AlaMohsen87 @RankaSagar @Nidhi_Madan9 @SaidAshrafMD @AKassier @StrobelAaron @maniaconboard @varda88 @singamnv
@SivaTaduru @ShivtejKaushal @RickyHansra @aniket_rali @MohitpahujaMD @AdnanKhalifMD @JZArnautovic @ykmedicine777 @NehaMantri_MD @tednfs @Shanti27 @jaideeppatelmd
• • •
Missing some Tweet in this thread? You can try to
force a refresh