Virgin coconut oil as the main fat source in a diet of 60% fructose, 20% protein, 10% fat maintains redox status and markedly improves glucose metabolism 
When animals are fed the same diet but with copra oil instead, they develop insulin resistance and advanced fatty liver.
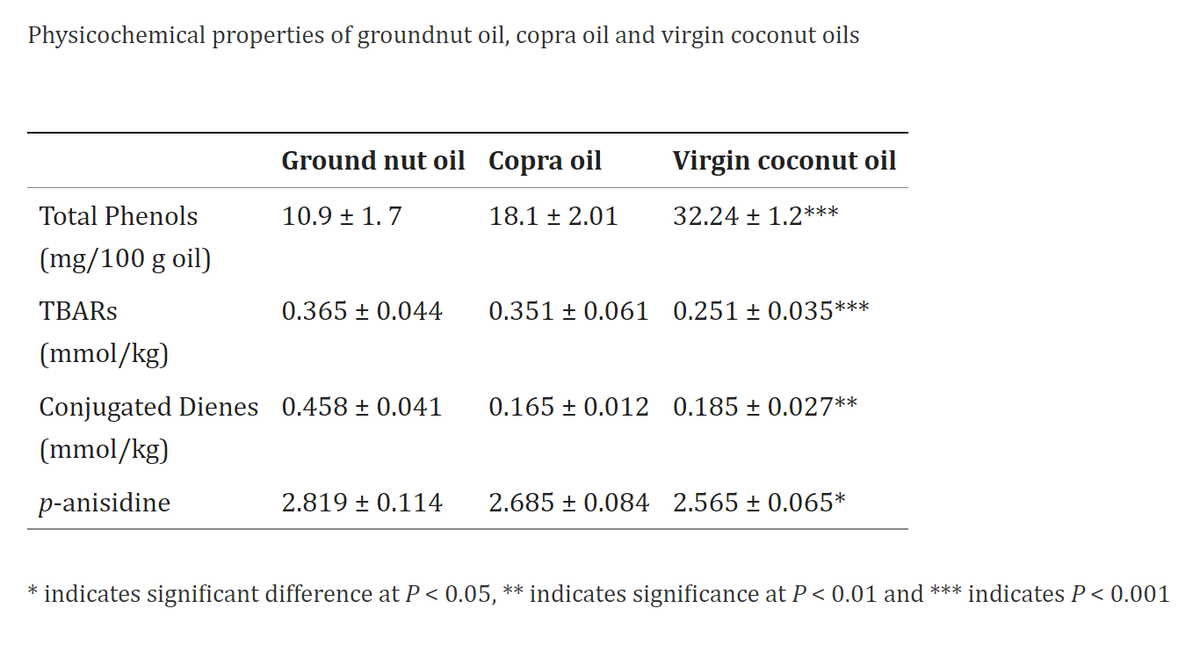
Both oils are composed of over 90% of the beneficial MCTs, so the 2-fold higher antioxidant polyphenols in virgin coconut oil seem to make the difference.

Both oils are composed of over 90% of the beneficial MCTs, so the 2-fold higher antioxidant polyphenols in virgin coconut oil seem to make the difference.

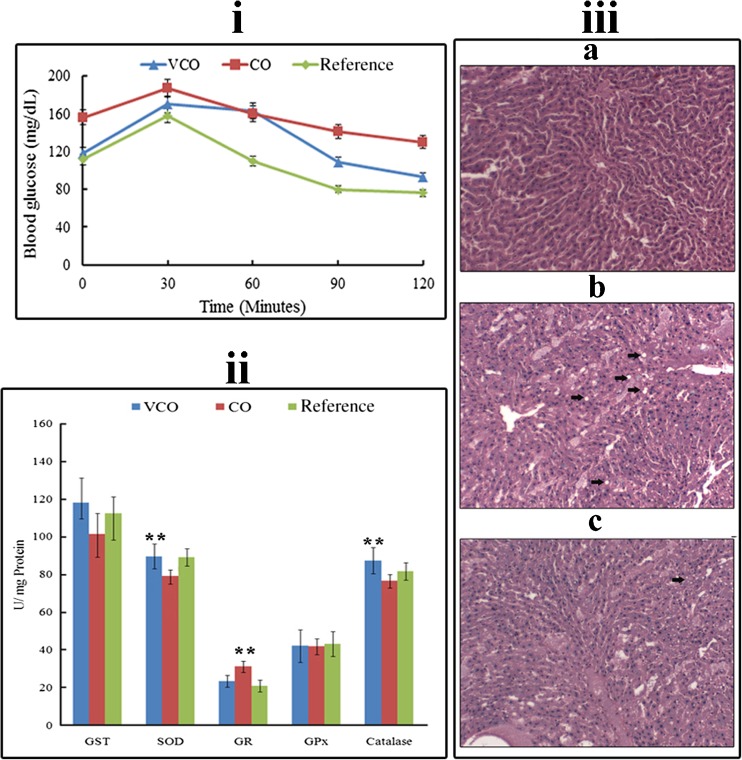
60% fructose + 10% fat as copra oil led to a 46% blood sugar increase and higher oxidative stress
60% fructose + 10% fat as virgin coconut oil only raised blood glucose by 16%, significantly increased glutathione and antioxidant enzymes, and reduced lipid peroxidation.
60% fructose + 10% fat as virgin coconut oil only raised blood glucose by 16%, significantly increased glutathione and antioxidant enzymes, and reduced lipid peroxidation.
Therefore, even if eating a high-carb low-fat diet, something akin to the Kitavans or Tsimane, eating the *wrong* kind of fat can still be detrimental even at extremely low amounts. No wonder both of those populations do so well eating lots of coconut.
https://twitter.com/JBianco215/status/1535277880598482945
Virgin coconut oil maintains redox status and improves glycemic conditions in high fructose fed rats
pubmed.ncbi.nlm.nih.gov/26788013/
#raypeat #diabetes #insulin #lchf #hclf #vegan #keto
pubmed.ncbi.nlm.nih.gov/26788013/
#raypeat #diabetes #insulin #lchf #hclf #vegan #keto
• • •
Missing some Tweet in this thread? You can try to
force a refresh