I'm not an immunologist, but I've been trying to read into the literature on waning immunity to SARS-CoV-2 and to understand the recent NIH, CDC, FDA booster recommendation (hhs.gov/about/news/202…). I'll share some takeaways here. 1/14
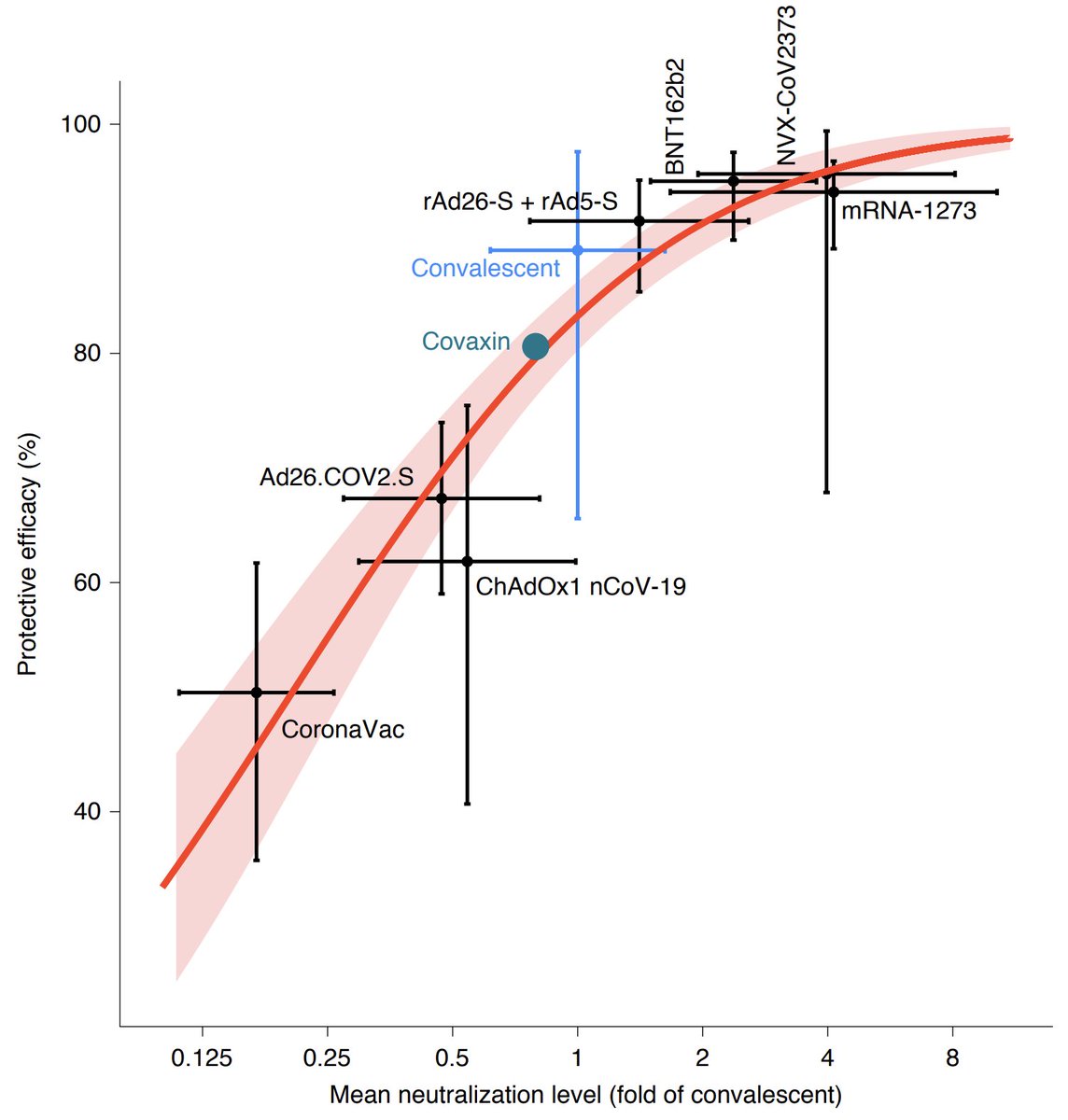
Previous studies in other viruses found that the potency and the concentration of circulating antibodies in an individual is often predictive of their protection to infection or illness after exposure. 2/14
This potency + concentration is commonly quantified as the titer required to neutralize 50% of viral plaques in a lab assay. These assays are run by diluting sera from an individual and seeing what dilution causes loss of neutralization. 3/14
If you look at neutralization titers after immunization by either mRNA vaccine you'll see modest titers after the first dose, but substantial titers after the second dose. 2-4 weeks after second dose titers begin to decline (Doria-Rose et al nejm.org/doi/full/10.10…). 4/14 

The phase 3 trials had most endpoints collected between in the initial ~2-3 months after second doses were given, during which time titers would have been near their peak. 5/14
Gilbert et al (medrxiv.org/content/10.110…) looks at the degree to which an individual's titer during the Moderna phase 3 trial determined their risk of acquiring symptomatic COVID-19 illness, finding that breakthrough infections were associated with lower titers. 6/14 

A similar relationship is observed between average titer generated by a particular vaccine and its measured efficacy (Khoury et al nature.com/articles/s4159…), further suggesting that neutralization titer can be used to predict degree of protection from symptomatic illness. 7/14 
The question becomes whether a ~5-fold reduction in titer 6 months after second dose is enough to impact vaccine effectiveness. @IsraelMOH looks at this directly by measuring incidence in individuals vaccinated at different dates (figure by @FT ft.com/content/23cdbf…). 8/14 

There may be other confounders here, but the critical one of age is directly controlled for by looking at incidence and vaccination date across age groups. Also, keep in mind that the unvaccinated cohort contains individuals with immunity through natural infection. 9/14
Importantly, @IsraelMOH observes a large difference between symptomatic illness and hospitalization, where protection against symptomatic illness waned, while protection against hospitalization remained robust (figure from slide deck gov.il/BlobFolder/rep…). 10/14 

This result of differential waning between symptomatic illness and severe illness is replicated by Tartof et al (papers.ssrn.com/sol3/papers.cf…) looking at outcomes in a Kaiser Permanente cohort. 11/14 

Work by @rishirajgoel et al (biorxiv.org/content/10.110…) identifies a potential mechanism in which although antibody responses partially wane over 6 months, memory B cell responses show more durability. 12/14 

Memory response kicking in after breakthrough infection would explain results from Chia et al (biorxiv.org/content/10.110…) and from @StephenKissler et al (medrxiv.org/content/10.110…) showing that viral load declines more rapidly in vaccinated individuals. 13/14 



Even if protection against severe outcomes remains robust, observed waning suggests that boosters will be necessary to reduce circulation. Delta has generated a late summer wave, but steady state is likely a winter "COVID season" with vaccination recommended beforehand. 14/14
• • •
Missing some Tweet in this thread? You can try to
force a refresh