One of my favorite and most intriguing causes of severe venous congestion (#VExUS = 3)
A 🧵on High Output Heart Failure (HOHF) 1/18
A 🧵on High Output Heart Failure (HOHF) 1/18
First, the index case:
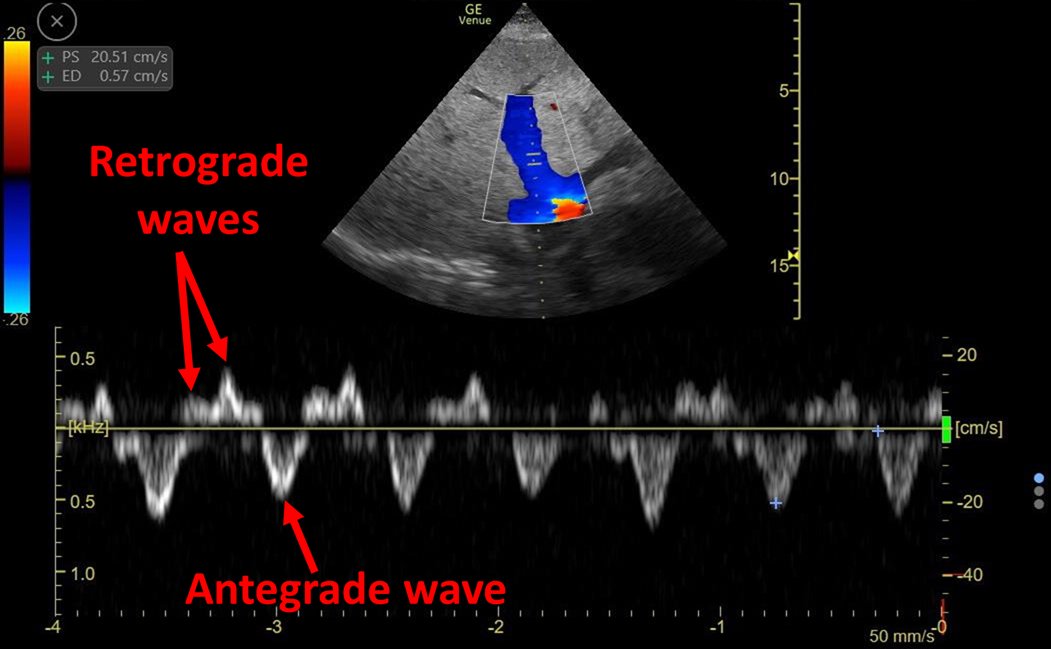
Clip above shows hyperdynamic flow from the vena cava
#echofirst 👇: Very dilated and plethoric IVC, LV OK, Dilated RV, D sign
Overall: Increased Right heart filling pressures
2/18
Clip above shows hyperdynamic flow from the vena cava
#echofirst 👇: Very dilated and plethoric IVC, LV OK, Dilated RV, D sign
Overall: Increased Right heart filling pressures
2/18
IVC = 3.4 cm
Portal Vein = > 100% pulsatility
LVOT VTI = 26
TRVmax = 3.04 m/s
So we have:
Venous Congestion (IVC, Portal Vein)
High Cardiac Output (LVOT-VTI)
Pulmonary Hypertension (TRVmax)
3/18



Portal Vein = > 100% pulsatility
LVOT VTI = 26
TRVmax = 3.04 m/s
So we have:
Venous Congestion (IVC, Portal Vein)
High Cardiac Output (LVOT-VTI)
Pulmonary Hypertension (TRVmax)
3/18




This was a case of High Output Heart failure secondary to Hereditary hemorrhagic telangiectasia
You can see many liver Arteriovenous malformations on CT scan!
4/18
You can see many liver Arteriovenous malformations on CT scan!
4/18
What is HOHF?
CO is usually normal or ⬇️ in patients with HF
A minority of pts present in a high-output state,
historically referred to as HOHF
The largest published cohort (PMID: 27470455) defined HOHF as:
elevated cardiac index (≥4 l/min/m2) + Clinical HF
5/18
CO is usually normal or ⬇️ in patients with HF
A minority of pts present in a high-output state,
historically referred to as HOHF
The largest published cohort (PMID: 27470455) defined HOHF as:
elevated cardiac index (≥4 l/min/m2) + Clinical HF
5/18

There are 5 main causes 👇
Regardless of cause, hemodynamics look pretty similar:
🔷Post-capilary PH (Wedge pressure > 15 mm Hg)
🔷⬆️RH and PA pressures
🔷 Preserved LV Ejection Fraction
*This cohort excluded anemia and hyperthyroidism as "reversible causes".
6/18


Regardless of cause, hemodynamics look pretty similar:
🔷Post-capilary PH (Wedge pressure > 15 mm Hg)
🔷⬆️RH and PA pressures
🔷 Preserved LV Ejection Fraction
*This cohort excluded anemia and hyperthyroidism as "reversible causes".
6/18



What leads to HOHF?
As this is a state of ⬆️ CO + Venous Congestion, increased plasma volume looks like a likely culprit
And yes, there is definitely increased Plasma Volume in HOHF.
But is ⬆️ plasma volume the cause of this condition?
7/18
As this is a state of ⬆️ CO + Venous Congestion, increased plasma volume looks like a likely culprit
And yes, there is definitely increased Plasma Volume in HOHF.
But is ⬆️ plasma volume the cause of this condition?
7/18

The answer is a strong: NO
⬆️ Plasma volume (whether caused by experimental saline loading or primary renal salt and water retention) does in fact initially lead to ⬆️CO
However this is NOT sustained!!!
8/18
⬆️ Plasma volume (whether caused by experimental saline loading or primary renal salt and water retention) does in fact initially lead to ⬆️CO
However this is NOT sustained!!!
8/18

Why is ⬆️CO not sustained?
⬆️CO will lead to tissue over-perfusion: Tissues do not like this!!
Tissues have the ability to regulate their flow by changing their resistance to flow
Regulation of flow has a higher priority than the regulation of pressure!
9/18
⬆️CO will lead to tissue over-perfusion: Tissues do not like this!!
Tissues have the ability to regulate their flow by changing their resistance to flow
Regulation of flow has a higher priority than the regulation of pressure!
9/18
⬆️ Tissue perfusion ➡️ Increased resistance (vasoconstriction) ➡️ Systemic Hypertension
Hypertension is a necessary evil because it leads to "pressure natriuresis". This helps the body get rid of most of the extra plasma volume!
10/18

Hypertension is a necessary evil because it leads to "pressure natriuresis". This helps the body get rid of most of the extra plasma volume!
10/18


This means the only way to have a sustained ⬆️ in CO is to have a sustained decrease in total peripheral resistance!
ALL patients with HOHF have ⬇️ systemic vascular resistance (SVR) which happens to be the most important hemodynamic determinant of survival
11/18

ALL patients with HOHF have ⬇️ systemic vascular resistance (SVR) which happens to be the most important hemodynamic determinant of survival
11/18


Sustained ⬇️ SVR can be caused by:
1⃣ Shunts
2⃣ Increased Metabolic Demands
12/18
1⃣ Shunts
2⃣ Increased Metabolic Demands
12/18
1⃣ Shunts:
AV fístula or AV malformation itself is the cause of ⬇️ SVR
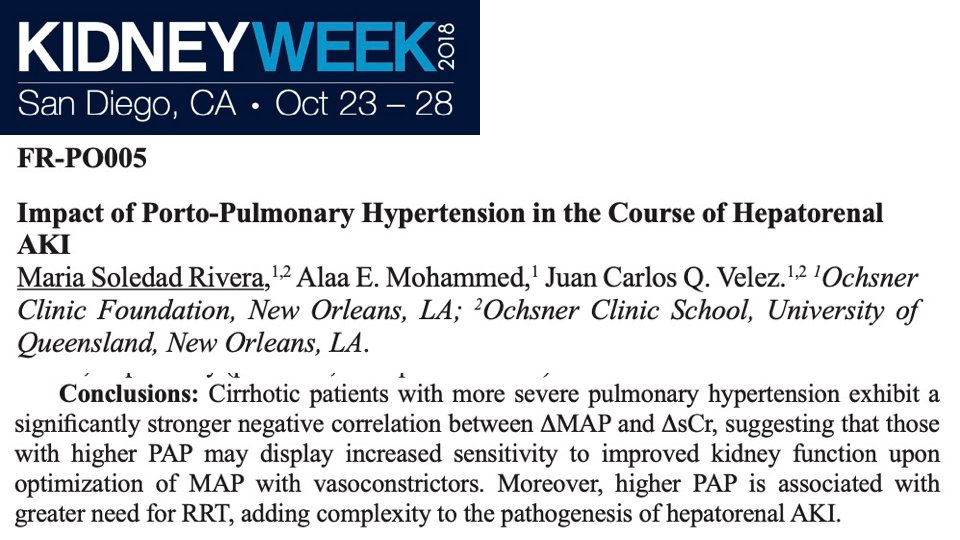
In Cirrhosis: Sustained splanchnic vasodilation is the cause. This is likely why AKI in these patients respond so well to Norepinefrine (work from @VelezNephHepato). They don't need more fluid!
13/18
AV fístula or AV malformation itself is the cause of ⬇️ SVR
In Cirrhosis: Sustained splanchnic vasodilation is the cause. This is likely why AKI in these patients respond so well to Norepinefrine (work from @VelezNephHepato). They don't need more fluid!
13/18
Here is a case of HOHF in Cirrhosis from my friend @Thind888:
Also a similar case of mine:
14/18
https://twitter.com/Thind888/status/1222682265953755137?s=20
Also a similar case of mine:
https://twitter.com/ArgaizR/status/1361563593347637249?s=20
14/18
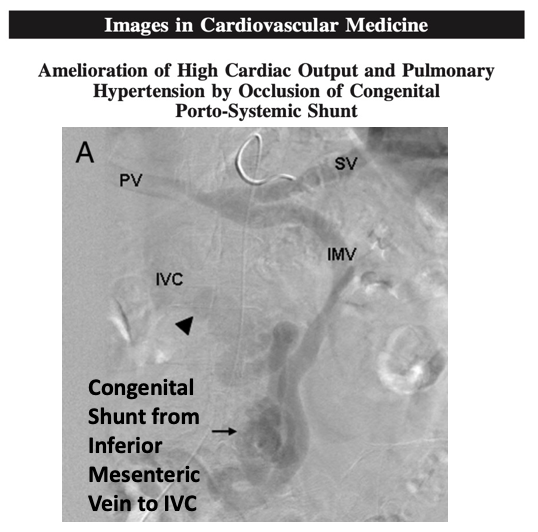
Besides splanchnic vasodilation, porto-systemic shunts (bypassing liver sinusoid resistance) can also contribute to HOHF
This is an awesome case of a congenital porto-systemic shunt WITHOUT cirrhosis leading to HOHF.
Shunt closure fixed this!
15/18

This is an awesome case of a congenital porto-systemic shunt WITHOUT cirrhosis leading to HOHF.
Shunt closure fixed this!
15/18

2⃣ Increased Metabolic Demands
⬆️ tissue metabolic demands will need ⬆️ blood flow for sustenance.
This will cause ⬇️ SVR and could end up causing HOHF!
This is the cause in Obesity.
This is also the cause of reversible pulmonary hypertension in Graves disease!
16/18
⬆️ tissue metabolic demands will need ⬆️ blood flow for sustenance.
This will cause ⬇️ SVR and could end up causing HOHF!
This is the cause in Obesity.
This is also the cause of reversible pulmonary hypertension in Graves disease!
16/18

Here is one of my favorite cases of HOHF from @AndreMansoor resulting from increase metabolic demands 2/2 thiamine deficiency. This was diagnosed at the beside by examining the nails!
17/18
https://twitter.com/AndreMansoor/status/1207348687841583105?s=20
17/18
In summary:
🔷HOHF is caused by sustained Low SVR
🔷 Low SVR is caused by 1) Shunt or 2) Increased metabolic demands
🔷 These pts have preserved EF. If one ignores CO, one might confuse this as garden variety HFpEF
🔷 Measuring CO is easy with #POCUS. Look at LVOT VTI!
18/18
🔷HOHF is caused by sustained Low SVR
🔷 Low SVR is caused by 1) Shunt or 2) Increased metabolic demands
🔷 These pts have preserved EF. If one ignores CO, one might confuse this as garden variety HFpEF
🔷 Measuring CO is easy with #POCUS. Look at LVOT VTI!
18/18
• • •
Missing some Tweet in this thread? You can try to
force a refresh