Starting at 1:40 pm ET at IACFS/ME, first panel discussion on COVID-19 related topics.
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic

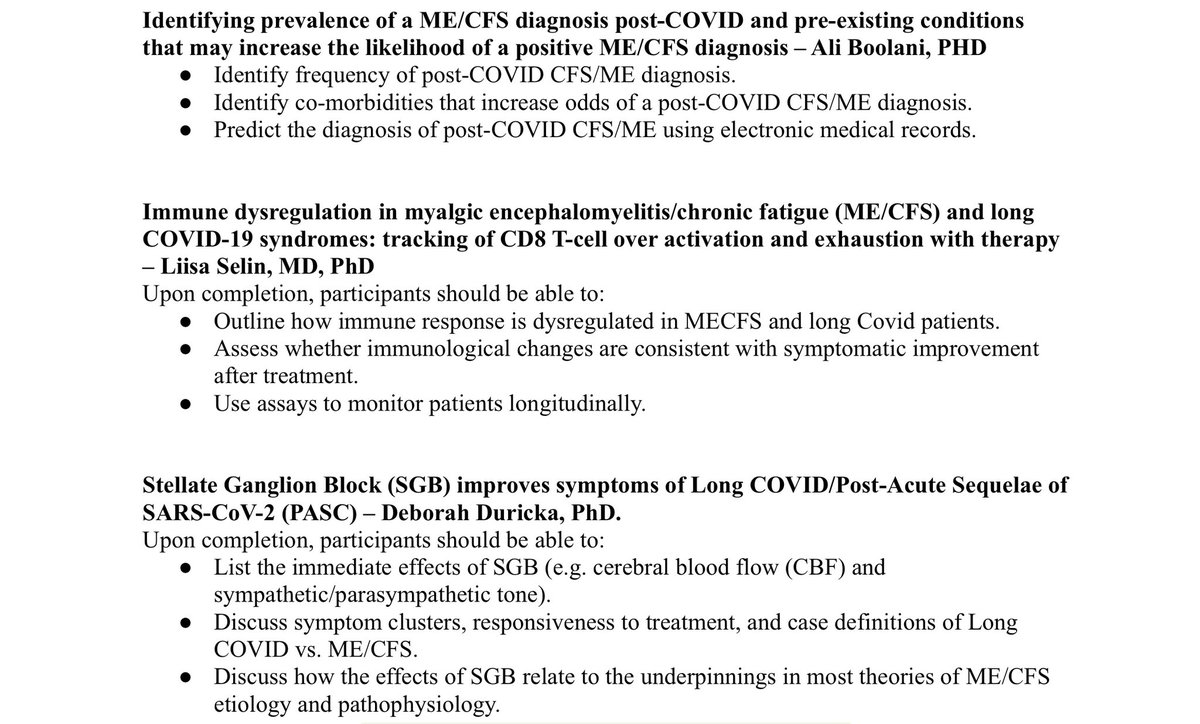
Dr. Boolani -- post-covid ME/CFS, and risk factors for that diagnosis.
Of 60,000+ patients hospitalized for C19, 8,500 developed MECFS, based on EHR analysis
Hypertension and immunosuppression were identified as important, along with certain demographic info, inc age
But, many limitations to data, given unreliability in use of diagnostic codes.
Next Dr Selin
Hypothesis based on similarity of MECFS and LC, esp increased CD4 & CD8 T cells and aberrant cytokines
Biomarker also includes: antigen over-activated exhausted CD8 T cells
Survey info shows similar symptom pattern.
Therapeutic approach: inspiritol to modulate immune system.
Info on 2 patients, one CFS, one LC. CFS: gradual improvement. LC: also gradual improvement. Both back to 80% of baseline.
Improvement also in 6 other patients.
Dr. Duricka on Stellate Ganglion Blocks for LC
Talk is based on case series published last year for 2 patients.
Data from chart review: improvement across a range of symptoms, but small N (11) limits significance.
Most improvement in fatigue, memory, problems concentrating. sleep problems, PEM, tachycardia, OI, plus MH. In some cases, patients experienced complete recovery.
Why is this treatment helping? Sympathetic block prevents sympathetically driven vasoconstriction. Improves blood & oxygen to brain stem.
1/2 -- During Q&A, an important clarification from Dr. Boolano re: hospitalized patients: these individuals were individuals who came to the hospital and were diagnosed with CFS/ME. They did not all get hospitalized.
2/2 We would have loved to have access to data from patients who were seen in the clinic however, the hospital system that contracted our lab did not allow us access to that information.
More Q&A: w/ Dr. Selin: Does exhausted T cells alone explain all the major symptoms of ME/CFS?
Yes, I actually think that all the major symptoms of ME/CFS can be explained by the state of CD8 T cell exhaustion. I have a modle slide at the end on my talk I was not able to show.
Yes, I actually think that all the major symptoms of ME/CFS can be explained by the state of CD8 T cell exhaustion. I have a modle slide at the end on my talk I was not able to show.
Special thanks to @Rivkatweets and Beth Mazur of #MEAction for bringing the SGB presentation to IACFS/ME
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
#CovidIsNotOver #mecfs #LongCovid #iacfsme #COVID19 @itsbodypolitic
• • •
Missing some Tweet in this thread? You can try to
force a refresh