
Just learn few fascinating things regarding the evolution of #SARSCoV2, pathogenicity of common cold coronaviruses (CCC), and the development of a new live attenuated vaccine candidate 1/
Those who think that the #Spike protein of #SARSCoV2 has ‘exhausted’ all its options to surprise us owing to limited space to undertake infinite mutations need to rethink & revise their opinions. 2/
A comparatively old paper on human coronavirus CoV-229E hints that 25 of the 31 receptor-contacting RBD residues in HCoV-229E have varied during virus's evolution in humans over the past 50 yrs. @jbloom_lab 3/
elifesciences.org/articles/51230
elifesciences.org/articles/51230

So, the #SARSCoV2 RBD is ‘not’ going to run out of evolutionary space. The spike’s landscape is truly vast. Mutational space seems far more capacious than previously thought. 4/
elifesciences.org/articles/51230
elifesciences.org/articles/51230
Another study suggests the same: The Spike S1 is the focus of adaptive evolution. But this is not alone. There are also positively selected mutations in other genes that are carving the evolutionary trajectory of SARS2. 5/
biorxiv.org/content/10.110…
biorxiv.org/content/10.110…
Adaptive changes in Spike's S1 accumulated rapidly, resulting in a remarkably high ratio of nonsynonymous to synonymous divergence that is 2.5X greater than that observed in HA1 of flu virus at the beginning of the 2009 H1N1 pandemic. @trvrb 6/
@trvrb Variants with high numbers of changes to the protein sequence in Spike spread faster than those without. Immune escape and increased receptor binding are being selected for. The SARS2 virus evolving many times faster than expected. 7/
But why should we be surprized, now?
We know from the beginning of the pandemic that enough sarbecoviruses sequences were available& the antigenic space is vast 8/
We know from the beginning of the pandemic that enough sarbecoviruses sequences were available& the antigenic space is vast 8/
Now come to the other issue: Why SARS2 is far more virulent than HCCoVs? As per @georgimarinov's idea, the greater number of accessory proteins in SARS-CoV-2 compared to seasonal HCoVs might partly explain its greater virulence. 9/ 

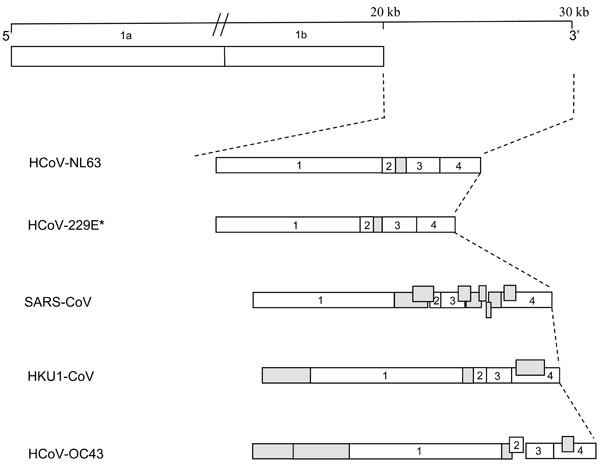

@georgimarinov These accessory proteins are largely responsible for the enhanced virulence. High levels of innate/cellular immune evasion and modulation are a great benefit to the virus. 10/
When you look at the HCCCoV genomes & the MERS/SARS ones, the immediately obvious difference is how many accessory proteins the latter have, while the HCCCs mostly have just one. And all of those are involved in fighting innate and adaptive immunity. 11/
https://twitter.com/georgimarinov/status/1495086316341522435?s=21
A new live attenuated Covid19 vaccine candidate is being developed based on the above knowledge where the researchers deleted ORF 3, 6, 7, and 8 (Δ3678). 12/
biorxiv.org/content/10.110…
biorxiv.org/content/10.110…
Among the deleted ORFs in the Δ3678 virus, #ORF3a accounts for the most attenuation through antagonizing STAT1 phosphorylation during type-I interferon signaling. 13/
The Δ3678 virus replicates about 7,500-fold lower than wild-type SARS-CoV-2 on primary human airway cultures but restores its replication on IFN-deficient Vero-E6 cells that are approved for vaccine production. 14/
biorxiv.org/content/10.110…
biorxiv.org/content/10.110…
Coming back to the HCCCoV 229E & other HCoVs. Why did they not evolve to greater virulence? Are these seasonal HCCoVs ‘benign’ right from the beginning? Is there any good record of how the virulence of 229E (or the other 4 HCoVs) has varied over the years? 15/
As per @jbloom_lab, CoV-229E mild as long as we've known about it. It was isolated in 1966 & next year they infected 26 volunteers: half developed colds. 229E probably jumped to humans way before 1966. 16/
https://twitter.com/jbloom_lab/status/1495045679151935495?s=20&t=22WF0KTCo1-WwbPro22ZQA
Speculation is that another HCoV OC43 maight have caused pandemic in 1889 but evidence is ‘very’ thin 17/
Nobody has any evidence at all that HCCCoVs, or many other pathogens, ever 'attenuated' -- it's just presumed on the basis of a hasty generalization from some very specific cases of obligate parasites. 18/
Also, it might be true that a SARS2 pandemic didn't get really noticed when life expectancy was <30 with the extreme age skew of mortality. Even when they had no supplemental oxygen, anti-coaugulants, immunosuppresants, etc. 19/
https://twitter.com/georgimarinov/status/1495086316341522435?s=20&t=22WF0KTCo1-WwbPro22ZQA
But a #SARS1 pandemic would be noticed even pre-20th century. The claim is that HCCCs were bad but attenuated. But there's no reason to assume they were exactly SARS2-level bad. Why not a lot worse? Or a lot milder? @Georgimarinov 20/
Still, there are many missing links in our knowledge. Probably, it’s because we didn’t have the *tools* to properly study viruses’ evolutions at the time when major churning was taking place. Many of our current assumptions may be wrong 21/
• • •
Missing some Tweet in this thread? You can try to
force a refresh















