#MASTERDAPT is out in @NEJM, short vs standard DAPT in high bleeding risk patients. Will be the most important DAPT Study we see this year. Much respect for the authors. Here’s are some quick thoughts (thread):
- high risk patients (1/3 NSTEMI, 11% STEMI, complex long lesions)
- high risk patients (1/3 NSTEMI, 11% STEMI, complex long lesions)
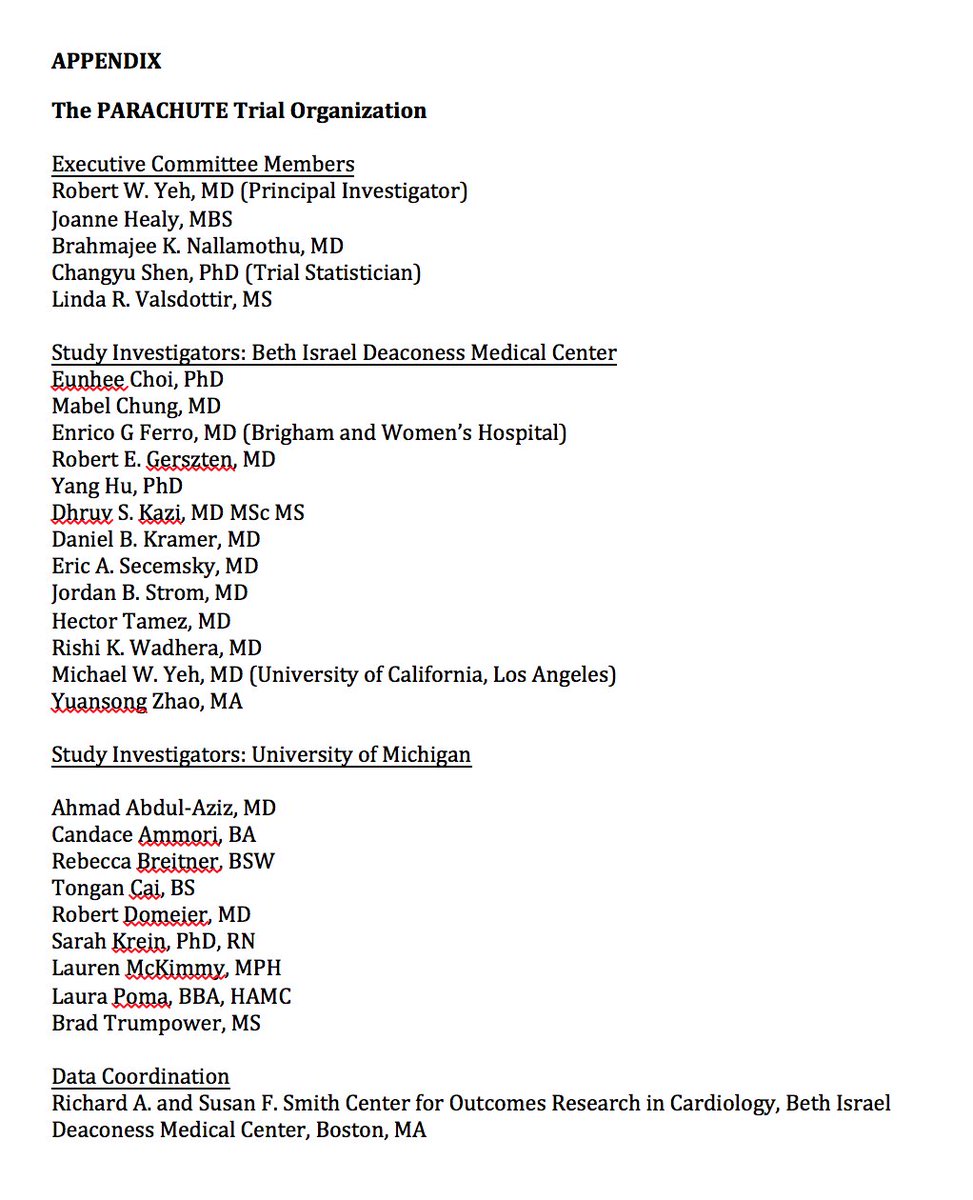
- OAC patients standard regimen has at least 3 months and sometimes longer of triple therapy. OAC short regimen got 1 month triple and stopped all antiplt therapy by 6 months.
- non OAC stratum majority of short regimen went to P2Y12 monotherapy with clopidogrel at 1 month.
- non OAC stratum majority of short regimen went to P2Y12 monotherapy with clopidogrel at 1 month.
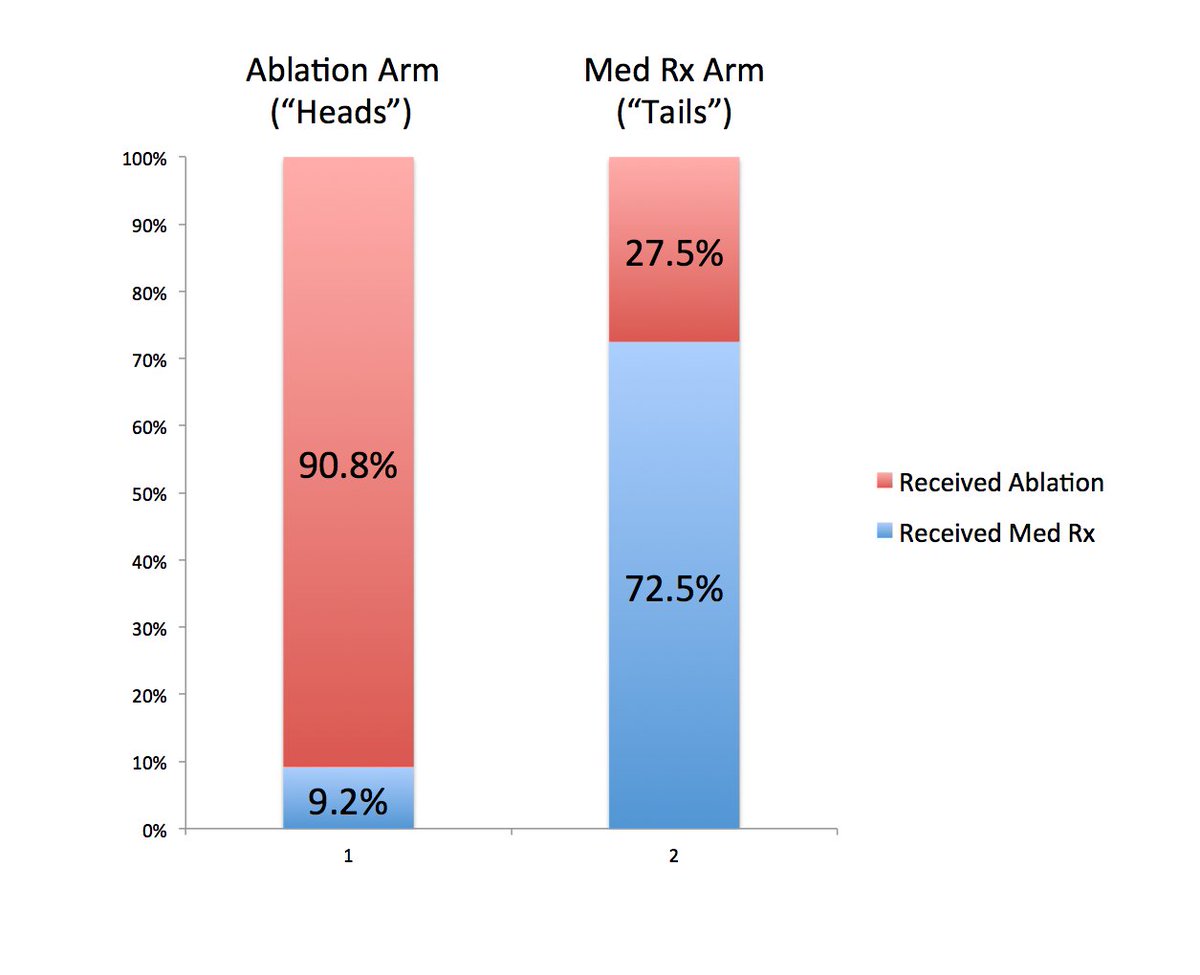
Per protocol non inferiority test for combined NACE endpoint, then combined MACE endpoint, then ITT superiority test for safety (BARC 2-5 bleeding).
Major results are below. Short DAPT was non inferior for NACE and MACE, superior for bleeding.
Major results are below. Short DAPT was non inferior for NACE and MACE, superior for bleeding.

Events rates were lower than anticipated, which makes achieving NI easier using this fixed margin approach for the first 2 endpoints. But looking at the point estimates and CIs, still a strong result favoring shorter DAPT on average.
OAC subgroup analysis in appendix is critical. One wonders how much of the NACE/bleeding findings driven by triple therapy for longer duration than most typically do. These are very underpowered but can start to see some signals but not necessarily a clear picture. 


High vs low DAPT Score subgroup is suggestive that high dapt score patients might be a subgroup that benefits form longer DAPT, pointing to a qualitative interaction. Underpowered but signal is consistent over many studies per @NinoNJ paper:
pubmed.ncbi.nlm.nih.gov/33111495/
pubmed.ncbi.nlm.nih.gov/33111495/
Bleeding differences driven by BARC 2 bleeding alone. BARC 3-5 no different.
Numerical differences also in stent thrombosis and MI (underpowered), favoring standard DAPT as would be expected. There’s no free lunch, just is a question of how cheap the lunch is, so to speak.
Numerical differences also in stent thrombosis and MI (underpowered), favoring standard DAPT as would be expected. There’s no free lunch, just is a question of how cheap the lunch is, so to speak.
how could the NACE event rates be lower than bleeding rates when the NACE event rate INCLUDES the same bleeding endpoint?
Suspect this is due to to the cause specific KM curve used for bleeding against high death rate background.
See here: pubmed.ncbi.nlm.nih.gov/29997149/
Suspect this is due to to the cause specific KM curve used for bleeding against high death rate background.
See here: pubmed.ncbi.nlm.nih.gov/29997149/
Takeaway there is that you may not be able to look at the bleeding ARR and convert that to an applicable NNT for your patients, would love to see what the cumulative incidence function curves for bleeding look like instead, as well as curves that allow for repeated events.
Overall, incredibly impressive work, potentially practice changing. Makes me much more likely to use P2y12 monotherapy early in HBR patients not going on OAC (esp low DAPT Score), and also stop all APT in OAC patients at 6 months which I had not done previously. End
Davide @DFCapodanno has the better explanation for the differences between the endpoint rates.
https://twitter.com/DFCapodanno/status/1431666856927039494
• • •
Missing some Tweet in this thread? You can try to
force a refresh