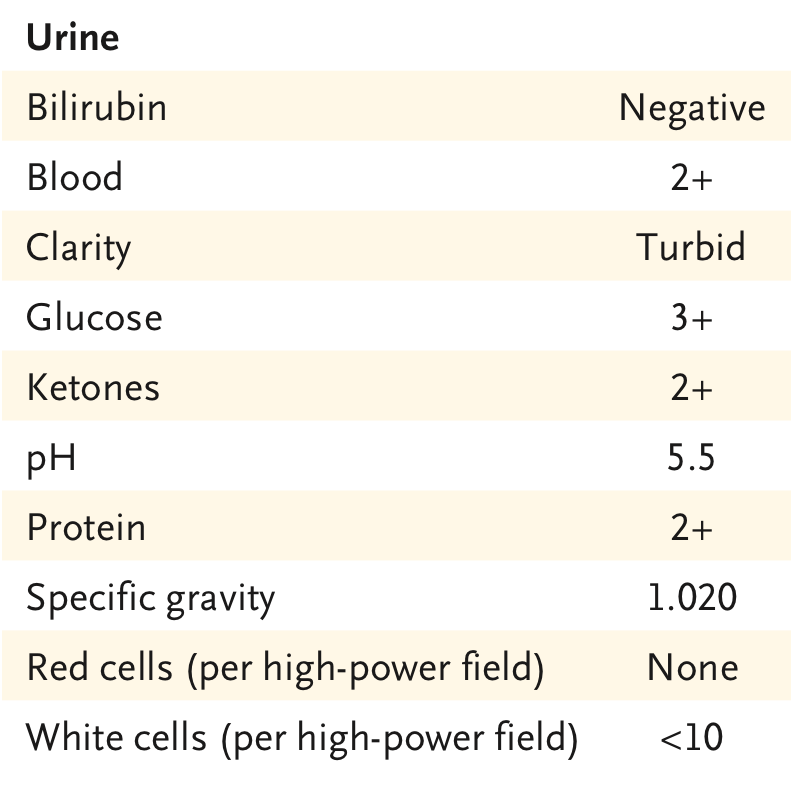
AKI Consult: 👵 ➡️ ED with severe DKA. CT Abdomen and Chest to look for infectious trigger: negative. Tx with IV insulin and balanced crystalloid + 6 L with obvious improvement. Cr was 2.7
Remained oliguric, now in sudden shock with increasing NE dose (0.5 ucg/kg/min) 🚨 1/12


Remained oliguric, now in sudden shock with increasing NE dose (0.5 ucg/kg/min) 🚨 1/12



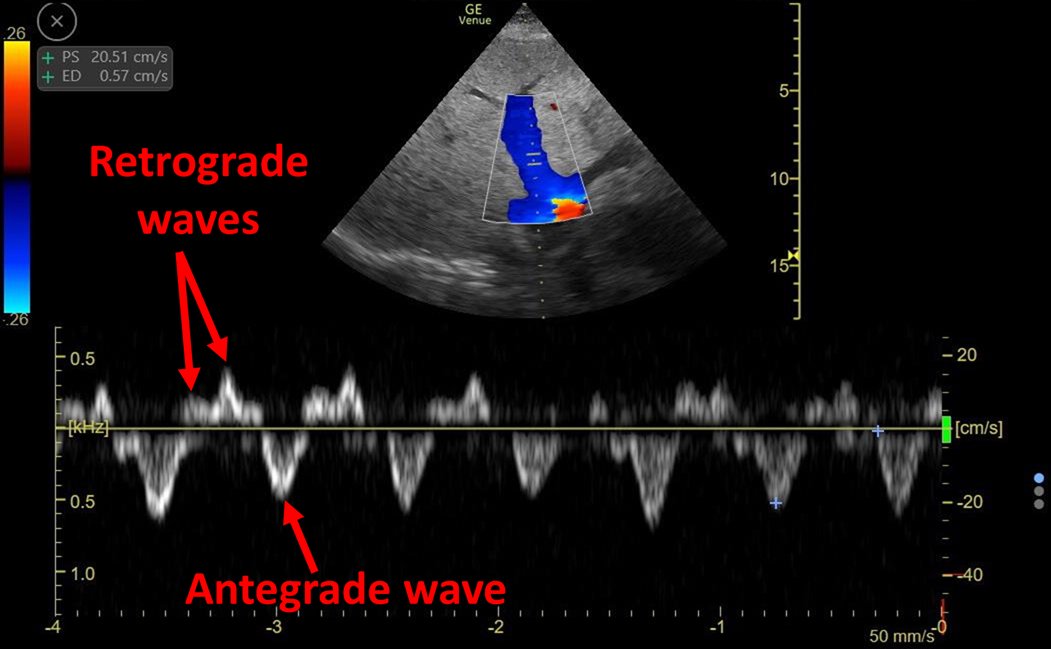
#POCUS Very hyper-dynamic🫀 with increased contractility and no RV dysfunction.
🔎 Look carefully at color of flow exiting the LV:
Aliasing (green color): This means ultrasound system is trying to image an event that is occurring faster than the sample rate
2/12
🔎 Look carefully at color of flow exiting the LV:
Aliasing (green color): This means ultrasound system is trying to image an event that is occurring faster than the sample rate
2/12
This means flow is fast. But how fast? Choose the CW doppler setting and find out!
In this case acceleration was almost 6 m/s!
Flow acceleration occurs in the setting of obstruction (similar to putting your finger on the hose exit)
So what is causing the obstruction? 3/12

In this case acceleration was almost 6 m/s!
Flow acceleration occurs in the setting of obstruction (similar to putting your finger on the hose exit)
So what is causing the obstruction? 3/12


Aortic stenosis is one possibility, if you look at #POCUS 👆 aortic valve looks normal.
In the setting of a hyper-dynamic LV, Dynamic Obstruction of the Left Ventricular Outflow Tract (DOLVOT) should be the first thing that comes to mind!
4/12
journals.sagepub.com/doi/10.1177/03…
In the setting of a hyper-dynamic LV, Dynamic Obstruction of the Left Ventricular Outflow Tract (DOLVOT) should be the first thing that comes to mind!
4/12
journals.sagepub.com/doi/10.1177/03…
DOLVOT can occur suddenly whenever there is
🚨Decreased LV filling volume🚨
Predisposing mechanisms:
Asymmetric septal hypertrophy
Sigmoid septum
Motion wall abnormalities (including 🐙)
Systolic anterior motion of the mitral valve (SAM)
5/12
atsjournals.org/doi/10.1513/An…
🚨Decreased LV filling volume🚨
Predisposing mechanisms:
Asymmetric septal hypertrophy
Sigmoid septum
Motion wall abnormalities (including 🐙)
Systolic anterior motion of the mitral valve (SAM)
5/12
atsjournals.org/doi/10.1513/An…

Decreased LV filling is always secondary to any of this three variables:
⬇️ Preload: Hypovolemia, Obstruction (RV failure w interdependence)
⬆️ Contractility and Heart Rate: Beta agonist, Norepinephrine
⬇️ Afterload: Sepsis
6/12
⬇️ Preload: Hypovolemia, Obstruction (RV failure w interdependence)
⬆️ Contractility and Heart Rate: Beta agonist, Norepinephrine
⬇️ Afterload: Sepsis
6/12

As such, treatment should focus on:
⬆️ Preload: Fluids.
*sometimes this is enough if the cause is hypovolemia (attached case)
⬆️ Afterload: Alfa agonists with no inotropism
⬇️ Contractility and heart rate: Beta Blockers
7/12
⬆️ Preload: Fluids.
*sometimes this is enough if the cause is hypovolemia (attached case)
⬆️ Afterload: Alfa agonists with no inotropism
⬇️ Contractility and heart rate: Beta Blockers
7/12
https://twitter.com/ArgaizR/status/1386800708909928454?s=20
In this case, even though cause was not clear, I started fluid bolus and stopped NE.
Then...the patient had abundant GI bleeding 🩸🩸🩸
We aggressively resuscitated with fluid and blood products. Patient improved immediately 8/12
Then...the patient had abundant GI bleeding 🩸🩸🩸
We aggressively resuscitated with fluid and blood products. Patient improved immediately 8/12
However, one hour later we were back at square one:
Patient was in shock again!
Did patient need more fluid? I performed #LUS: Clear B-lines. Even thought patient is still fluid responsive. She is no longer fluid tolerant!!!
I was not keen on continuing fluids... 9/12
Patient was in shock again!
Did patient need more fluid? I performed #LUS: Clear B-lines. Even thought patient is still fluid responsive. She is no longer fluid tolerant!!!
I was not keen on continuing fluids... 9/12
I ordered AngioCT to rule out active recurrent bleeding.
No bleeding.
However diverticulitis with abscess formation was diagnosed!!
Not previously seen because of lack of IV contrast 🤦♂️
10/12
No bleeding.
However diverticulitis with abscess formation was diagnosed!!
Not previously seen because of lack of IV contrast 🤦♂️
10/12

We started antibiotics and vasopressin (⬆️ afterload with no inotropism). *IV beta-blocker was not available at the moment (public hospital shortage).
Fortunately, vasopressin did the trick and patient improved and oliguria resolved! Repeat #POCUS showed DLVOTO resolution 11/12


Fortunately, vasopressin did the trick and patient improved and oliguria resolved! Repeat #POCUS showed DLVOTO resolution 11/12



🔑
💎DLVOTO is easy to diagnose (CW Doppler)
💎Norepinephrine should be avoided at all costs
💎Although these patients improve rapidly with fluid,
THIS IS NOT A PERMANENT SOLUTION
💎Treat with Phenylephrine + IV BB
Bonus: Always use IV contrast even in AKI! @PulmCrit

💎DLVOTO is easy to diagnose (CW Doppler)
💎Norepinephrine should be avoided at all costs
💎Although these patients improve rapidly with fluid,
THIS IS NOT A PERMANENT SOLUTION
💎Treat with Phenylephrine + IV BB
Bonus: Always use IV contrast even in AKI! @PulmCrit


• • •
Missing some Tweet in this thread? You can try to
force a refresh