1/5 A 78 yo F with no prior medical history p/w progressive pill-rolling tremor, shuffling gait, and dizziness upon standing. She takes no meds. Orthostatics are ➕. What is the likely cause of her orthostatic hypotension?
#MedTwitter #MedEd #FOAMEd #GeriTwitter #NeuroTwitter
#MedTwitter #MedEd #FOAMEd #GeriTwitter #NeuroTwitter
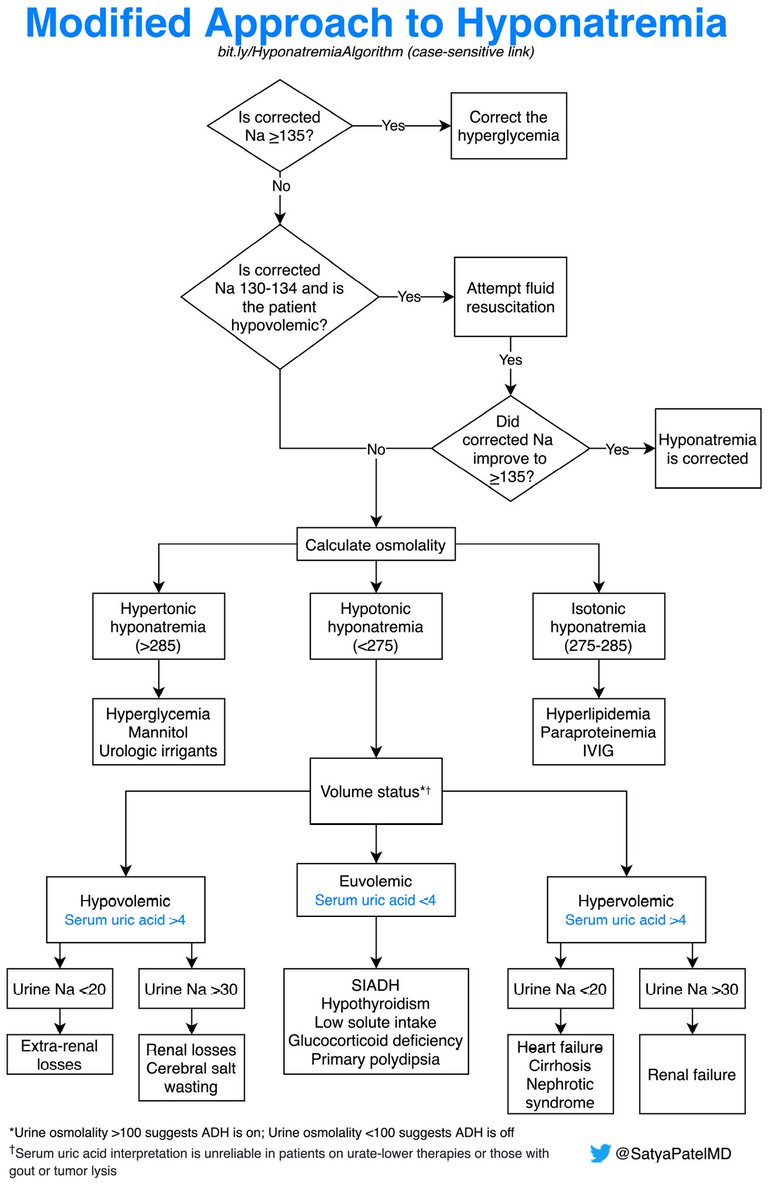
2/5 The answer is Parkinsonism! Parkinsonism is a synucleinopathy (the protein alpha-synuclein accumulates in neurons and glia) leading to autonomic dysfunction. Review this approach on orthostatic hypotension here:
https://twitter.com/SatyaPatelMD/status/1417493742768902144?s=20. Let's keep going.
3/5 She is diagnosed with Parkinsonism, and started on carbidopa-levodopa BID with improvement in symptoms. Her family has hired 24/7 caregivers who ensure her PO intake is adequate.
4/5 She continues to have dizziness that is worse than before and has started falling. She has been having witnessed episodes of fainting w/o head trauma. Orthostatic vital signs are markedly ➕ with supine hypotension. What is the likely cause?
5/5 The answer is carbidopa-levodopa! Levodopa worsens orthostatic hypotension via splanchnic vasodilation and ⬇️ supine BP through a central mechanism in a dose-dependent fashion. These BP fluctuations can be avoided by splitting the total daily dose into more frequent doses!
• • •
Missing some Tweet in this thread? You can try to
force a refresh