1) Welcome to our new #accredited #tweetorial on #mechanismofaction & impact of meds commonly used in patients with or at risk for #DKD progression: #MRAs, #GLP-1 receptor agonists & #DPP-4 inhibitors. I am Sophia Ambruso DO, @sophia_kidney, from @CU_Kidney. 

2) This #accredited #tweetorial series on #kidneydisease #DKD through the lens of #T2D is supported by an independent educational grant from the Boehringer Ingelheim/Lilly Alliance and is intended for healthcare providers.
3) This activity is accredited for #physicians #physicianassociates #nurses #NPs #pharmacists. Past programs still eligible for credit can be found at ckd-ce.com. Faculty disclosures are at ckd-ce.com/disclosures/. FOLLOW US for regular programs by expert faculty!
4) Let’s start with a case. 65 YO with #T2D & #HTN is referred for mgt of #DKD. Meds include metformin, lisinopril & empagliflozin. BP 125/78. Pertinent labs: Na 140, K 4.5, BUN 30, Crea 1.9, A1c 7.5, #UACR 750mg/g. What’s your next step in management?
5) We must view this case and SO many more like it in the context of #DM as a global health crisis, affecting
~27-31 million ppl (8.2% of US population)
~400 million ppl worldwide
🔓cdc.gov/diabetes/pdfs/…
~27-31 million ppl (8.2% of US population)
~400 million ppl worldwide
🔓cdc.gov/diabetes/pdfs/…
6) #DM affects ~10% of the US population
As of 2018, crude prevalence of #ESKD attributable to diabetes was 38.6%.
Diabetes is the leading cause of #CKD worldwide, accounting for up to 5⃣0⃣% of all patients with ESKD.
As of 2018, crude prevalence of #ESKD attributable to diabetes was 38.6%.
Diabetes is the leading cause of #CKD worldwide, accounting for up to 5⃣0⃣% of all patients with ESKD.
7) There were an estimated 219,451 deaths attributed to diabetic kidney disease #DKD, ➡️approximately 35% of ALL CKD deaths in 2017 worldwide.
See below: diabetic kidney disease mortality per 100,000 worldwide in 2017
🔓link.springer.com/article/10.100…
See below: diabetic kidney disease mortality per 100,000 worldwide in 2017
🔓link.springer.com/article/10.100…
8) The combination #DM+#CKD ➡️independent & additive effect on #CV risk & mortality.
For every halving of #eGFR, CV incidence is 2x higher.
For every 10x ⬆️in baseline urine albumin, CV event incidence is 2.5x higher.
🔓pubmed.ncbi.nlm.nih.gov/22051245/
🔓ncbi.nlm.nih.gov/pmc/articles/P…

For every halving of #eGFR, CV incidence is 2x higher.
For every 10x ⬆️in baseline urine albumin, CV event incidence is 2.5x higher.
🔓pubmed.ncbi.nlm.nih.gov/22051245/
🔓ncbi.nlm.nih.gov/pmc/articles/P…

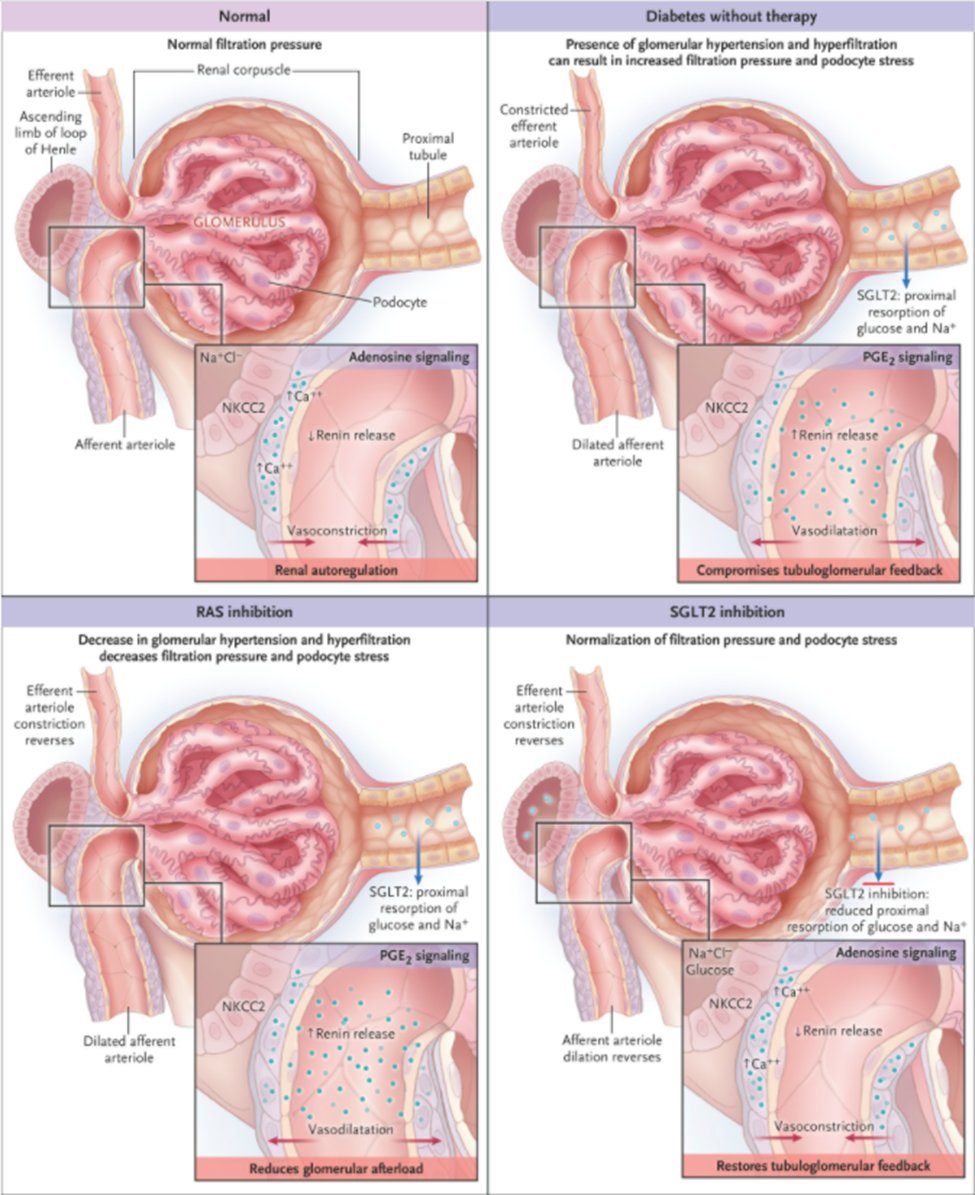
9) Progression of diabetic nephropathy #DN, begins with glomerular #hyperfiltration followed by
moderate albuminuria ➡️ severe albuminuria ➡️ progressive #CKD ➡️#ESKD
🔓pubmed.ncbi.nlm.nih.gov/29398179/

moderate albuminuria ➡️ severe albuminuria ➡️ progressive #CKD ➡️#ESKD
🔓pubmed.ncbi.nlm.nih.gov/29398179/


10) Hyperfiltration is ≥25% ⬆️ in GFR secondary to
- afferent arteriolar vasodilation
- efferent arteriolar vasoconstriction
thereby ⬆️intraglomerular pressures
🔓jasn.asnjournals.org/content/early/…
nejm.org/doi/full/10.10…

- afferent arteriolar vasodilation
- efferent arteriolar vasoconstriction
thereby ⬆️intraglomerular pressures
🔓jasn.asnjournals.org/content/early/…
nejm.org/doi/full/10.10…


11) Hyperfiltration is mediated by
- impaired tubuloglomerular feedback #TGF
- local and circulating vascular factors &
- upregulated #RAAS activity.
🔓jasn.asnjournals.org/content/early/…
- impaired tubuloglomerular feedback #TGF
- local and circulating vascular factors &
- upregulated #RAAS activity.
🔓jasn.asnjournals.org/content/early/…
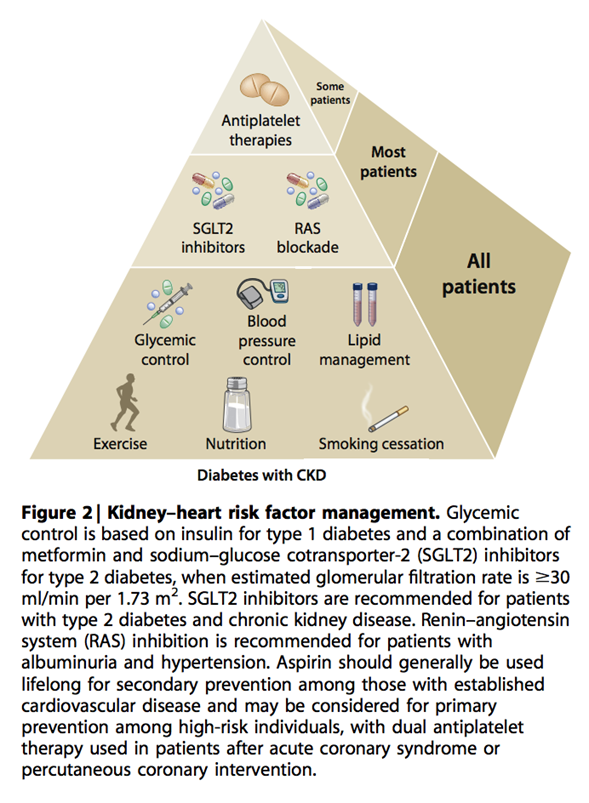
12) Goal of #DKD treatment is three-fold:
I. reduce concurrent or continued injury by addressing modifiable risk factors
--Glycemic control (goal A1c <7)
--Weight loss
--Smoking cessation
--BP control (goal <130/80)
--Low salt diet
🔓ajkd.org/article/S0272-…
I. reduce concurrent or continued injury by addressing modifiable risk factors
--Glycemic control (goal A1c <7)
--Weight loss
--Smoking cessation
--BP control (goal <130/80)
--Low salt diet
🔓ajkd.org/article/S0272-…
13) Goal of #DKD treatment is three-fold:
II. medicines that improve glomerular hemodynamics and intraglomerular pressures thereby modifying hyperfiltration
III. medicines with anti-inflammatory/antifibrotic activity
🔓ajkd.org/article/S0272-…
II. medicines that improve glomerular hemodynamics and intraglomerular pressures thereby modifying hyperfiltration
III. medicines with anti-inflammatory/antifibrotic activity
🔓ajkd.org/article/S0272-…
14) The most familiar medicines known to alter glomerular hemodynamics are the #RAASi agents (#ACEi & #ARBs) and #SGLT2i.
nejm.org/doi/full/10.10…
In fact, the discovery of new mechanisms of #SGLT2i kidney and CV anti-inflammatory and antifibrotic effects continues ….
nejm.org/doi/full/10.10…
In fact, the discovery of new mechanisms of #SGLT2i kidney and CV anti-inflammatory and antifibrotic effects continues ….
15) In this #FOAMed #tweetorial, we will focus on the activity of & kidney benefits of glucagon-like peptide 1 #GLP-1 receptor agonists, glucose-dependent insulinotropic peptide-4 inhibitors #DPP-4i receptor inhibitors, & nonsteroidal mineralocorticoid receptor antagonist #MRAs
16) So let’s start with glucagon-like peptide 1 (#GLP-1) agonists. What are the renal protective benefits of GLP-1 agonists?
a. anti-inflammatory
b. glycemic control
c. natriuresis upregulated TGF
d. all of the above
a. anti-inflammatory
b. glycemic control
c. natriuresis upregulated TGF
d. all of the above
17) Mark your best answer & return TOMORROW for more education &🆓CE/#CME credit as we explore the impact of these 3⃣ classes of medications used in the fight against #DKD! Shout-outs @edgarvlermamd @nephondemand @ChristosArgyrop @dguerrot @kdjhaveri @AtulPathak31 @lissabauer
18) Welcome back! We are talking #mechanismofaction & impact of meds commonly used in pts with or at risk for #DKD progression: #MRAs, #GLP-1 receptor agonists & #DPP-4 inhibitors. I am @sophia_kidney & you are earning CE/#CME. Hello to
@inglisjosh @AliceYYCheng @RpratleyMD
@inglisjosh @AliceYYCheng @RpratleyMD
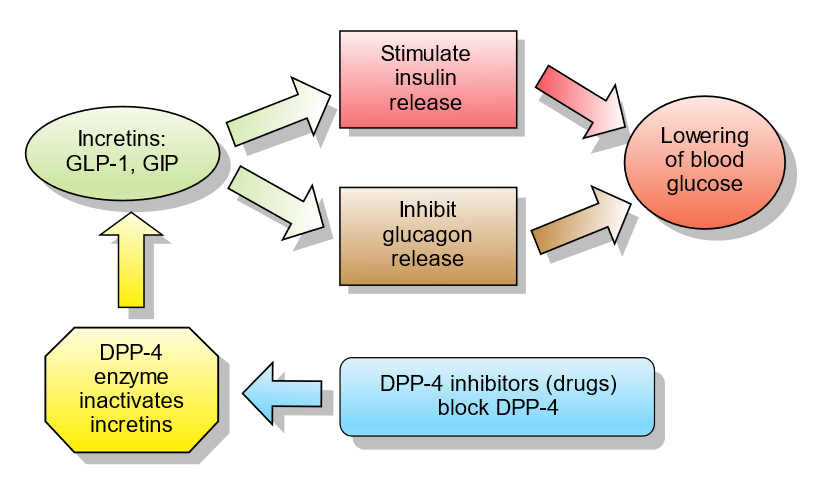
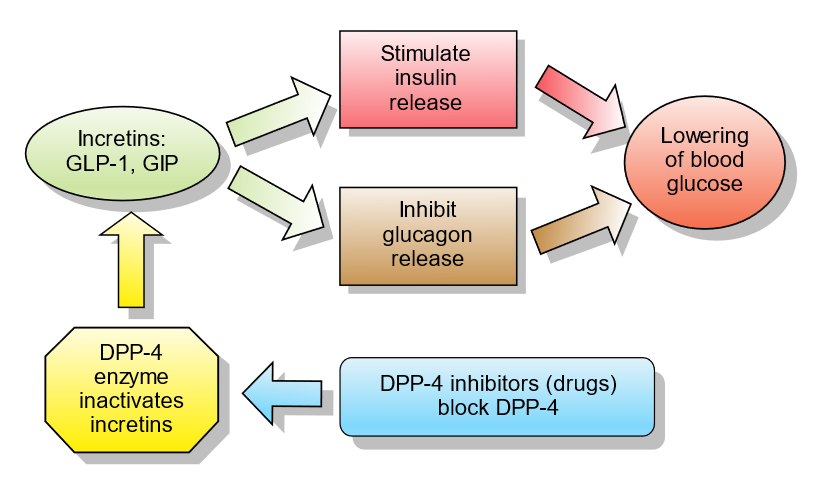
19) The answer to yesterday's poll? ALL of the above. #GLP-1 is an #incretin hormone, a gut hormone released postprandial with a goal of decreasing blood glucose via augmented insulin release and inhibited glucagon release. Figure from
🔓en.wikipedia.org/wiki/Incretin
🔓en.wikipedia.org/wiki/Incretin
20) In pts with #DM, the benefits of #GLP-1 agonists are striking:
--↑insulin, ↓glucagon
--↓insulin resistance
--↓appetite, ↑satiety
--Weight loss
--Improved endothelial function
--Improved myocardial contractility
--↓ inflammation
--Natriuresis
nature.com/articles/nrnep…
--↑insulin, ↓glucagon
--↓insulin resistance
--↓appetite, ↑satiety
--Weight loss
--Improved endothelial function
--Improved myocardial contractility
--↓ inflammation
--Natriuresis
nature.com/articles/nrnep…
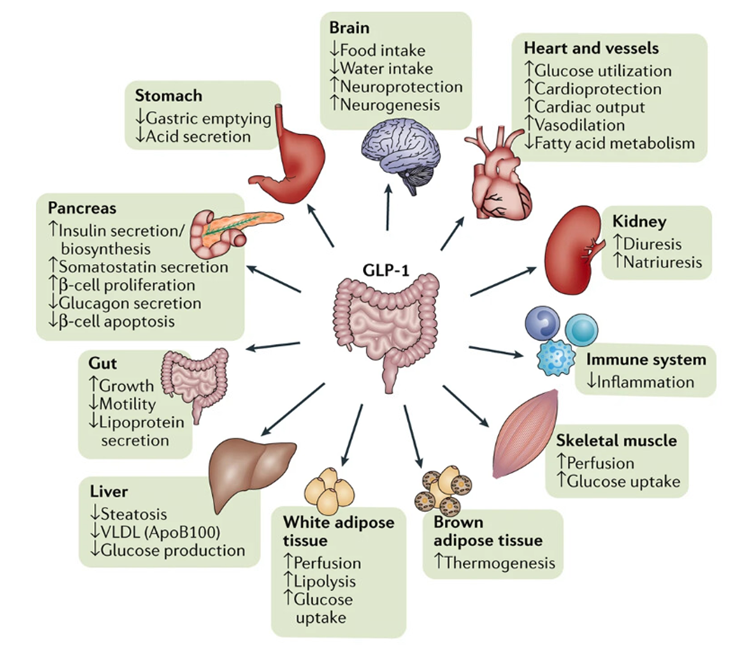
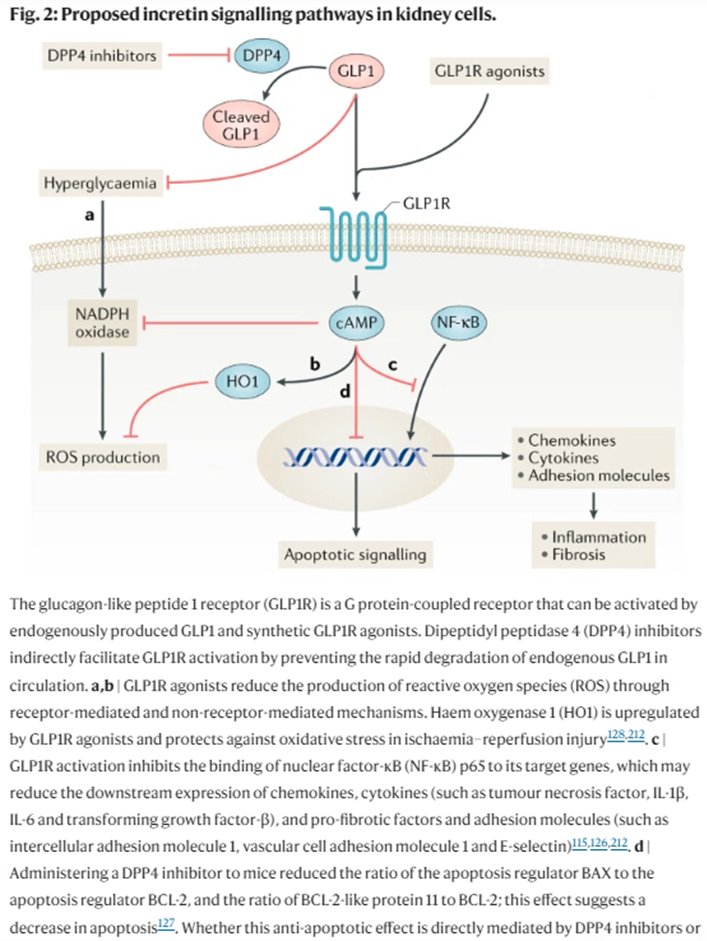
21) Below is a summary of preclinical data supporting anti-inflammatory actions of incretin therapies
nature.com/articles/s4158…

nature.com/articles/s4158…


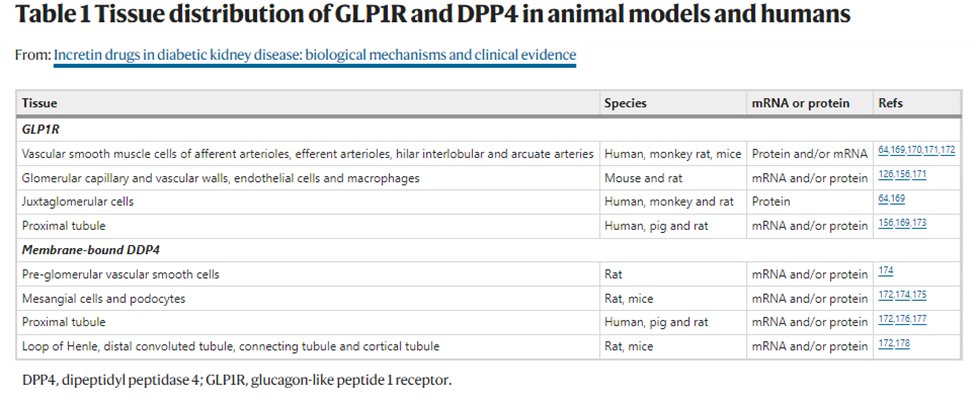
22) #GLP-1 receptors are found in smooth muscle cells of renal arterioles (efferent and afferent) & arteries, glomerular capillary & vascular walls, juxtaglomerular cells, & proximal tubule suggesting its anti-inflammatory reach
nature.com/articles/s4158…
nature.com/articles/s4158…
23) #GLP-1 agonists⬆️#GFR through⬆️renal blood flow, mediated by an attenuated autoregulatory response resulting in afferent arteriole vasodilatation.
doi.org/10.1152/ajpren…
doi.org/10.1152/ajpren…
24) In a study in🐀, GLP-1 agonists suppressed renal proximal tubular reabsorption by 20-40% & increased urine flow rate six-fold without altering TGF responsiveness, suggesting proximal diuretic & renal vasodilator activity
🔓journals.physiology.org/doi/full/10.11…
🔓journals.physiology.org/doi/full/10.11…
25) Interestingly, in subjects with diabetic kidney disease and hyperfiltration, the increased GFR and RBF of those on GLP-1 agonists is not observed. Why?
26) It is proposed in #DKD and #hyperfiltration, afferent arteriolar vasodilatory GLP1 agonist response is attenuated.
27) The indirect effects associated with GLP-1 induced-natriuresis is the predominant physiology returning glomerular hemodynamics closer to normal, where distal sodium delivery increases #TGF & suppresses #RAAS
28) How do #GLP-1 agonists induce a natriuresis?
a. Inhibit the sodium chloride cotransporter (NCC) in DCT
b. partial inhibition of the SGLT2 cotransporter in PCT
c. inhibition of the NHE3 in the PCT
d. all of the above
Mark your answer before scrolling⤵️‼️
a. Inhibit the sodium chloride cotransporter (NCC) in DCT
b. partial inhibition of the SGLT2 cotransporter in PCT
c. inhibition of the NHE3 in the PCT
d. all of the above
Mark your answer before scrolling⤵️‼️
29) Did you mark C?
In fact, #GLP-1 agonists reduce phosphorylation of renal cortical Na+/H+ exchanger isotope 3 (NHE3) antiporter, which correlates with NHE3 reduced transport activity in the proximal tubule and resultant natriuresis.
🔓journals.physiology.org/doi/full/10.11…
In fact, #GLP-1 agonists reduce phosphorylation of renal cortical Na+/H+ exchanger isotope 3 (NHE3) antiporter, which correlates with NHE3 reduced transport activity in the proximal tubule and resultant natriuresis.
🔓journals.physiology.org/doi/full/10.11…
30) Combined, the proposed resulting renoprotective effects are complex & include
--TGF upregulation & glomerular hemodynamic normalization
--⬇️Reactive oxygen species #ROS production
--⬇️ chemokine & cytokine release
--⬇️ inflammation & fibrosis
🔓ncbi.nlm.nih.gov/pmc/articles/P…
--TGF upregulation & glomerular hemodynamic normalization
--⬇️Reactive oxygen species #ROS production
--⬇️ chemokine & cytokine release
--⬇️ inflammation & fibrosis
🔓ncbi.nlm.nih.gov/pmc/articles/P…
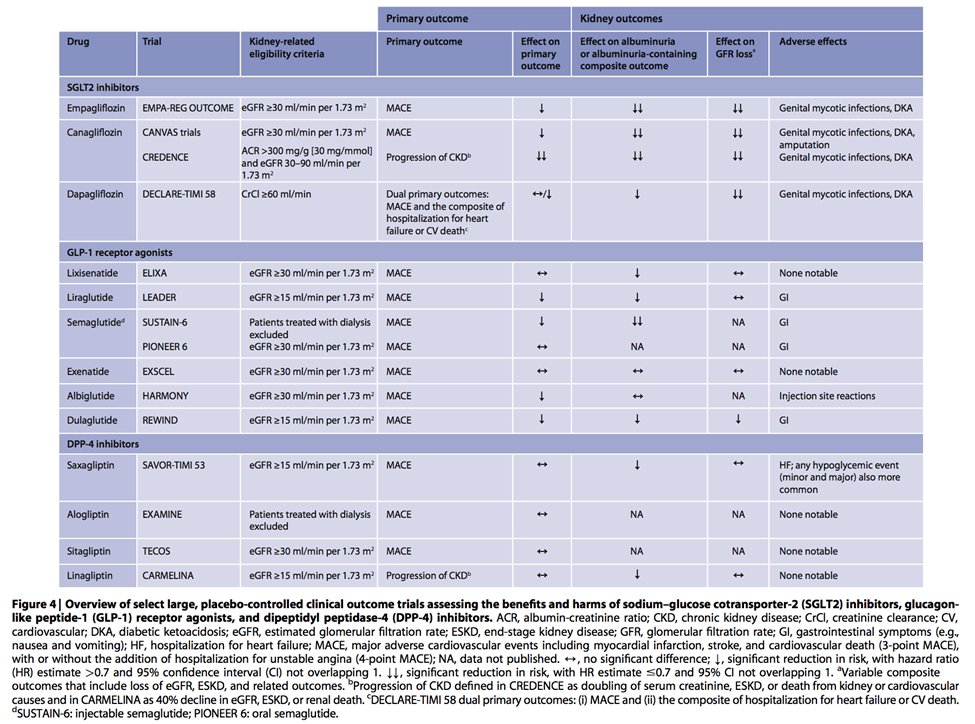
31) Cardiovascular #CV outcome studies summarized below revealed mixed kidney outcome results but strongly trend towards renoprotective activity through reduction in albuminuria and/OR better secondary composite kidney outcomes
nature.com/articles/s4158…
nature.com/articles/s4158…
32) There are *more recent data* from the #AMPLITUDE-O #RCT of CV & renal outcomes with #efpeglenatide vs placebo in T2D. ✔️out the secondary composite outcome: UACR >300, UACR ≥30% increase from baseline, ESRD or death from any cause
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…
33) AMPLITUDE-O results: That secondary composite renal outcome favored efpeglenatide; 353 events occurred in efpeglenatide vs 250 in patients on placebo
HR 0.6 (95% CI 0.57-0.79, p <0.001)
nejm.org/doi/full/10.10…
HR 0.6 (95% CI 0.57-0.79, p <0.001)
nejm.org/doi/full/10.10…
34) And we can still 👀 forward to the FLOW trial clinicaltrials.gov/ct2/show/NCT03…. This is the largest #RCT to date of weekly SQ semaglutide vs placebo. The primary composite outcome consists of 50% #eGFR ⬇️, kidney failure, or ☠️🪦 from kidney or #CV disease
35) So, TOMORROW, we'll address glucose-dependent insulinotropic peptide-4 (#DPP-4) inhibitors and #MRAs, and link you to your 0.75hr CE/#CME for #physicians #physicianassociates #nurses #pharmacists 🇺🇸🇬🇧🇪🇺🇨🇦. Don't miss it! FOLLOW US! #nephtwitter @MedTweetorials
36) Welcome back! I am @sophia_kidney and we're talkin bout 3⃣ classes of meds used to manage #DKD. You're earning CE/#CME the easy way, on Twitter! Hello to @KatherineTuttl8 @JoshuaNeumiller @arvindcanchi @PokrajacAna @DanielJDrucker @Chillslincoln79 @PhWafaShamlan
37) Onward to glucose-dependent insulinotropic peptide-4 (#DPP-4) inhibitors! MOA: inhibits DPP-4 enzyme that degrades incretins like GLP-1, preventing the postprandial fall of GLP-1. Otherwise, in vivo 1/2-life for the active GLP-1 peptide ~1-2min. From
ren.wikipedia.org/wiki/Incretin
ren.wikipedia.org/wiki/Incretin
38) By this mechanism, similar potential renoprotective mechanisms are proposed for DPP-4 inhibitors, albeit modest in comparison:
--Anti-inflammatory, antifibrotic activity
--Natriuresis
--Increased TGF activity
nature.com/articles/s4158…

--Anti-inflammatory, antifibrotic activity
--Natriuresis
--Increased TGF activity
nature.com/articles/s4158…

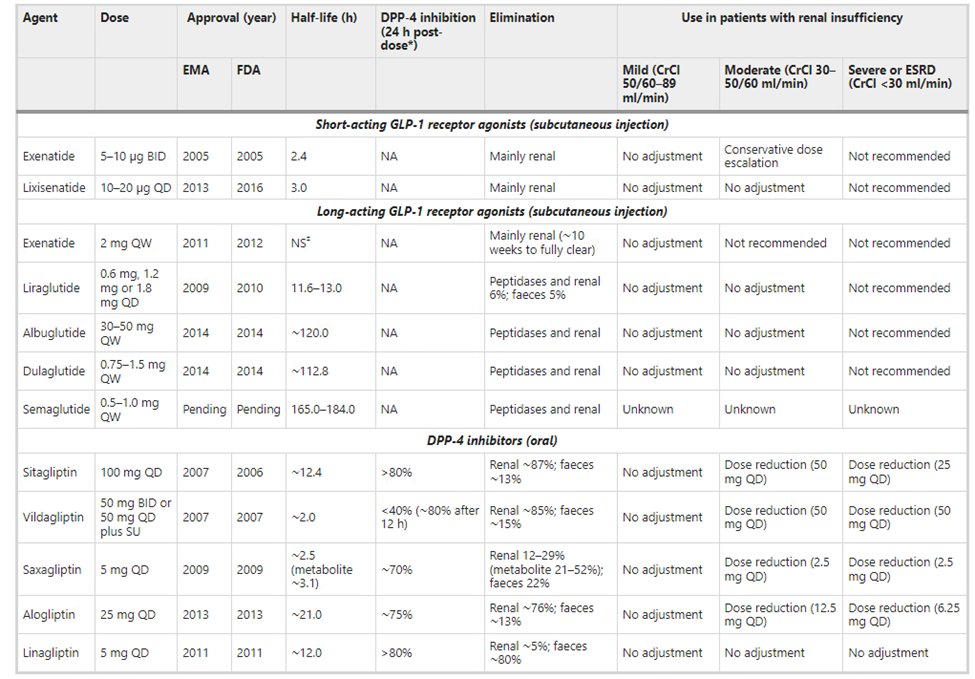
39) #DPP-4i clinical data have not revealed the same promising outcome data as have #GLP-1 agonists. As summarized below, no significant differences were seen in secondary, exploratory outcomes & secondary analyses. 

40) Then why are DPP-4 inhibitors seemingly less effective? First, ⬇️potency➡️DPP-4i's induce 1.5-3.0 fold ⬆️in circulating GLP-1, which is low compared to the 10x increase seen with therapeutic doses of GLP-1 agonists
41) Secondly, DDP-4i exert incretin-independent effects like bioactive peptide cleavage, which includes chemokines, neuropeptides & regulatory peptides, as well as impaired natural killer cell recruitment. These less-understood pleiotropic effects may muddy DPP-4i benefit.
42) Below is a list of incretin-based therapies, including #GLP-1 agonists and #DPP-4 inhibitors, from
nature.com/articles/nrnep…
nature.com/articles/nrnep…
43) The 2020 @goKDIGO Diabetes Management in #CKD Guideline provides a nice summary of clinical trials and evidence of albuminuria reduction vs GFR loss for #SGLT2i, #GLP-1 agonists and #DPP4i.
See 🔓kdigo.org/guidelines/dia…
See 🔓kdigo.org/guidelines/dia…
44) Based on this information, the antihyperglycemic #T2D + #CKD algorithm (along with #RAASi, #bloodpressure mgmt & lifestyle modification) includes #metformin & #SGLT2i, and then a #GLP-1 agonist is the next preferred agent.
See 🔓kdigo.org/guidelines/dia…

See 🔓kdigo.org/guidelines/dia…

45) So scroll back⤴️ to Tweet 4. What's your best next step for a pt w/#T2D+#HTN already on metformin, lisinopril & empagliflozin? BP 125/78. Pertinent labs: Na 140, K 4.5, BUN 30, Crea 1.9, A1c 7.5 and urine albumin to creatinine ratio of 750mg/g.
You'd start Semaglutide weekly
You'd start Semaglutide weekly
46) So finally, let’s shift to mineralocorticoid receptor antagonist (#MRA) agents, both steroidal & nonsteroidal formulations. But to do that, we need to discuss the effects of the mineralocorticoid aldosterone. Want more #CME on this? Go to ckd-ce.com/category/mra/
47) #Aldosterone is a mineralocorticoid that participates in the control of #bloodpressure and homeostasis through the regulation of salt and water reabsorption in the kidneys (and colon). 
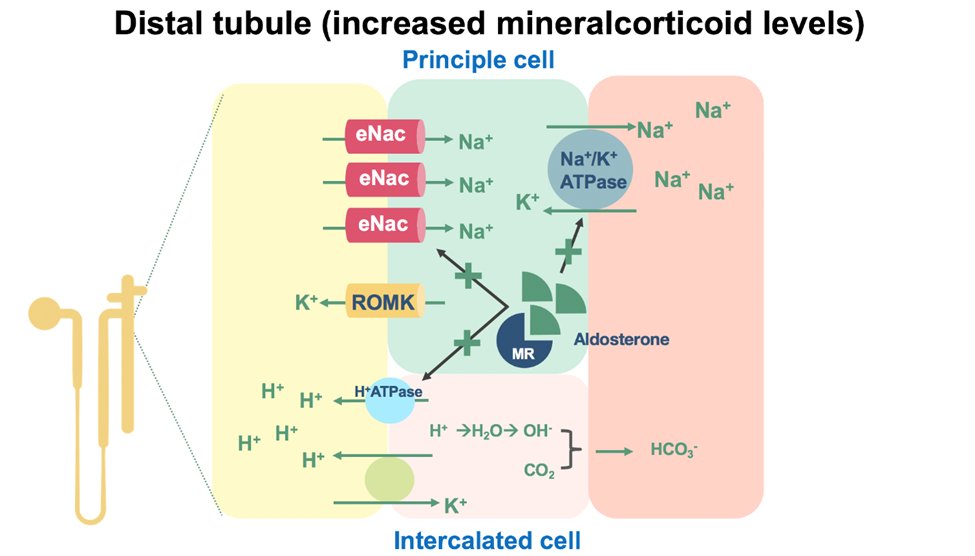
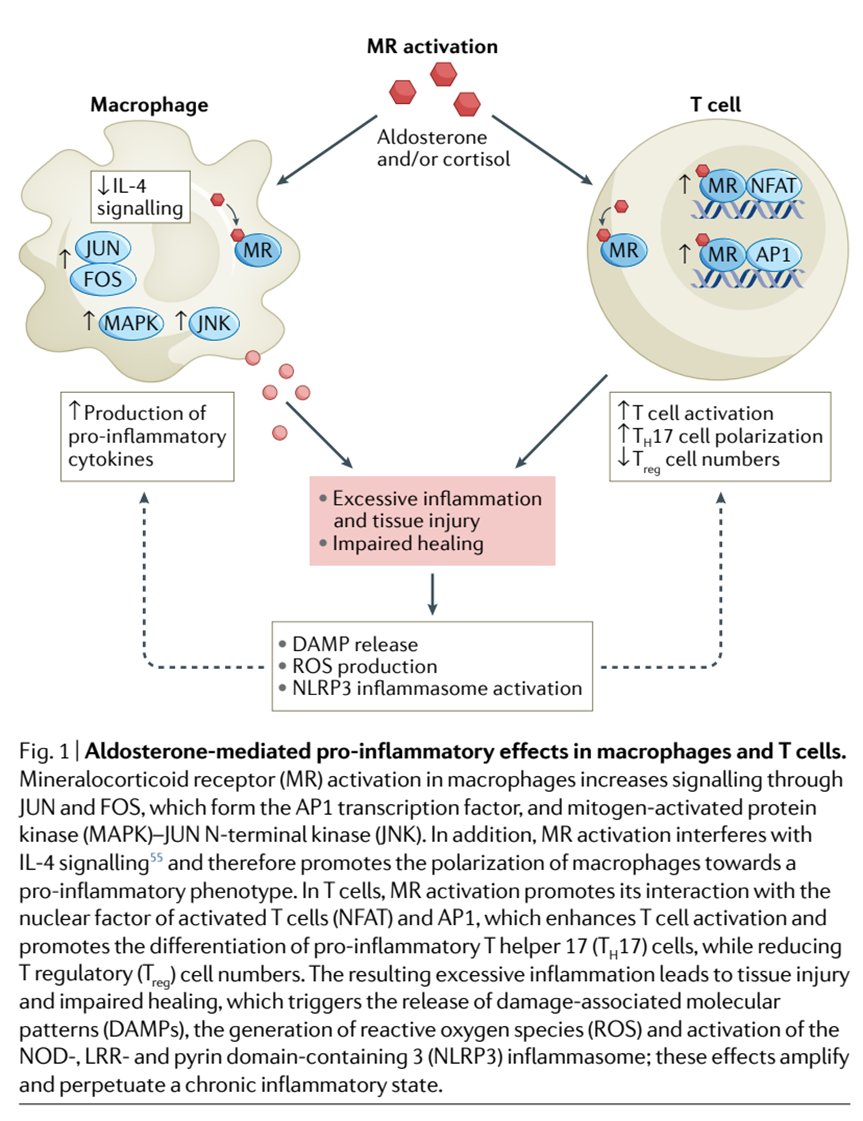
48) Aldosterone OVERPRODUCTION➡️kidney & #CV injury via inflammation, tissue remodeling, & fibrosis. In the kidney, it induces reactive oxygen species (#ROS) production through NADPH oxidase or mitochondrial activity, inducing podocyte damage, fibrosis & inflammation.
50) Aldosterone also contributes to pro-inflammatory activity in macrophages and T cells leading to production of pro-inflammatory cytokines, T-cell activation, inflammation, & tissue injury.🔓nature.com/articles/s4158… 
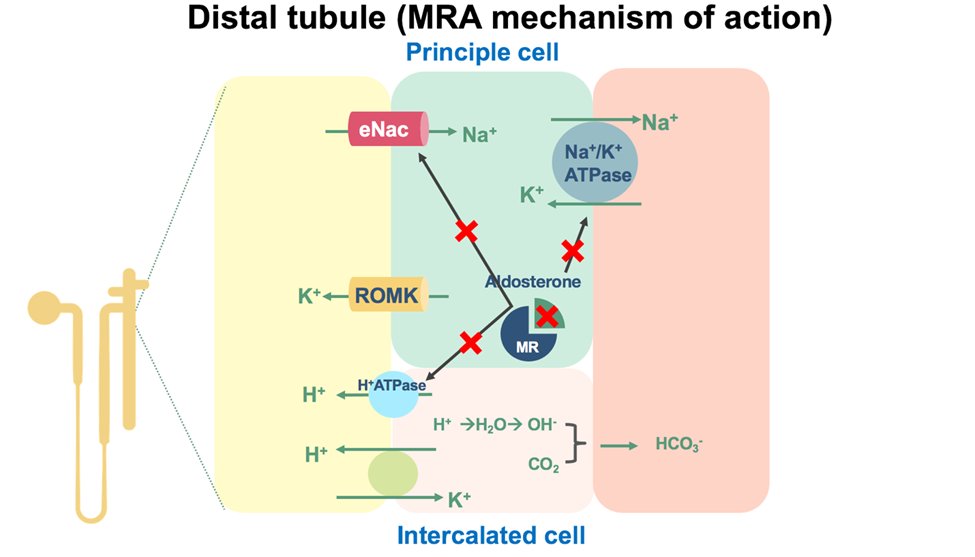
51) Mineralocorticoid receptor antagonists #MRAs are potassium-sparing antihypertensives that do just as their name suggests: inhibit mineralocorticoid activity at the mineralocorticoid receptor impairing mechs of salt reabsorption… but as you’re about to learn, do much more! 
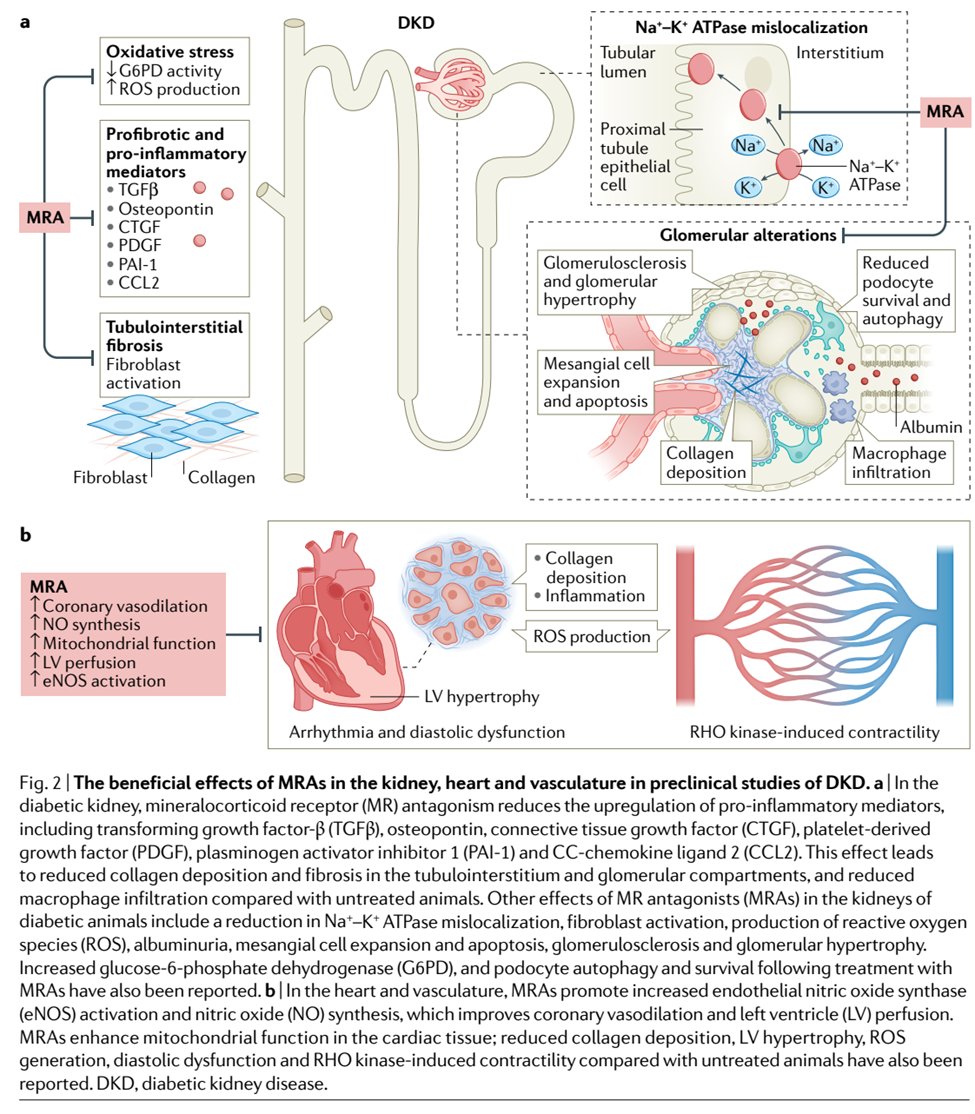
52) Preclinical data reveal #MRAs:
--reduce oxidative stress, proinflammatory mediator activity and tubulointerstitial fibrosis
--contribute to glomerular (and cardiovascular) remodeling
--⬇️ albuminuria
nature.com/articles/s4158…
--reduce oxidative stress, proinflammatory mediator activity and tubulointerstitial fibrosis
--contribute to glomerular (and cardiovascular) remodeling
--⬇️ albuminuria
nature.com/articles/s4158…
53) Steroidal (spironolactone & eplerenone) vs nonsteroidal (finerenone & esaxerenone) MRAs: What are potential benefits of nonsteroidal?
a. less anti-androgenic & progestogenic activity
b. ⬇️hyperkalemia risk
c. ⬆️anti-inflammatory/antifibrotic activity
d. all of the above
a. less anti-androgenic & progestogenic activity
b. ⬇️hyperkalemia risk
c. ⬆️anti-inflammatory/antifibrotic activity
d. all of the above
54) The anti-androgenic & progestogenic adverse effects w/steroidal #MRAs, however less apparent with eplerenone, are suboptimal . . . and
Preclinical models suggest more effective anti-inflammatory and antifibrotic activity w/nonsteroidal MRAs
pubmed.ncbi.nlm.nih.gov/30664703/
Preclinical models suggest more effective anti-inflammatory and antifibrotic activity w/nonsteroidal MRAs
pubmed.ncbi.nlm.nih.gov/30664703/
55) Clinical data w/steroidal MRAs: multiple clinical studies have demonstrated reduced #albuminuria with steroidal #MRAs like #eplerenone or #spironolactone, but #hyperkalemia remains an overwhelming adverse effect. 
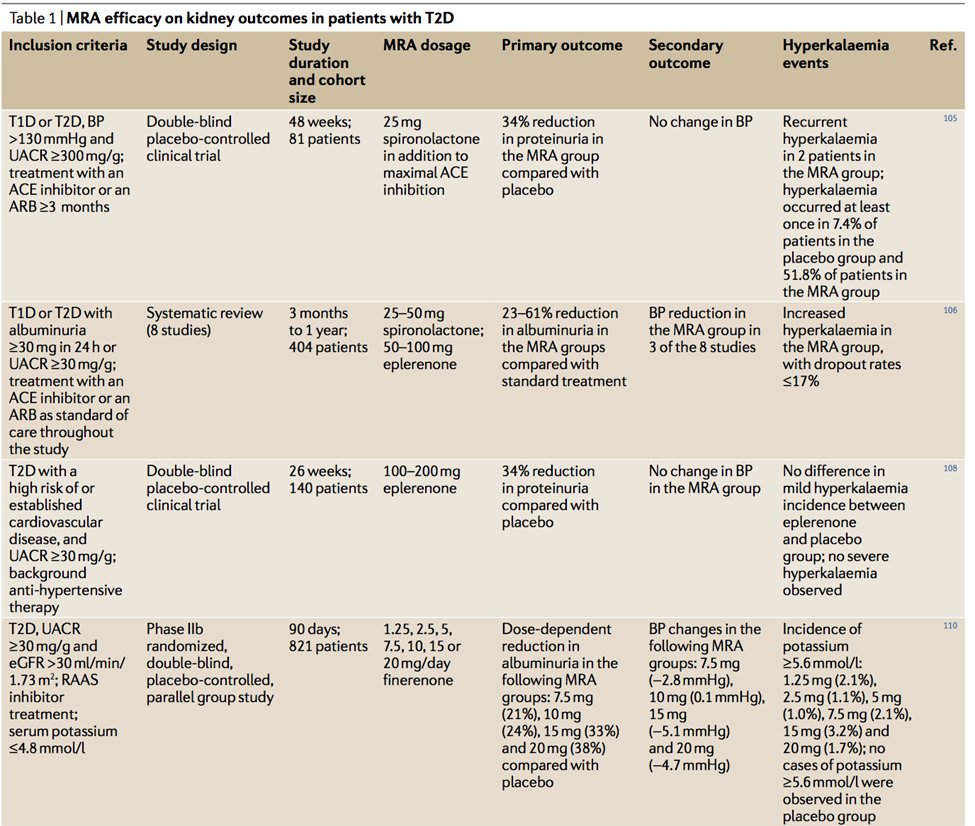
56) Clinical data w/nonsteroidal MRAs demonstrated various combinations of reduced albuminuria and/or reduction in primary composite outcome of kidney failure, sustained decrease in eGFR of 40% or more, or death of renal cause. 
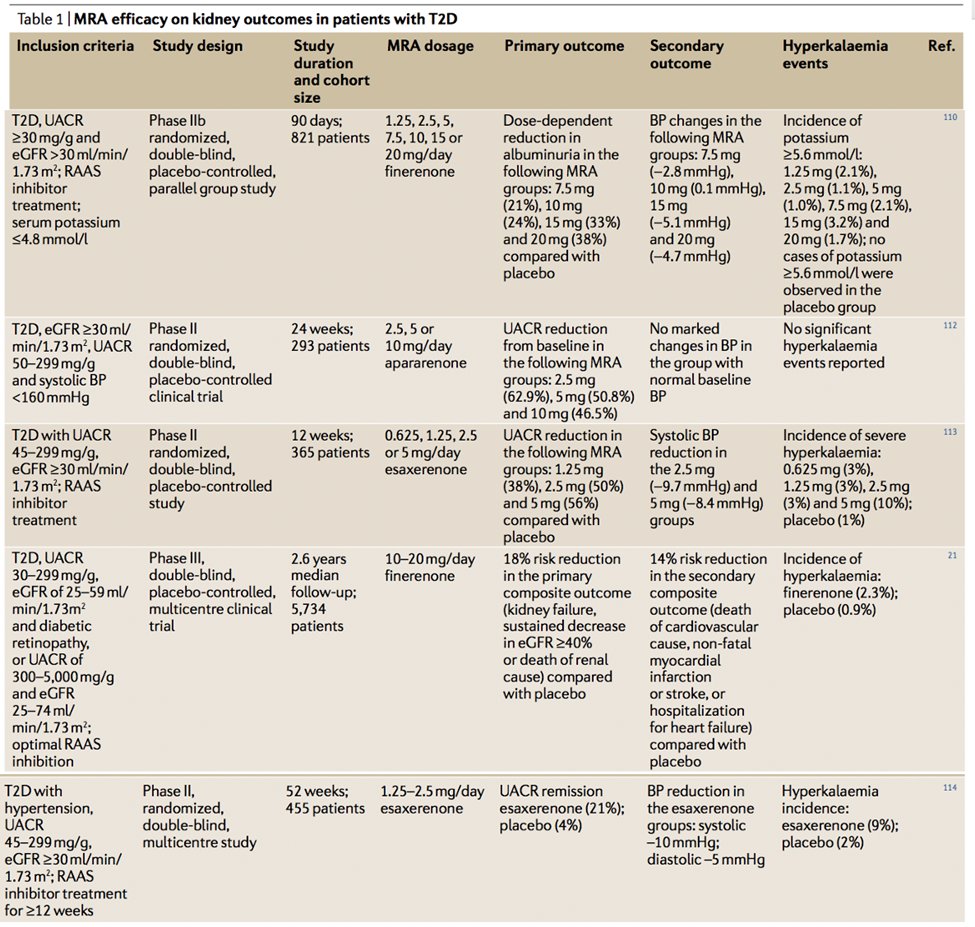
57) #FIDELIO-DKD, #RCT of finerenone vs placebo in CKD outcomes in #T2D vs placebo. Primary outcome: kidney failure, sustained eGFR decrease > 40% or death from any renal cause, N = 5674, favored finerenone, 17.8% event rate vs 21.1% w/placebo
🔓nejm.org/doi/10.1056/NE…
🔓nejm.org/doi/10.1056/NE…
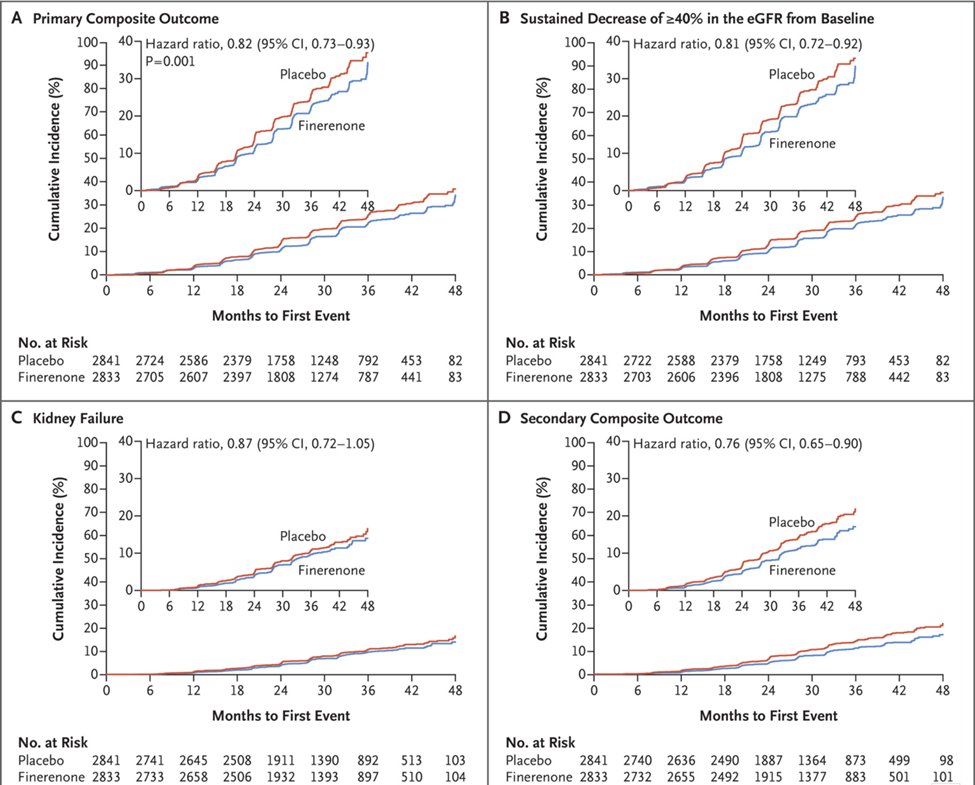
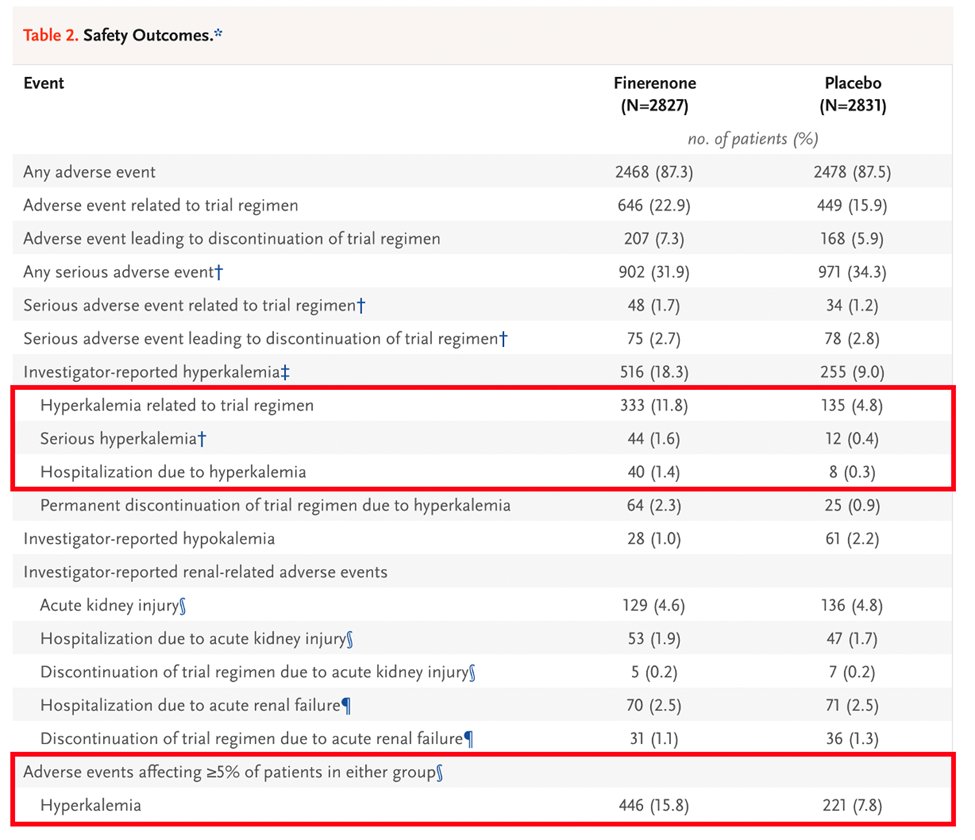
58) That #FIDELIO-DKD HR was 0.82 (95% CI 0.73-0.93; p = 0.001). But what about safety? #Hyperkalemia is still an issue; serious hyperkalemia occurred in 1.6% vs 0.4% in placebo group 
59) To date, no head-to-head RCT have been performed to compare kidney outcomes or frequency of hyperkalemia, steroidal vs nonsteroidal MRAs, but there is likely added benefit of nonsteroidal MRAs like finerenone through reduction in albuminuria & #DKD progression.
60) As nonsteroidal MRAs have proven difficult to prescribe or obtain insurance coverage, if unable to prescribe a nonsteroidal MRA, a steroidal MRA for anti-albuminuric effects should be considered.
61) So back to our case: You started pt on semaglutide 3 months ago. BP 128/75; Na 140, K 4.5, BUN 30, Crea 1.7, A1c 6.5 & #UACR still elevated at 600mg/g. What do you do next?
a. Discharge from clinic
b. target BP <120/80
c. start finerenone
d. start a DPP-4 inhibitor
a. Discharge from clinic
b. target BP <120/80
c. start finerenone
d. start a DPP-4 inhibitor
62) Hopefully no one missed this . . . start finerenone. If unavailable, initiate spironolactone or eplerenone for the antialbuminuric effects. And with that, you just earned 0.75hr CE/#CME! Go to ckd-ce.com/dkd4/ to claim it. I am @sophia_kidney. FOLLOW US!
• • •
Missing some Tweet in this thread? You can try to
force a refresh