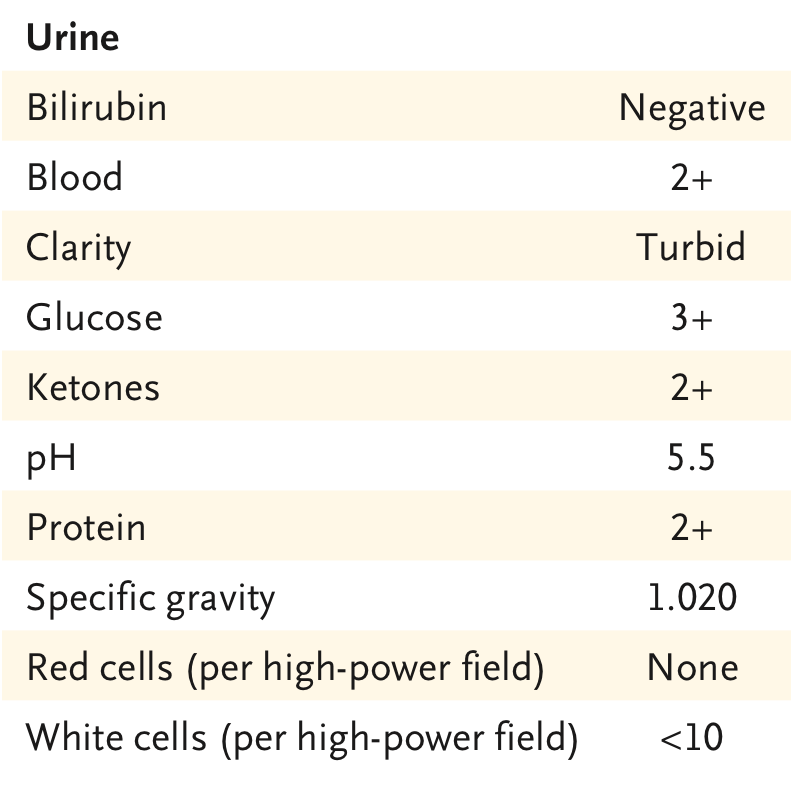
Pt w advanced liver cirrhosis. 🏥 Comes w worsening ascites. No fever🤒, no bleeding🩸. 🧠 ok, no asterixis. BP 91/50. Labs📈: AKI (Cr 3.0 mg/dl), UNa 7 mEq/L, bland sediment. #POCUS 👉small cirrhotic liver with significant ascites. Paracentesis ruled out PBE. 📊Poll below👇 1/11
What would your initial treatment be? 2/11
Don't treat reflexively. A thorough physical exam ♥️🩺revealed a systolic murmur at left lower sternal border. Neck exam 👇
Sitting Down (90º) /// Supine (45º) 3/11
Sitting Down (90º) /// Supine (45º) 3/11
Albumin for volume expansion makes no sense in the face of venous congestion. Perform a good physical exam and you might not even need #POCUS. (Where is the fun in that? 😅)
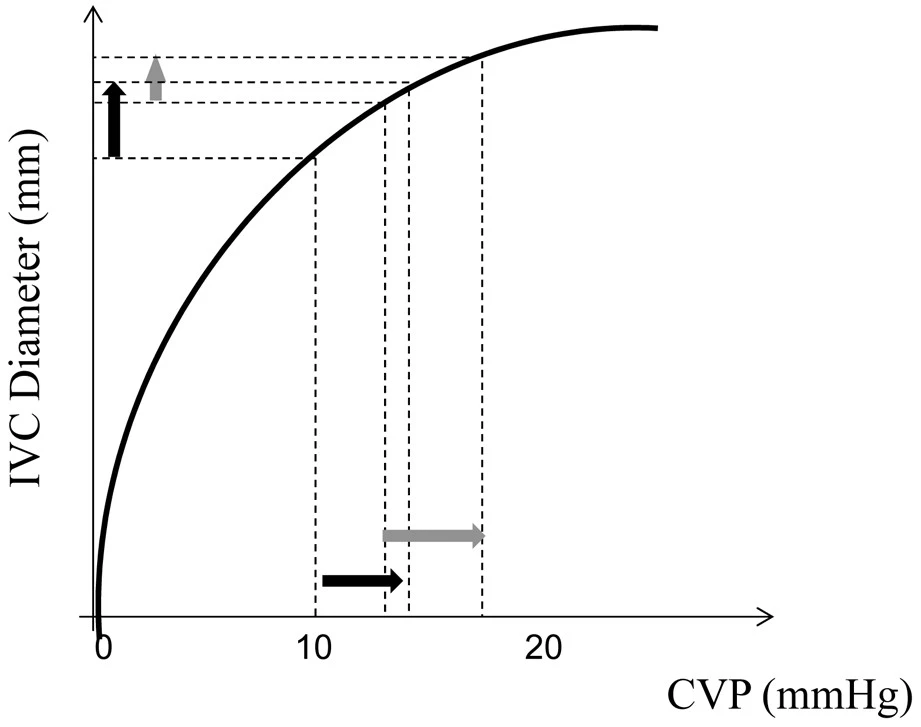
If you look closely at the first video. IVC is huge! With no inspiratory variation. 4/11
If you look closely at the first video. IVC is huge! With no inspiratory variation. 4/11

#LUS (lung ultrasound) showed A pattern (not shown) which rules out lung congestion (good LV). The ♥️ is performing OK. 👇 PLAx, PSAx, A4ch with Good LV and RV systolic function. 5/11
#Echofirst revealed moderate/severe TR (but we knew this already, didn't we?). Apical 4ch, Parasternal Short and Parasternal Long views of the RV with color shown 👇 6/11
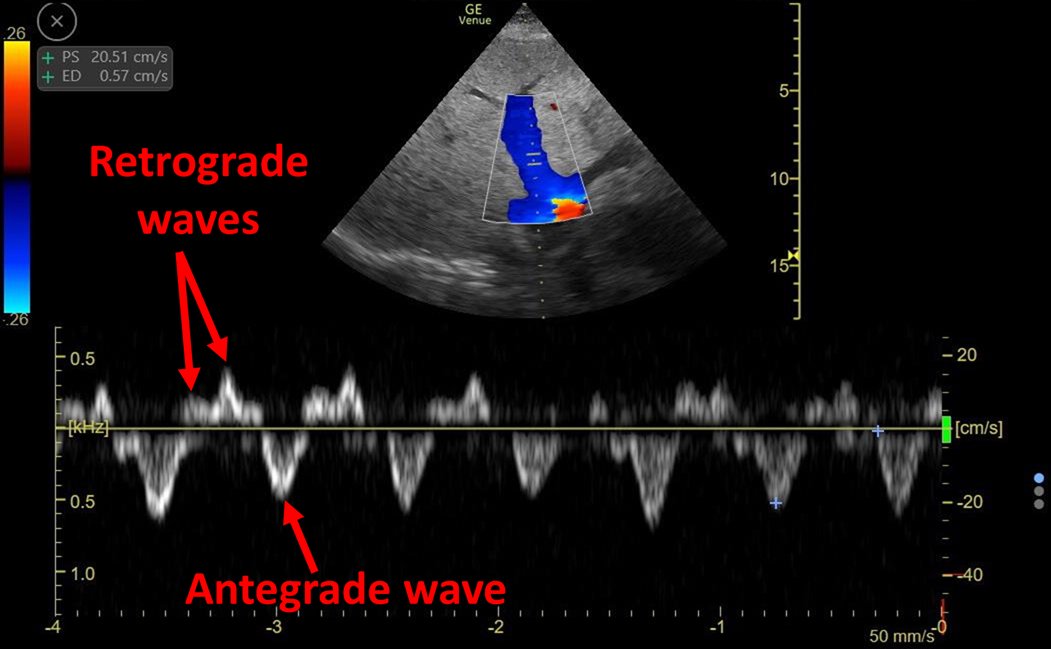
Some Doppler for the nerds: 1) TRVMax (showing moderate tricuspid regurgitation), 2) LVOT-VTI is increased (high stroke volume), 3) Normal shaped RVOT-VTI (ruling out severe precapillary PH) 4) Intra-renal venous doppler (IRVD) with biphasic pattern = venous congestion 7/11 







#POCUS confirmed physical exam!
Hemodynamic AKI, distributive type.
Hyper-dynamic heart with increased CO (low peripheral vascular resistance) + Venous congestion = High output heart failure
8/11
Hemodynamic AKI, distributive type.
Hyper-dynamic heart with increased CO (low peripheral vascular resistance) + Venous congestion = High output heart failure
8/11
Albumin and crystalloid are volume expanders. Why would we want this? This will make congestion worse. Remember volume expansion is meant to achieve an increase in cardiac output but... It is already very high!!
This quote here 👇👇👇👇
doi.org/10.1038/s41581… 9/11
This quote here 👇👇👇👇
doi.org/10.1038/s41581… 9/11

In this case, I would advise to start vasopressors early (not wait 48 hrs of futile volume expansion). In fact, this was done and patient improved rapidly with good urine output and rapid resolution of AKI. 10/11
We see this frequently, with the exact same physiology: Low BP, normal ♥️, moderate/severe functional TR, and venous congestion (plethoric IVC and altered IRVD). I wrote about a very similar case here:
criticalcarenow.com/2020/10/04/alb…
11/11
criticalcarenow.com/2020/10/04/alb…
11/11
• • •
Missing some Tweet in this thread? You can try to
force a refresh