1/ Atypical CLOT- a tweetorial
I recently saw a controversial tweet arguing against tx of chronic clot and restricting tx SOLEY to the CFV/iliac. While I agree (for the most part)- data is limited. At the end of the day we care about the pt, and not every pt is the same! Case➡️
I recently saw a controversial tweet arguing against tx of chronic clot and restricting tx SOLEY to the CFV/iliac. While I agree (for the most part)- data is limited. At the end of the day we care about the pt, and not every pt is the same! Case➡️

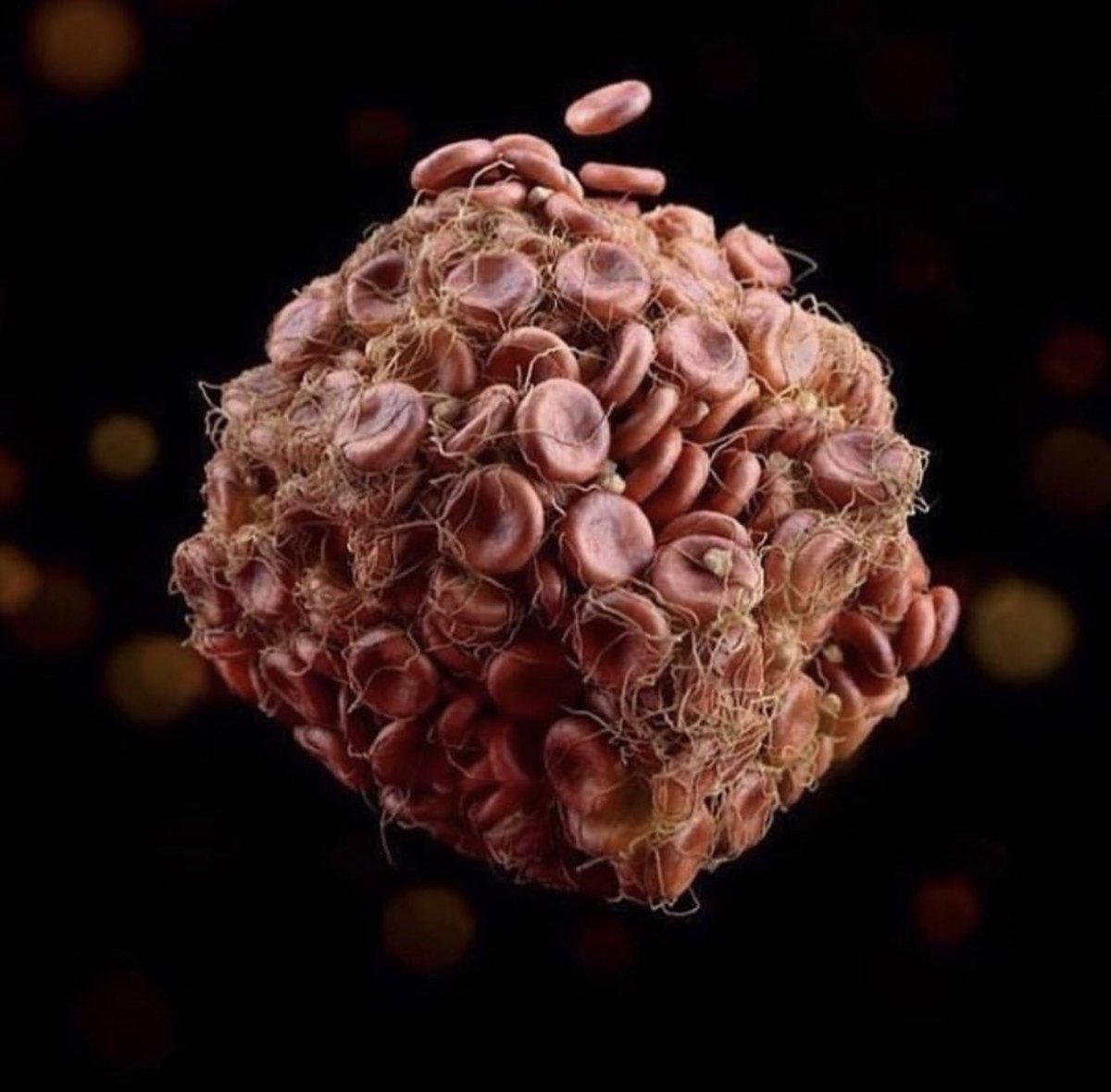
2/ Pathophysiology of chronic #clot formation.
It’s important to recognize the lesions that can form after a clot:
Spurs/Webs
Rokitansky/NIVL/fibrosis
Your pts CEAP >5 always consider for non thrombotic obstructions! Consider #IVUS if things don’t fit!
It’s important to recognize the lesions that can form after a clot:
Spurs/Webs
Rokitansky/NIVL/fibrosis
Your pts CEAP >5 always consider for non thrombotic obstructions! Consider #IVUS if things don’t fit!

3/ Clot is in a constant state of evolution. #Fibrin—> #Collagen.
Unfortunately many patients present in the subacute or late phase of #clot development which hinders many of our treatment approaches.
7️⃣days- 20% collagen
1️⃣5️⃣ days- 50% collagen
2️⃣1️⃣days- 80% (!!) collagen
Unfortunately many patients present in the subacute or late phase of #clot development which hinders many of our treatment approaches.
7️⃣days- 20% collagen
1️⃣5️⃣ days- 50% collagen
2️⃣1️⃣days- 80% (!!) collagen

3/ When to tx?
In a rare subset of patients with CFV junction or deep femoral clot symptoms sometimes are not controlled with conservative management. I’ve noticed this more in my orthopedic patient that continue to suffer from limited mobility post event. SYMPTOMS MATTER
In a rare subset of patients with CFV junction or deep femoral clot symptoms sometimes are not controlled with conservative management. I’ve noticed this more in my orthopedic patient that continue to suffer from limited mobility post event. SYMPTOMS MATTER
5/ Young
These Pts often are placed on OAC and due to limited mobility the amount of PTS I’ve seen is somewhat eye opening. What’s also worrisome is many of these patients are young with no other issues.
My patient: 2 months after DVT, compliant with xarelto
These Pts often are placed on OAC and due to limited mobility the amount of PTS I’ve seen is somewhat eye opening. What’s also worrisome is many of these patients are young with no other issues.
My patient: 2 months after DVT, compliant with xarelto

6/ Mobility
Limited mobility reduces their ability to wear/tolerate compression and also just getting them on. Also is the data with compression that good? 😔30-65% of patients will fail compression stockings
Raju S, Hollis K, Neglen P
Ann Vasc Surg. 2007 Nov; 21(6):790-5.
Limited mobility reduces their ability to wear/tolerate compression and also just getting them on. Also is the data with compression that good? 😔30-65% of patients will fail compression stockings
Raju S, Hollis K, Neglen P
Ann Vasc Surg. 2007 Nov; 21(6):790-5.

7/ Good study from JAMA on ASYMPTOMATIC patients with SVF/pop DVT post surgery. No difference in PTS if patients with Coumadin. So don’t treat right? jamanetwork.com/journals/jamai…
8/ You have to be able to separate patients in your mind CLINICALLY. The Doppler may be the same but there is a big difference between symptomatic and asymptomatic DVT patients. Does it have to do with reserve? Collateral flow? Developed saphenous system?
(Different case)
(Different case)
9/ Patient case
Young female with knee replacement, complicated by deep femoral (at junction) and significant pain/swelling. Tx conservatively. Pain continues. Doppler 3 months later with continued DVT (now chronic and occlusive). @RadialFirstBot @BotPci @CardioBot @EPeeps_Bot
Young female with knee replacement, complicated by deep femoral (at junction) and significant pain/swelling. Tx conservatively. Pain continues. Doppler 3 months later with continued DVT (now chronic and occlusive). @RadialFirstBot @BotPci @CardioBot @EPeeps_Bot
10/ After discussion with patient and referring cardiologist/orthopedic surgeon we decided to proceed with invasive assessment. Popliteal access ➡️ venography/IVUS. Significant fibrosis/chronic clot deep femoral and down. Iliac and CFV appear under perfused #Clot #Thrombectomy
11/ We elected to use ClotTriever BOLD. This is different from the original in that it has a stiffer cage and can assist with chronic thrombus. This is the only device I’ve used that can actually remove chronic thrombus. @InariMedical @Thomas_TuMD @t_intheleadcoat @kabguy 

12/ On the first few passes we yielded just small flaking matter (always frustrating), no large clot. We noticed the basket kept collapsing at the proximal SFV. @HadyLichaaMD @VenuVadlamudiMD @VladLakhter @LuaySayed @EricSecemskyMD @ShariqShamimMD @perc_surgeon @Dr_Bowser
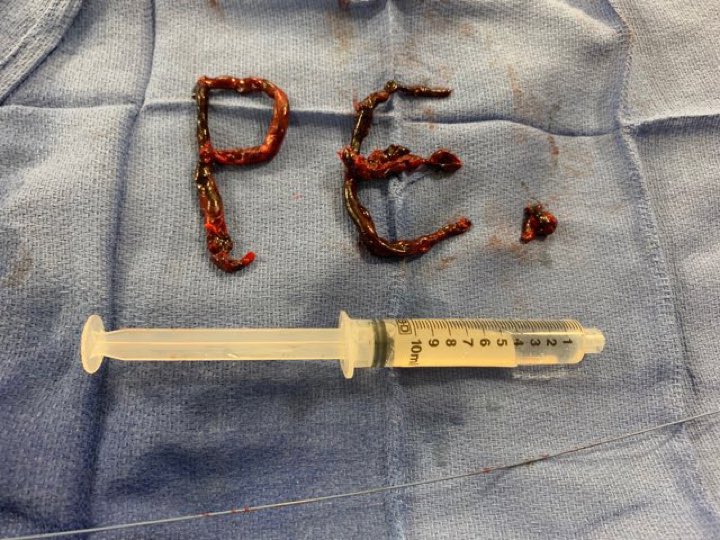
13/ Massive chronic clot at the proximal deep femoral vein @bkolskk @AmputationSuck @MarqPatton @CHICKVIR @drochohan @AustinBourgeois @RadDrDuke @SDhandMD @CHICKVIR @AustinBourgeois @ajgunnmd @ABrandisMD @IR_Doctor @LessneVIR @VIR_Li @_backtable @keithppereira
14/ due to this we balloon the region with an 8 followed by 11 balloon (in hope to macerate the clot)- sometimes I’ll put a buddy wire in to help act like a “scoring balloon” (coronary trick). @Pooh_Velagapudi @nyalborgesmd @IR_Doctor @heartdoc45 @DBelardoMD @UjjwalRastogiMD
15/ Next we take the BOLD once again, using #IVUS guidance to aim the mouth of the basket against the medial wall where the clot seemed adherent. You can also “spray paint” the clot to help see (video for education) #MechanicalThrombectomy #Thrombus
16/ This pass seemed to grasp the clot however we got stuck at the sheath so we maintained wire position and pulled the catheter out with the sheath. This is what we got! MONSTER CHRONIC CLOT @RadDrDuke @SDhandMD @CHICKVIR @AustinBourgeois @ajgunnmd @ABrandisMD @IR_Doctor 

17/ Sheath was replaced and final IVUS/venography demonstrating improvement of flow. Patient has since followed up with near resolution of her infrapop swelling. Now we are working with PT to get her mobile! @IR_Doctor @LessneVIR @VIR_Li @_backtable @keithppereira @IRKhalsa
18/ No previous treatments
Now with catheter based devices we actually have the ability to safely/effectively tx pts we always elected to tx conservatively. The data is still limited, especially below the groin, but like everything in medicine, things evolve, but WE NEED DATA!
Now with catheter based devices we actually have the ability to safely/effectively tx pts we always elected to tx conservatively. The data is still limited, especially below the groin, but like everything in medicine, things evolve, but WE NEED DATA!
Thank you @InariMedical for the BOLD and @LindsayStearns_ for the support and Dr. Edwards for reaching out to collaborate and treat this patient and give her a new lease on life! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh