ID proponents of surgical masking on COVID wards, often site a handful of systematic reviews to defend their position.
Spurred by @AntibioticDoc's thread and @McDevonMD's tweet below - I did some digging.
Was MacIntyre 2013 covered in these reviews, and if so, how?
🧵1/17
Spurred by @AntibioticDoc's thread and @McDevonMD's tweet below - I did some digging.
Was MacIntyre 2013 covered in these reviews, and if so, how?
🧵1/17
https://twitter.com/McDevonMD/status/1451744671655501829
First, let's review @Globalbiosec's MacIntyre 2013.
This RCT had 3 arms: 1) continuous surgical masks 2) continuous N95s 3) targeted N95s (worn only during high-risk procedures and AGPs)
The 3rd arm is testing the status quo at most hospitals.
2/17
atsjournals.org/doi/full/10.11…

This RCT had 3 arms: 1) continuous surgical masks 2) continuous N95s 3) targeted N95s (worn only during high-risk procedures and AGPs)
The 3rd arm is testing the status quo at most hospitals.
2/17
atsjournals.org/doi/full/10.11…


MacIntyre 2013 found that continuous N95 use resulted in a statistically significant reduction in Clinical Respiratory Illness (CRI), whereas targeted/intermittent N95 use was not superior to medical masks.
This is not surprising given the nature of aerosol transmission.
3/17


This is not surprising given the nature of aerosol transmission.
3/17



So... wait a minute... if we have an RCT from 2013, that shows continuous N95s are significantly protective against Clinical Respiratory Illness (CRI) - why are all these ID doctors saying there is no evidence to support N95 use?
Time to check the systematic reviews..
4/17
Time to check the systematic reviews..
4/17
Let's start with the authoritative Jefferson 2020 systematic review, with Alberta's Dr. Conly as the 2nd author.
This review pools 3 N95 RCTs, and concludes no clear difference between surgical masks and N95s to reduce respiratory viral infection.
5/17
cochranelibrary.com/cdsr/doi/10.10…
This review pools 3 N95 RCTs, and concludes no clear difference between surgical masks and N95s to reduce respiratory viral infection.
5/17
cochranelibrary.com/cdsr/doi/10.10…
So did they include MacIntyre 2013?
Yes they did!
Here's what they pooled in their meta-analysis:
1) MacIntyre 2011 - Continuous N95
2) MacIntyre 2013 - Continuous N95
3) MacIntyre 2013 - Targeted/intermittent N95
4) Radonovich 2019 - "Close contact" N95
6/17

Yes they did!
Here's what they pooled in their meta-analysis:
1) MacIntyre 2011 - Continuous N95
2) MacIntyre 2013 - Continuous N95
3) MacIntyre 2013 - Targeted/intermittent N95
4) Radonovich 2019 - "Close contact" N95
6/17


Note they pooled BOTH the continuous arm AND the targeted arm of MacIntyre 2013.
Remember, the targeted arm only used N95s during high-risk procedures and AGPs.
This arm was included in MacIntyre's study, to show the status-quo isn't sufficient.
7/17

Remember, the targeted arm only used N95s during high-risk procedures and AGPs.
This arm was included in MacIntyre's study, to show the status-quo isn't sufficient.
7/17
https://twitter.com/LeylaDAsadi/status/1452308295700647940?s=20

In addition, they pooled Radonovich 2019, with a 41% weight. This study is even more problematic - the N95s and Surgical Masks were only worn in "close contact", ie. within 6ft of patients with suspected respiratory illness.
8/17



8/17
https://twitter.com/CPita3/status/1451771507546509314?s=20



In summary, they pooled 4 arms from 3 studies, 2 of which were certain to fail in protecting against aerosol inhalation.
The 2 continuous N95 arms (MacIntyre 2011 and 2013) DID find a significant reduction in CRI, but those results were diluted in the meta-analysis.
9/17
The 2 continuous N95 arms (MacIntyre 2011 and 2013) DID find a significant reduction in CRI, but those results were diluted in the meta-analysis.
9/17
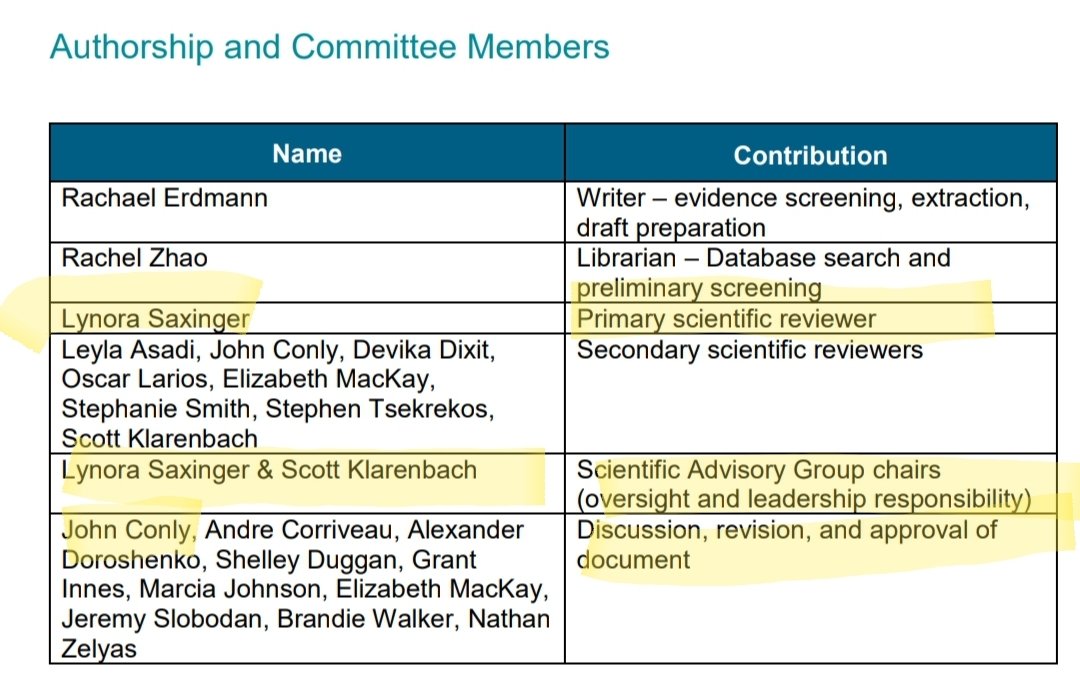
Next, let's look at @AHS_media Scientific Advisory Group's Rapid Evidence Review on COVID-19 PPE Guidelines from Dec 2020.
This review heavily references the above Jefferson Systematic Review, but also summarizes the specifics in MacIntyre 2013.
10/17
albertahealthservices.ca/assets/info/pp…
This review heavily references the above Jefferson Systematic Review, but also summarizes the specifics in MacIntyre 2013.
10/17
albertahealthservices.ca/assets/info/pp…

It falsely states that MacIntyre 2013 found NO statistically significant differences between continuous N95 and continuous masking for clinical respiratory illness. It then references an RR of 0.70 (95% CI 0.35 - 1.40).
Compare to what MacIntyre 2013 actually said.
11/17


Compare to what MacIntyre 2013 actually said.
11/17



So where did that RR of 0.7 (95% CI 0.35 = 1.4) come from, if not from MacIntyre?
Turns out, it came from the Jefferson/Conly review - only they took the RR for the TARGETED N95 arm, while referring to the CONTINUOUS N95 arm in the text.
A pretty egregious WHOOPSIES!
12/17

Turns out, it came from the Jefferson/Conly review - only they took the RR for the TARGETED N95 arm, while referring to the CONTINUOUS N95 arm in the text.
A pretty egregious WHOOPSIES!
12/17


But wait... THERE'S MORE!
Dr. Conly recently released a correspondence in The Lancet, rebuking Dr. MacIntyre's calls for Continuous N95 use on COVID wards.
What does he reference? His own Jefferson systematic review, and another systematic review.
13/17
thelancet.com/journals/lance…
Dr. Conly recently released a correspondence in The Lancet, rebuking Dr. MacIntyre's calls for Continuous N95 use on COVID wards.
What does he reference? His own Jefferson systematic review, and another systematic review.
13/17
thelancet.com/journals/lance…

The second systematic review is Bartoszko/Loeb 2020. (You will recognize Loeb from the N95 RCT being run with nurses in COVID-19 wards in Canada)
Surely this review contains some convincing evidence to show N95s aren't superior to surgical masks?
14/17
onlinelibrary.wiley.com/doi/10.1111/ir…
Surely this review contains some convincing evidence to show N95s aren't superior to surgical masks?
14/17
onlinelibrary.wiley.com/doi/10.1111/ir…
Nope.. this systematic review performs an almost identical meta-analysis to Jefferson.. pooling the SAME 3 studies, in the SAME problematic way.
Just like Jefferson, it heavily weights the "close contact" Radonovich trial, and includes the targeted N95 arm from MacIntyre.
15/17
Just like Jefferson, it heavily weights the "close contact" Radonovich trial, and includes the targeted N95 arm from MacIntyre.
15/17

Reading through all of this left me feeling both incredulous and defeated. Our Canadian (and global) Infectious Disease Evidence Based Medicine empire, which is driving critical PPE decisions during a deadly, Airborne Pandemic, is teetering upon this rickety house of cards.
16/17
16/17
I think a good parallel to these systematic reviews, is the Subprime Mortgage Crisis - where banks packaged risky subprime mortgages into layered & increasingly obfuscated securities. At the top, the securities were rated AAA, but they were all based on the same junk.
end/
end/
• • •
Missing some Tweet in this thread? You can try to
force a refresh