A tale of two hearts: Physiological observations on AV shunts and congestion 🧵
These are 2 patients on IHD I saw in the outpatient clinic
🔷 Both with severe venous congestion (#VExUS = 3)
🔷 Both with tortuous brachiocephalic AV fístula
1/11
These are 2 patients on IHD I saw in the outpatient clinic
🔷 Both with severe venous congestion (#VExUS = 3)
🔷 Both with tortuous brachiocephalic AV fístula
1/11

What I found remarkable was the diametrically opposed effects of manual AVF compression on JVP! 🤯
🔴 Patient A: AVF Compression improves venous congestion
🔵 Patient B: AVF Compression worsens venous congestion
2/11
🔴 Patient A: AVF Compression improves venous congestion
🔵 Patient B: AVF Compression worsens venous congestion
2/11
🔴 Patient A: SLE + Lupus Nefritis ➡️ ESRD in HD
#echofirst: Plethoric IVC, good LVEF, paradoxical septal motion, ventricular interdependence, severe RV/RA dilation, torrential TR
3/11
#echofirst: Plethoric IVC, good LVEF, paradoxical septal motion, ventricular interdependence, severe RV/RA dilation, torrential TR
3/11
🔴 Some Doppler for the nerds 🤓
LVOT VTI = 21.9
Cardiac Index = 4.38
TRVmax = Triangular shape (can't calculate RVSP with torrential TR)
This looks like severe PAH. The hx of SLE suggests group 1 PH
There is also high CI (>4) suggesting High Output Heart Failure (HOHF)!
4/11
LVOT VTI = 21.9
Cardiac Index = 4.38
TRVmax = Triangular shape (can't calculate RVSP with torrential TR)
This looks like severe PAH. The hx of SLE suggests group 1 PH
There is also high CI (>4) suggesting High Output Heart Failure (HOHF)!
4/11

🔵 Patient B: T2DM ➡️ ESRD in HD
#echofirst: Plethoric IVC, good LVEF, preserved LV/RV ratio, increased left filling pressures and mild TR (not shown, pleural effusion.
5/11
#echofirst: Plethoric IVC, good LVEF, preserved LV/RV ratio, increased left filling pressures and mild TR (not shown, pleural effusion.
5/11
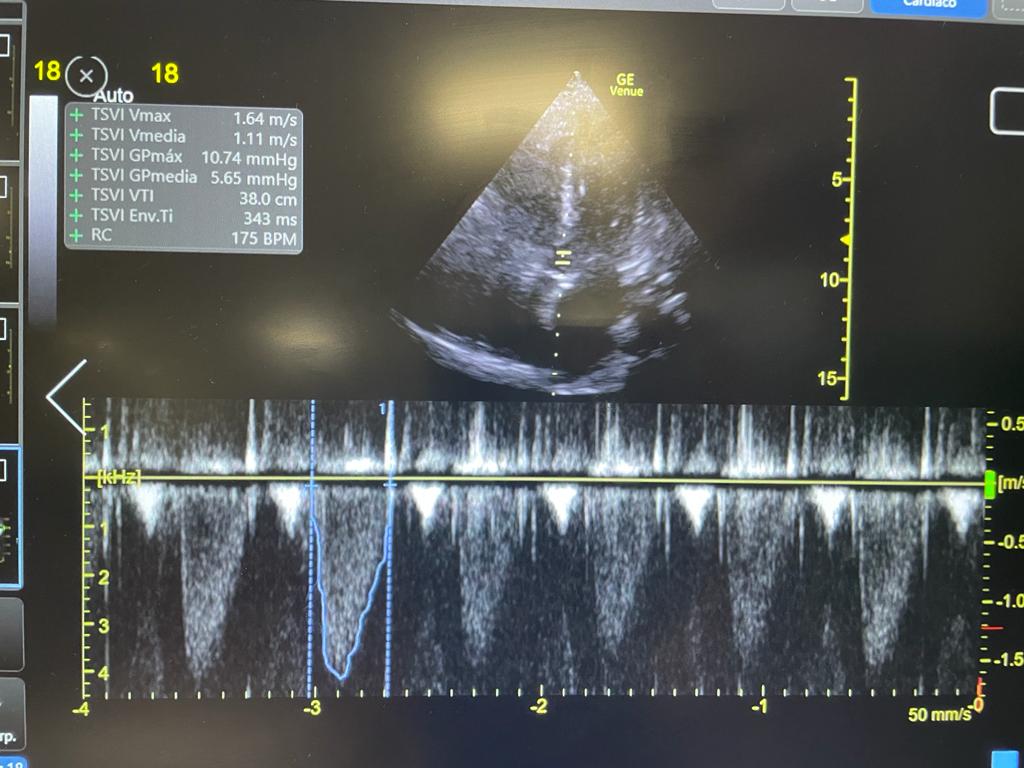
🔵 Some Doppler for the nerds 🤓
LVOT VTI = 29
Cardiac Index = 3.19 (normal)
TRVmax = 3.2
This looks like garden variety Heart Failure with Preserved Ejection Fraction (HFpEF)
6/11
LVOT VTI = 29
Cardiac Index = 3.19 (normal)
TRVmax = 3.2
This looks like garden variety Heart Failure with Preserved Ejection Fraction (HFpEF)
6/11

To understand the physiology it helps to remember that the creation of an AV Fístula causes significant hemodynamic changes:
🔷 Lower SVR
🔷 Lower Afterload
🔷 Increased venous return and Preload
🔷 Increased Cardiac Output
academic.oup.com/eurheartj/arti…
7/11
🔷 Lower SVR
🔷 Lower Afterload
🔷 Increased venous return and Preload
🔷 Increased Cardiac Output
academic.oup.com/eurheartj/arti…
7/11
Here is what I believe is happening!
🔑 AVF compression = ⬆️ Afterload and ⬇️ Preload
A🔴: PAH + torrential TR is more susceptible to ⬆️ Preload (Improves with AVF compression)
B🔵: HFpEP (Group 2 PH) is more susceptible to ⬆️ Afterload (Worsens with AVF compression)
8/11
🔑 AVF compression = ⬆️ Afterload and ⬇️ Preload
A🔴: PAH + torrential TR is more susceptible to ⬆️ Preload (Improves with AVF compression)
B🔵: HFpEP (Group 2 PH) is more susceptible to ⬆️ Afterload (Worsens with AVF compression)
8/11
A bit is more to this story:
Let's take a look at the AVFs!
A🔴: Flow = 1607 ml/min
B🔵: Flow = 1020 ml/min
Also, manual compression of the AVF improves #VExUS in A🔴 but does nothing for B🔵!
9/11



Let's take a look at the AVFs!
A🔴: Flow = 1607 ml/min
B🔵: Flow = 1020 ml/min
Also, manual compression of the AVF improves #VExUS in A🔴 but does nothing for B🔵!
9/11




A🔴: High flow fistula (>1500 ml/min) + improving with compression suggests AV fistula is strongly contributing to RHF and HOHF
B🔵: Pt was actually 6 kg above "dry weight"
We decided to remove the AVF for A🔴 and intensify UF for B🔵
This achieved decongestion on both!
10/11

B🔵: Pt was actually 6 kg above "dry weight"
We decided to remove the AVF for A🔴 and intensify UF for B🔵
This achieved decongestion on both!
10/11


Patient A🔴 had PAH that was severely exacerbated by AVF induced HOHF!
Patient B🔵 had HFpEF, congestion was caused by volume overload!
#VExUS takes hemodynamic evaluation to another level!
We reported the findings on Patient A🔴 in this letter: academic.oup.com/ckj/advance-ar…
END/
Patient B🔵 had HFpEF, congestion was caused by volume overload!
#VExUS takes hemodynamic evaluation to another level!
We reported the findings on Patient A🔴 in this letter: academic.oup.com/ckj/advance-ar…
END/
BONUS:
Here is #echofirst from Pt A🔴 before and 24 hrs after fistula ligation:
There was immediate reversal of septal flattening!
1/2
Here is #echofirst from Pt A🔴 before and 24 hrs after fistula ligation:
There was immediate reversal of septal flattening!
1/2
Also there was reversal of Torrential TR, only moderate TR remained.
Formal echocardiogram after 3 weeks showed complete reversal of pulmonary hypertension and only mild TR
END OF BONUS
Formal echocardiogram after 3 weeks showed complete reversal of pulmonary hypertension and only mild TR
END OF BONUS
• • •
Missing some Tweet in this thread? You can try to
force a refresh