With #Omicron rapidly spreading nationwide, I am concerned about all the members of our communities with damage and injury in the immune system, particularly to cell-mediated injury (to T cells and Ab-producing cells). In neutralization studies, most monoclonal Abs used to date
2/ have lost activity to #Omicron and are no longer useful in areas with high attack rates (pretty much everywhere in US right now). There are two possible exceptions. The first is #sotrovimab which was originally isolated from an individual with
3/ #SARSCoV1 (not a typo) back in 2003. The Ab recognizes a conserved glycan motif at the base of the Spike protein (away from the ACE-2 receptor-binding domain). Extremely limited supplies and fairly narrow emergency use authorization, as follows:
4/ Limitations of Authorized Use.
• Sotrovimab is not authorized for use in patients:
o who are hospitalized due to COVID-19, OR
o who require oxygen therapy due to COVID-19, OR
o who require an increase in baseline oxygen flow rate due to COVID-19 (in those on chronic oxygen
• Sotrovimab is not authorized for use in patients:
o who are hospitalized due to COVID-19, OR
o who require oxygen therapy due to COVID-19, OR
o who require an increase in baseline oxygen flow rate due to COVID-19 (in those on chronic oxygen
5/ therapy due to underlying non-COVID-19 related comorbidity).
• Benefit of treatment with sotrovimab has not been observed in patients hospitalized due to COVID-19. (Copied from the EUA)
• Benefit of treatment with sotrovimab has not been observed in patients hospitalized due to COVID-19. (Copied from the EUA)
6/ The second mAb which may retain activity against #OmicronVariant is Tixagevimab/cilgavimab (Evusheld). The EUA stipulates use only for prophylaxis, but NOT for post-exposure prophylaxis, as follows, in the follwoing patients > 12 yo:
7/ • Who are NOT currently infected with SARS-CoV-2 and who have not had a known recent exposure to an individual infected with SARS-CoV-2 and
• Who have moderate to severe immune compromise due to a medical condition or receipt of immunosuppressive medications or treatments
• Who have moderate to severe immune compromise due to a medical condition or receipt of immunosuppressive medications or treatments
8/ and may not mount an adequate immune response
to COVID-19 vaccination or
• For whom vaccination with any available COVID-19 vaccine, according to the approved or authorized schedule, is not recommended due to a history of severe adverse reaction
to COVID-19 vaccination or
• For whom vaccination with any available COVID-19 vaccine, according to the approved or authorized schedule, is not recommended due to a history of severe adverse reaction
9/ There is a clear gap between these different EUAs. There is no coverage for post-exposure prophylaxis with either agent. In addition, neither agent is indicated for patients in hospital with #COVID19. The situation may change rapidly. In the meantime, dexamethasone and
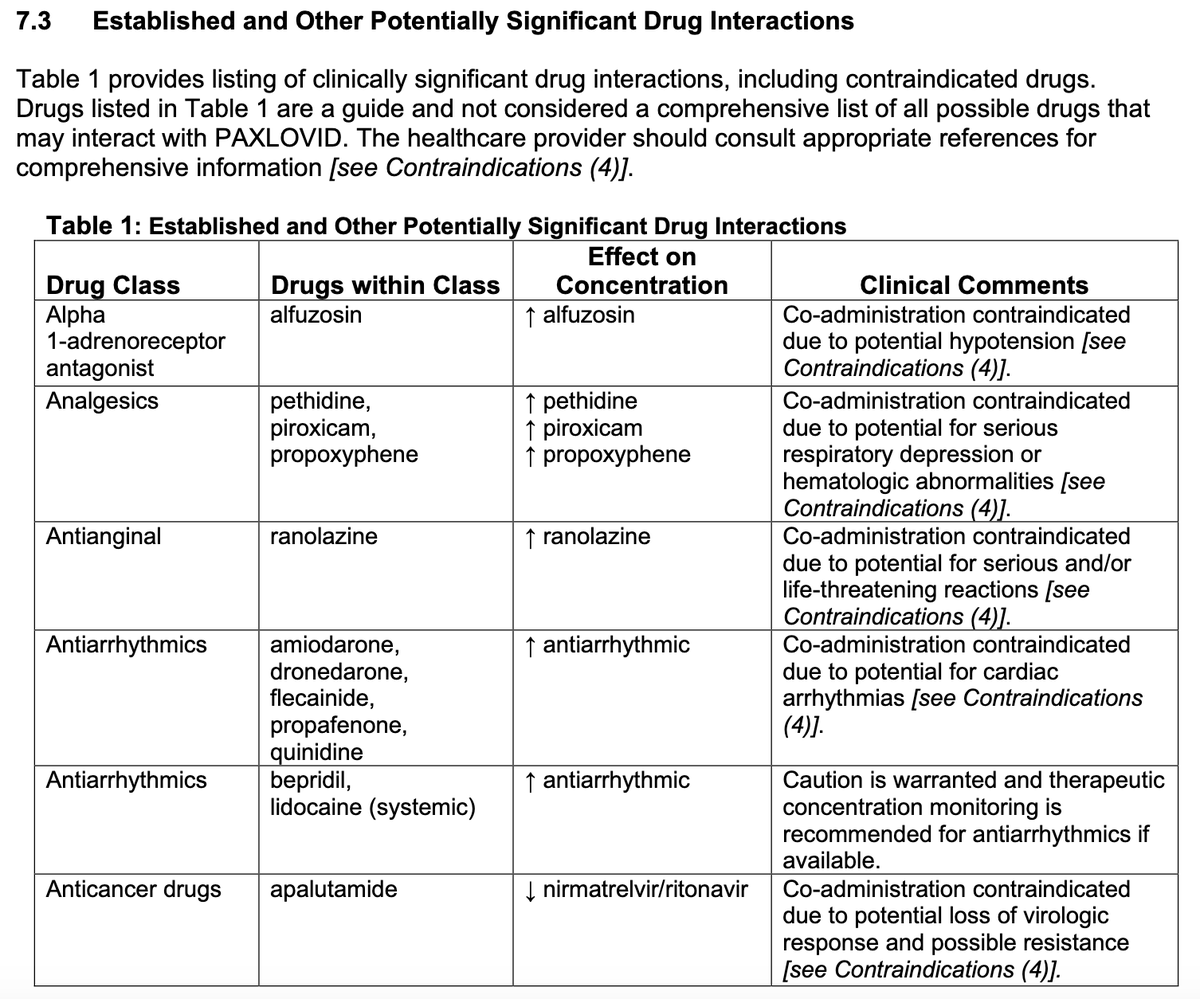
10/ remdesivir remain treatment options. In addition, we are eagerly awaiting news on paxlovid (which is Spike protein/variant agnostic based on mechanism on action). The goal is to limit morbidity among vulnerable patients @sloan_kettering and around the world. You can do your
11/ part by getting vaccinated, boosted, wearing a mask, and sending kind words to your exhausted health care provider doing their best to everyone safe, well, and alive. #GetVaccinatedNow #GetBoostedNow #Sotrovimab #monoclonalAb #COVID19
12/ Re: #Evusheld - it would be highly informative to see the primary data from @AstraZeneca that supports the statement on the retention of activity against #OmicronVariant - astrazeneca.com/media-centre/p…
@LionakisLab astutely points to the following data:
@LionakisLab astutely points to the following data:

13/ Source: biorxiv.org/content/10.110…
The question is how this observation translates to a real-world prophylaxis setting - given the increase in IC50, will the duration of protection (6 months) be negatively impacted? Important questions as prepare to administer to vulnerable
The question is how this observation translates to a real-world prophylaxis setting - given the increase in IC50, will the duration of protection (6 months) be negatively impacted? Important questions as prepare to administer to vulnerable
14/ groups @sloan_kettering and elsewhere. Great to have in arsenal but needs further study. #TxID #IDTwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh