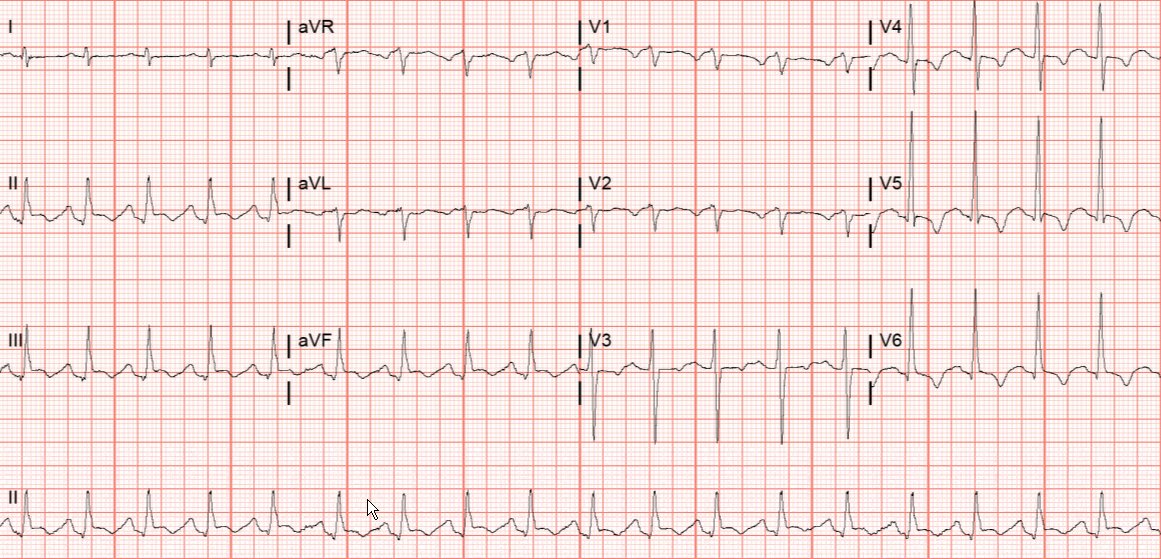
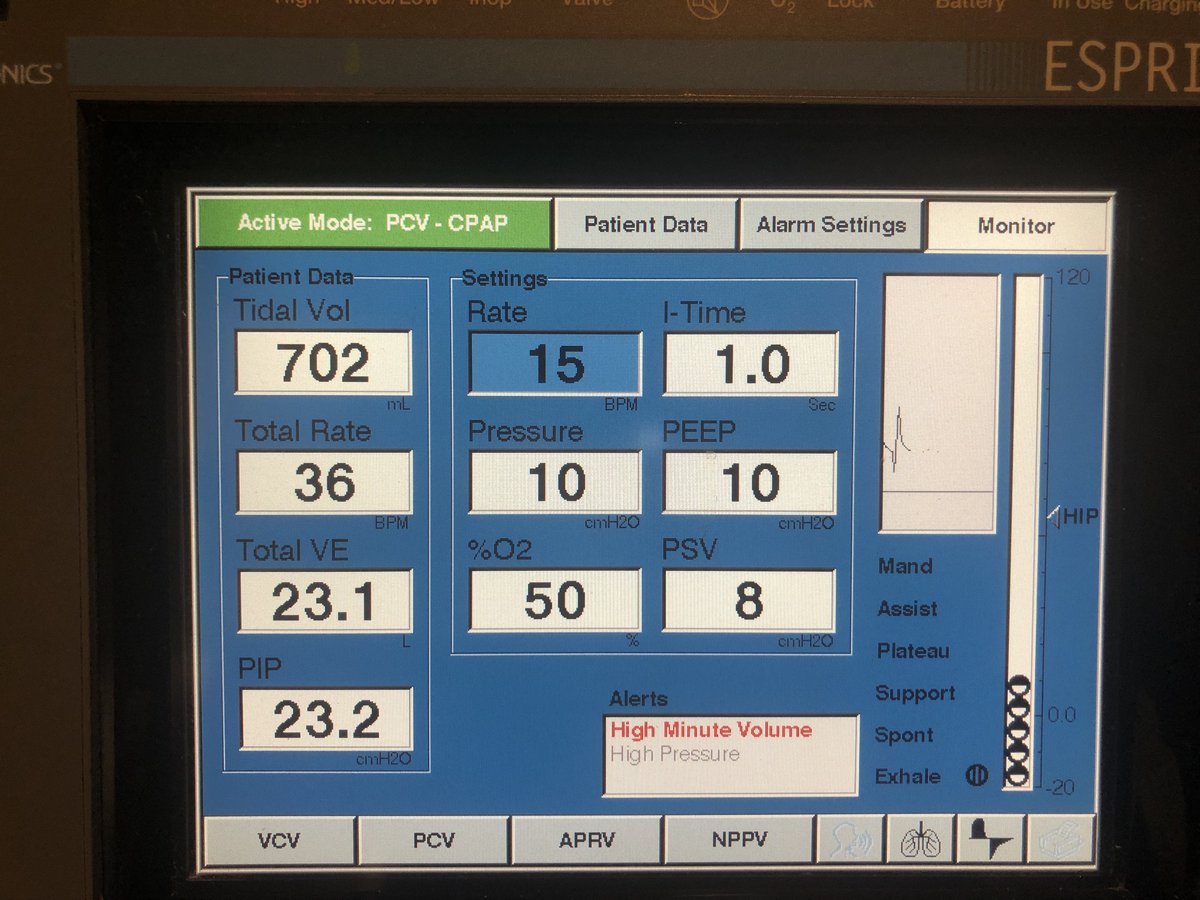
ICU stories: You start your night shift and while walking in and out each patient’s room, you see this 👇 on one ventilator's screen:
The patient (I know: I should have looked at the patient first, not at the ventilator screen... 🤷♂️) is breathing like this 😳:
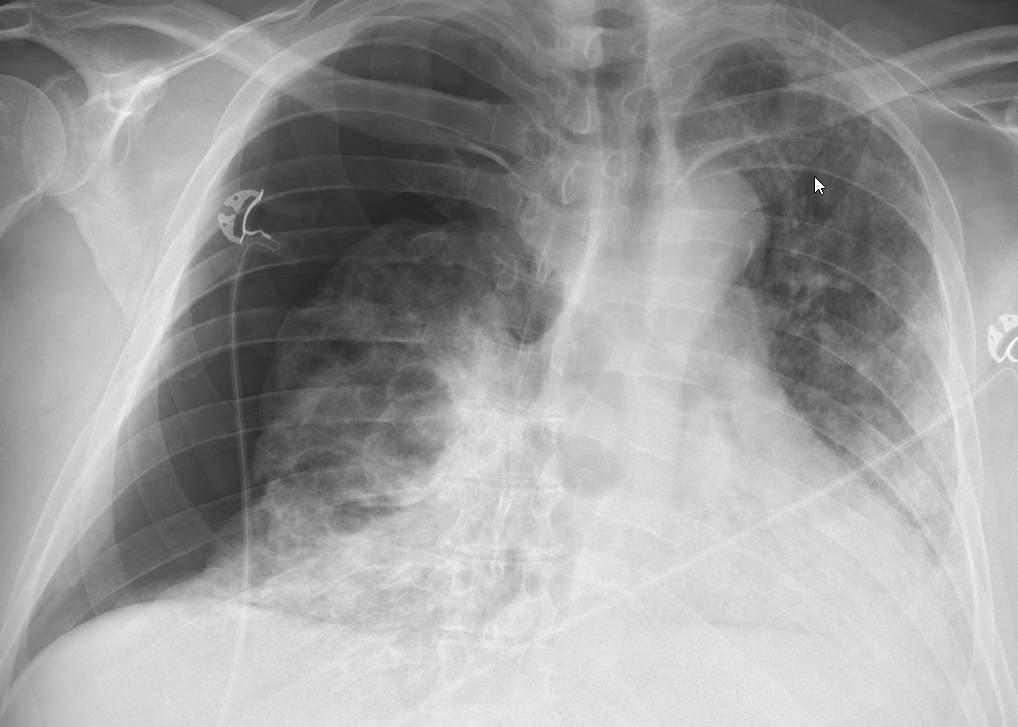
Quick chart review: middle-aged pt admitted w ARDS > 1 month ago. Already w tracheostomy + PEG. Still unable to be weaned on trach mask, despite being on "moderate" fio2 of 40-50%. On iv sedation; drowsy, hemodynamically stable. Not febrile or acidotic. No "weird" labs. CXR: 

Next step?
Let's assume that you are not busy and decide to spend some time to "study" the patient. What button(s) can you click on the ventilator to help you better understand the status of the respiratory drive?
Right! Let's try a P0.1 maneuver:
The P0.1 button is one of the most neglected buttons on a ventilator... The maneuver was described 50 years ago (Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a measure of respiratory center output in conscious man. Respir Physiol 1975; 23: 181-99)
P0.1 is a simple way to assess the respiratory drive at the bedside
P0.1 is one of the 7 pressures we should measure when someone is on the vent. The other 6 are: plateau, peak, auto-peep, driving, esophageal (not easy), and blood pressure!
P0.1 is one of the 7 pressures we should measure when someone is on the vent. The other 6 are: plateau, peak, auto-peep, driving, esophageal (not easy), and blood pressure!
The P0.1 is the pressure generated during the first 100 msec (0.1 sec) of an inspiratory effort against an occluded airway. Most modern ventilators allow the measurement of P0.1 with the click of a button. This is how to do it in a PB840:
During the occlusion, airway pressure follows the pressure generated by the respiratory muscles. The occlusion does not affect the effort because the brain needs > 0.1 sec to react to the occlusion! In healthy spontaneously breathing adults, P0.1 is ~1 cm H2O; ...
...in ventilated pts, a value > 3-4 cm H2O is associated w ⬆️ effort. Our pt had a P0.1 close to 13… Since there is breath-by-breath variability, most ventilators measure the average of 3-5 breaths. An “abnormal” respiratory drive on MV, is represented by P0.1 < 1.0 or > 3.0-4.0
An "out of range" P0.1 is considered a risk factor for diaphragmatic + lung injury. ⬆️ values may be due to insufficient support while ⬇️ values suggest over-assistance. P0.1 can be used to adjust PEEP in pts w hyperinflation, to predict weaning failure (or success!) etc
A P0.1 > 5-6 cm while pt is receiving full ventilation is worrisome. If there is no reason for ⬆️respiratory drive (remember that I wrote initially: no fever/acidosis), you have to ⚖️ the potential injury risks w benefits of allowing the pt to continue breathing spontaneously
So, what should we do next?
Patient did not respond to more sedation and was paralyzed that night. I saw the pt a few days later when I was on call again. Chest CT:
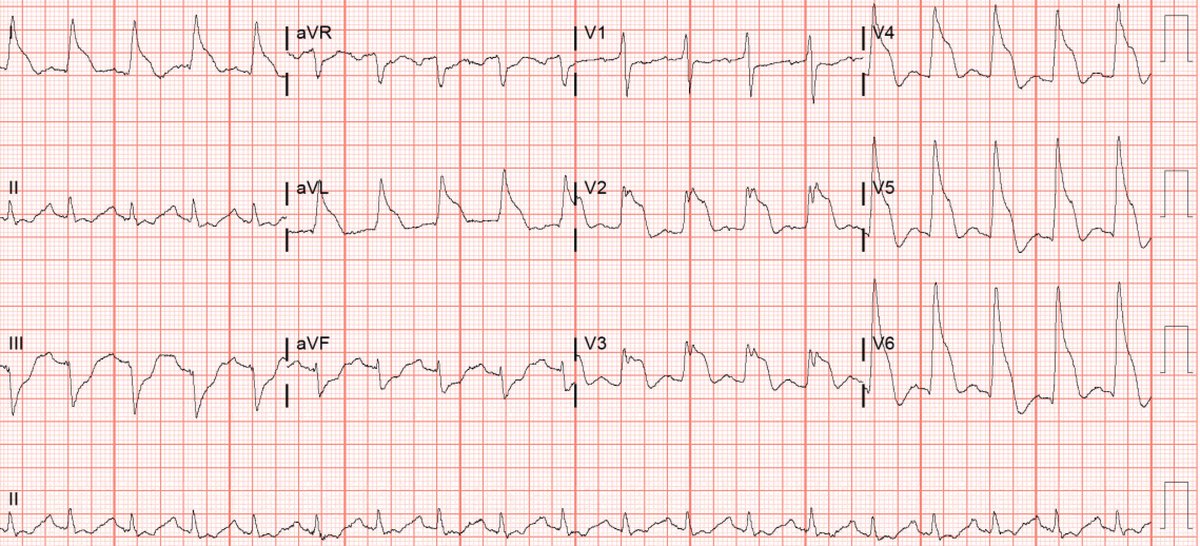
👆he had developed sc emphysema, pneumomediastium and right pneumothorax. Eventually improved and was discharged to long-term acute care hospital. Readmitted a few months later with 👇 
Take-home message
Ventilators remain black-boxes but the more we familiarize ourselves w them, the more w can understand how they work, how patients breathe and how their interaction (synchrony) can be optimized
Thanks for reading!
Follow @msiuba @Thind888 for more details!
Ventilators remain black-boxes but the more we familiarize ourselves w them, the more w can understand how they work, how patients breathe and how their interaction (synchrony) can be optimized
Thanks for reading!
Follow @msiuba @Thind888 for more details!
#FOAMed #FOAMcc #MedTwitter #MedEd #EMBound @siddharth_dugar @HeyDrNik @NickjohnsonMD @nickmmark @cjosephy @critconcepts @MediCasos @RogerAlvarezDO @MegriMohammed
Excellent ? from @icmteaching regarding a trial of "spontaneous mode". I remembered I tried different modes+settings; I did not save everything but this is when I tried PS (PS 8 + PEEP 10). Lower PS was followed by RR in the 40-50s; higher PS followed by tidal volume 800-900 cc 
Even though the most reliable method to measure patient's muscle effort (Pmus) is the analysis of esophageal pressure-volume loops using the Campbell diagram, we have data from bench studies that there is significant correlation between P0.1 and Pmus; DOI doi.org/10.53097/JMV.1…
• • •
Missing some Tweet in this thread? You can try to
force a refresh