1/9 You admit a patient overnight with hyponatremia and you diagnose it as SIADH. But how are you going to manage it?
To review how to diagnose SIADH, check out the volume-based or ADH/RAAS-based approaches below.
#MedEd #FOAMed #MedTwitter #NephTwitter #Tweetorial


To review how to diagnose SIADH, check out the volume-based or ADH/RAAS-based approaches below.
#MedEd #FOAMed #MedTwitter #NephTwitter #Tweetorial
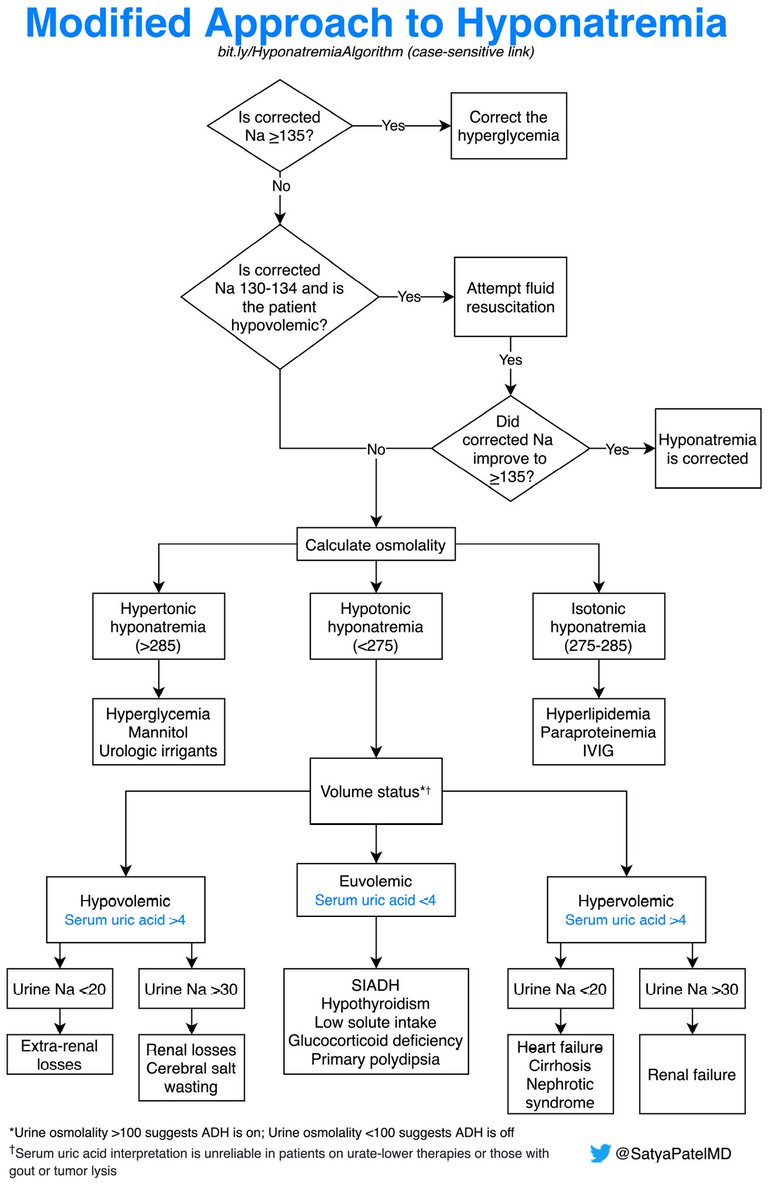


2/9 The cornerstone of treatment is to treat the underlying cause. Everything else is just a 🩹. It can sometimes be very hard to treat the underlying cause immediately (assuming you can identify it). 

3/9 Free water restriction is going to help (to a certain degree), but make sure that it’s feasible for the patient (they often need to do this beyond hospitalization). Consider restricting 500 cc below their 24-hour urine output:
https://twitter.com/edgarvlermamd/status/756197181468663808?s=20
4/9 But what about in the first 24 hours of hospitalization? I arbitrarily do 1-1.5L restriction. Remember that the food the patient receives also has free water (that is quite difficult to quantify). 

5/9 Let’s move onto 🧂. What dose should you order? It depends on the following questions:
1️⃣ How low is the Na?
2️⃣ Are they at risk for volume overload?
I start with NaCl 1g PO TID.
1️⃣ How low is the Na?
2️⃣ Are they at risk for volume overload?
I start with NaCl 1g PO TID.

6/9 Next up we have urea powder. To read more about it: cjasn.asnjournals.org/content/13/11/…).
Start with 15g PO daily.
Start with 15g PO daily.

7/9 Next we have 0.9% NS (wait, I thought we started using LR for most things these days?). It’s a process called desalination:
For more reading: doi.org/10.1093/qjmed/…
https://twitter.com/edgarvlermamd/status/756555997993369600?s=20
For more reading: doi.org/10.1093/qjmed/…

9/9 Here is a summary slide of all the options to manage SIADH – hope this helped! Feedback is always welcome. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh