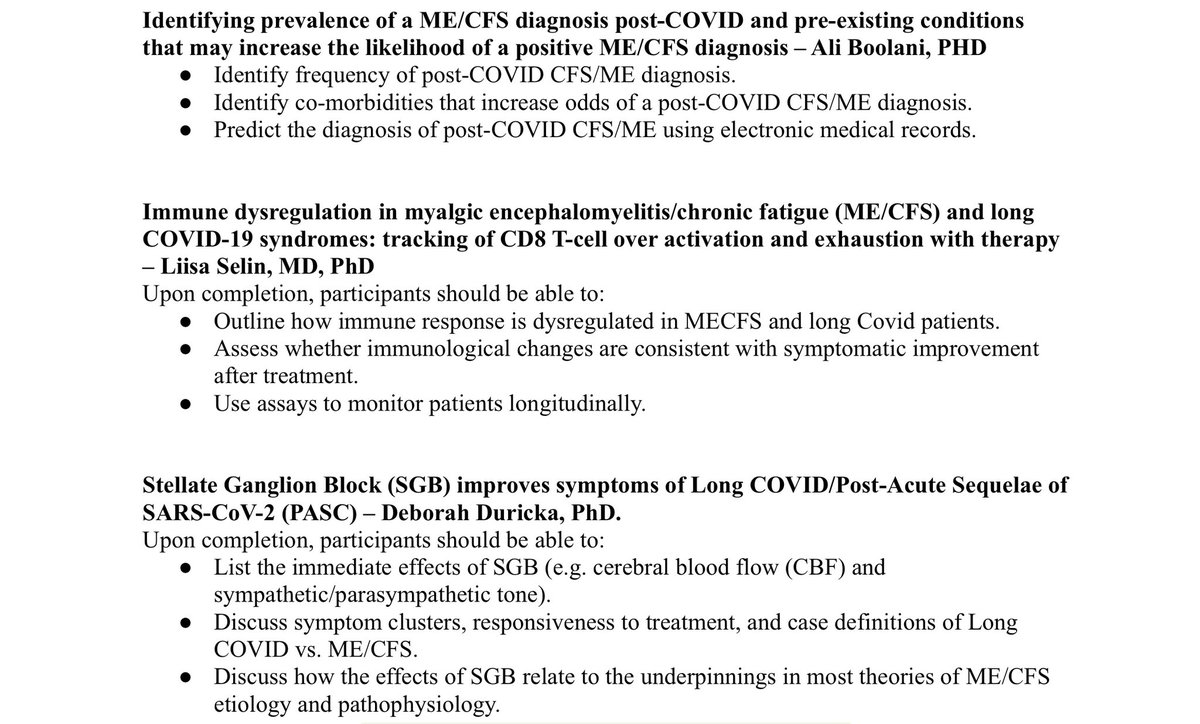
Up next at #IACFSME: three presentations under the Immunology track. Starts at 1:30 pm ET.
#CovidIsNotOver #mecfs #LongCovid #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #COVID19 @itsbodypolitic

Background info on Dr. Roy's paper: Here we report a potential mouse model that displays ME/CFS pathologies after two weeks of gavaging with 5 mg/kg bwt of compound # 13563531, a potent autophagy inhibitor.
Dr. described a set of procedures to develop the mouse model, most of which focused on the inhibition of autopathy.
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
Jessica Maya from Cornell is focused on how the immune system and cellular metabolism are dysregulated in ME/CFS.
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
Specifically T cell exhaustion as a theory in ME/CFS
Flow cytometry is the key methodology and identifies different exhaustion markers
ME/CFS T cells have an exhausted subset of T cells not seen in healthy controls
Continued work will shed more light on the potential for using immune modulators as a treatment for ME/CFS
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
More info on Dr. Roy and the findings from the mouse model: the model replicates PEM in mice (treadmill exercise), and gender differences also appear in the mouse model.
3rd talk is Immune Comparison of Male and Female ME/CFS Patients, by Kristina K Aenlle
Men with ME/CFS have increased T cells at baseline vs controls, and women have increase in B cells
For cytokines, women show increase in pro-inflammatory cytokines, but men do not in this study.
Question for further research: are ME/CFS patients displaying accelerated aging?
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
From the Q&A, for Dr. Maya: Has T cell exhaustion been observed in Long Covid patients as well?
A: There have been some studies investigating pd1 and exhaustion in long-covid, some studies in JCI insight claim increased PD1
A: There have been some studies investigating pd1 and exhaustion in long-covid, some studies in JCI insight claim increased PD1
More Q&A w/Dr. Maya: Can the T-cell exhaustion theory explain the co-ocurrence of the major symptoms of ME/CFS: chronic fatigue, brain fog, chronic insomnia, OI/POTS, sensory hypersensitivity, other dysautonomic effects? If so, what are the putative causal connections?
Ans-next
Ans-next
A: If t cell exhaustion is occuring, its a change to the immune system. if your t cells are being exposed to a viral challenge for years, you will not be able to fight off other im challenges very well, so immune-related symptoms could be explained by this type of imm cell state.
• • •
Missing some Tweet in this thread? You can try to
force a refresh