
Pt with advanced Cirrhosis
AKI, Oliguria + Encephalopathy
Initial treatment = Albumin + Lactulose enemas
🧂Na is now 158 (From Lactulose induced free water loss)
#POCUS ninja @tumleal noticed something was wrong! He got his probe and texted me
📱 #WhatsAppAKIConsult 1/5

AKI, Oliguria + Encephalopathy
Initial treatment = Albumin + Lactulose enemas
🧂Na is now 158 (From Lactulose induced free water loss)
#POCUS ninja @tumleal noticed something was wrong! He got his probe and texted me
📱 #WhatsAppAKIConsult 1/5


#POCUS: Plethoric non collapsible IVC
Based on the clinical scenario, IVC, heart rate and Pulse Pressure...
What is the likely underlying pathophysiology? 2/5
Based on the clinical scenario, IVC, heart rate and Pulse Pressure...
What is the likely underlying pathophysiology? 2/5
@tumleal went ahead and confirmed his suspicion:
He 📲texted me this:
LVOT VTI = 38!
Some 🔢:
VTI of 38, assuming a LVOT diameter of 20 mm: Stroke Volume = 119 ml
119 ml x HR (93 bpm) = 11.1 L/min of CO!
This is High Output Heart Failure (Very common in Cirrhosis) 3/5

He 📲texted me this:
LVOT VTI = 38!
Some 🔢:
VTI of 38, assuming a LVOT diameter of 20 mm: Stroke Volume = 119 ml
119 ml x HR (93 bpm) = 11.1 L/min of CO!
This is High Output Heart Failure (Very common in Cirrhosis) 3/5
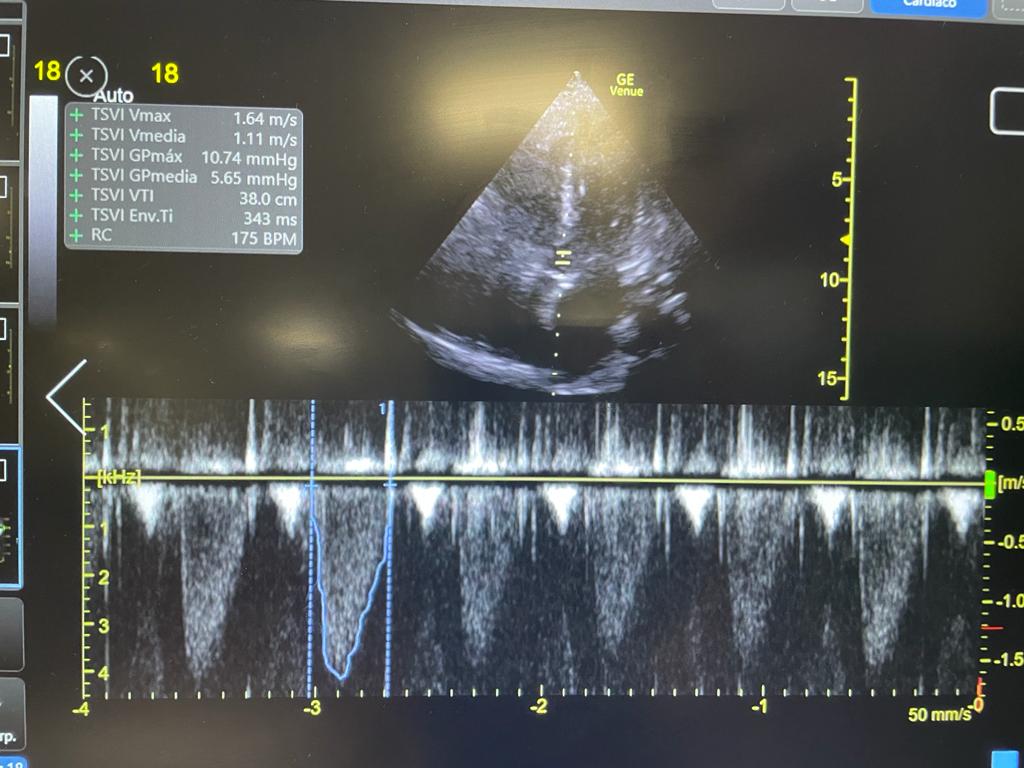

⬆️ pulse pressure suggested ⬆️ Stroke Volume. This + Tachycardia meant High Cardiac Output!
This was confirmed by #POCUS (great job @tumleal)
The cause of High Output Heart Failure (HOHF) is low peripheral vascular resistance
More on HOHF here:
4/5
This was confirmed by #POCUS (great job @tumleal)
The cause of High Output Heart Failure (HOHF) is low peripheral vascular resistance
More on HOHF here:
https://twitter.com/ArgaizR/status/1431693225446809600?s=20
4/5
Treating the underlying cause (vasodilation) with vasopressors would likely increase renal perfusion, urine output and help the kidney get rid of extra sodium (hypervolemic hypernatremia)
This actually happened! UOP, AKI and hypernatremia resolved with pressors!
/END
This actually happened! UOP, AKI and hypernatremia resolved with pressors!
/END

• • •
Missing some Tweet in this thread? You can try to
force a refresh
















