1/7 Considering how to manage community-acquired pneumonia (CAP)? Is it CURB-65 or should it be CARB-65? No idea what I am talking about? Let's talk about azotemia and uremia!
#MedTwitter #FOAMEd #MedEd #NephTwitter #IDTwitter
#MedTwitter #FOAMEd #MedEd #NephTwitter #IDTwitter
2/7 The CURB-65 score has been used for diagnosis and treatment of adults with community-acquired pneumonia (CAP). The most recent IDSA CAP guidelines in 2019 (pubmed.ncbi.nlm.nih.gov/31573350/) referenced the 2007 IDSA CAP criteria for defining severity 
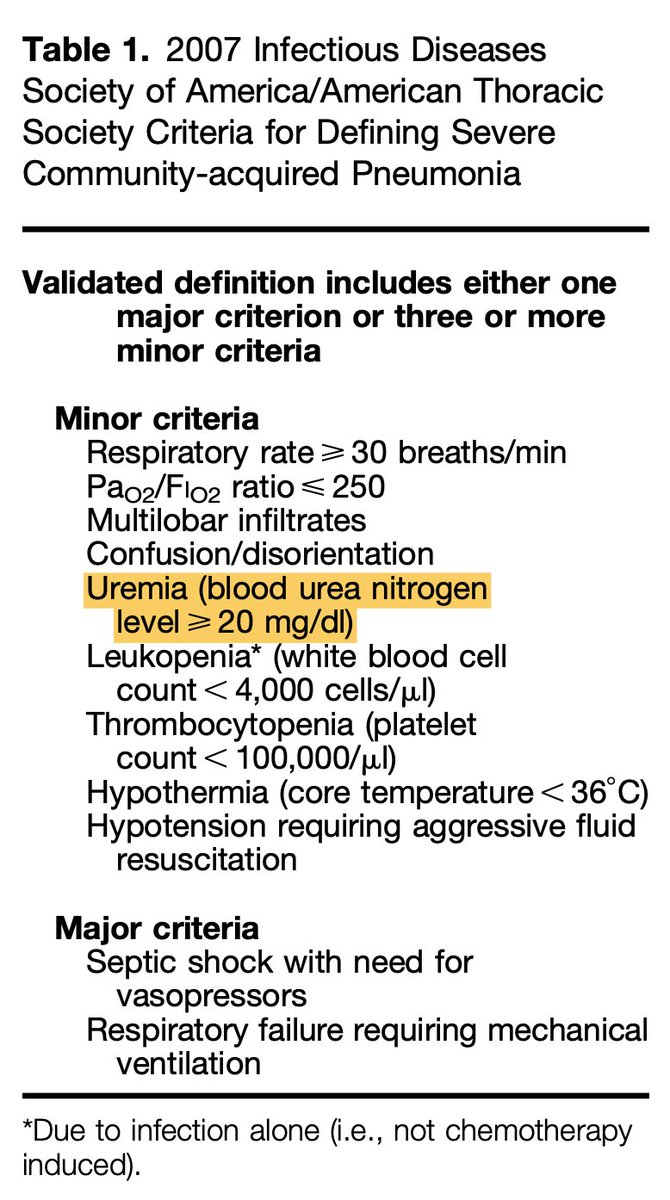
3/7 The original article that describes validation of the CURB scoring system (ncbi.nlm.nih.gov/pmc/articles/P…) does NOT use the word "uremia," but instead references an serum urea level cutoff. 

4/7 In the past, the term “uremia” was simply used to describe an elevated serum urea level. However, its use is now typically reserved for a clinical syndrome that is the result of this lab abnormality (jasn.asnjournals.org/content/25/10/…) 



5/7 For clarity:
💥 Azotemia = ⬆️ urea level
💥 Uremia = Azotemia + clinical syndrome from ⬆️ urea level
Why does this nomenclature even matter?
💥 Azotemia = ⬆️ urea level
💥 Uremia = Azotemia + clinical syndrome from ⬆️ urea level
Why does this nomenclature even matter?
6/7 "Confusion" and "⬆️ Urea level" are individual components of CURB-65. By calling it uremia, you risk "double dipping" in the CURB-65 score. Additionally, confusion is a separate minor criterion in the new CAP guidelines.
7/7 You may think that calling it azotemia is semantics, but if not appropriately categorized, we can inappropriately stratify someone in the wrong tier of disease severity. So, which team are you on now?
• • •
Missing some Tweet in this thread? You can try to
force a refresh