Topic - Ventricular Tachycardia!
Agenda:
1- Approach to evaluating #VT
2- Management of #VT
3- Practice Cases
Please share your thoughts & input to this #tweetorial!
@ACCCardioEd @ACCinTouch #FOAMed @MichiganACC
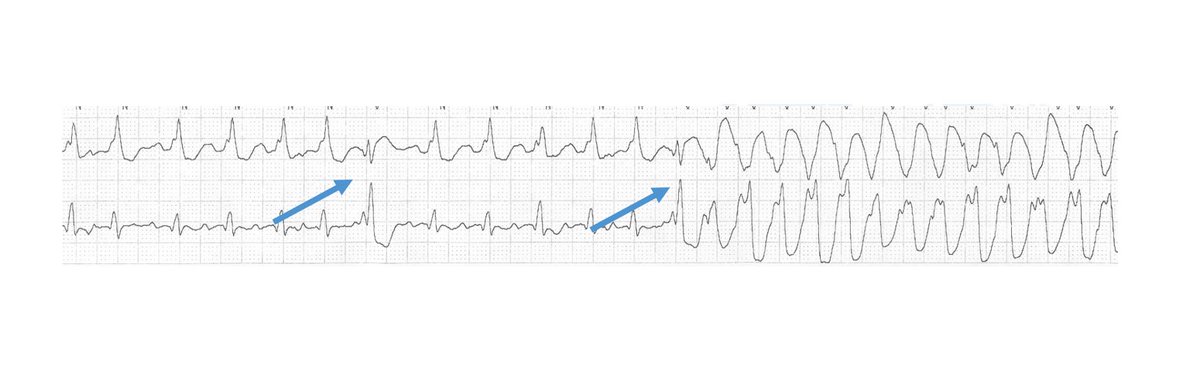
1/10 – Ventricular Tachycardia
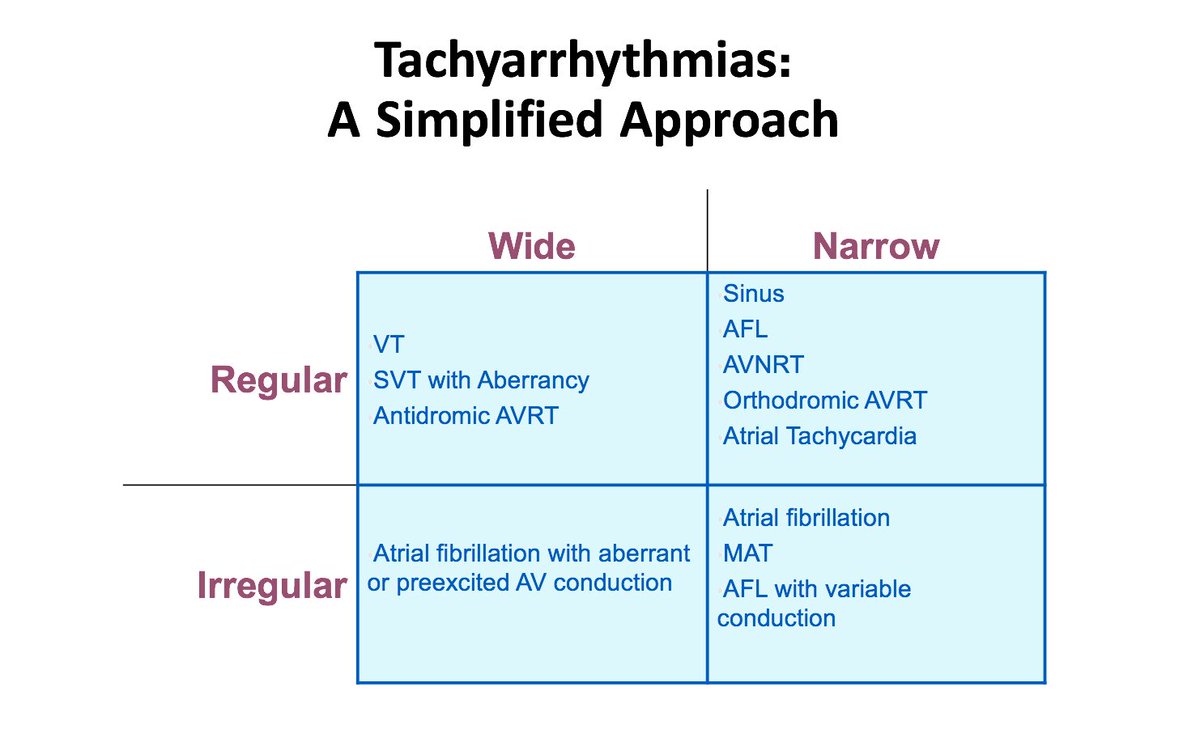
Simplified approach to evaluate tachycardia:
Rule #1 – If HD unstable ➡️ shock!
If HD stable, sit down & think.
Step # 1 - QRS: wide or narrow?
Step # 2 - Rhythm: regular or irregular?
This will narrow DDx!
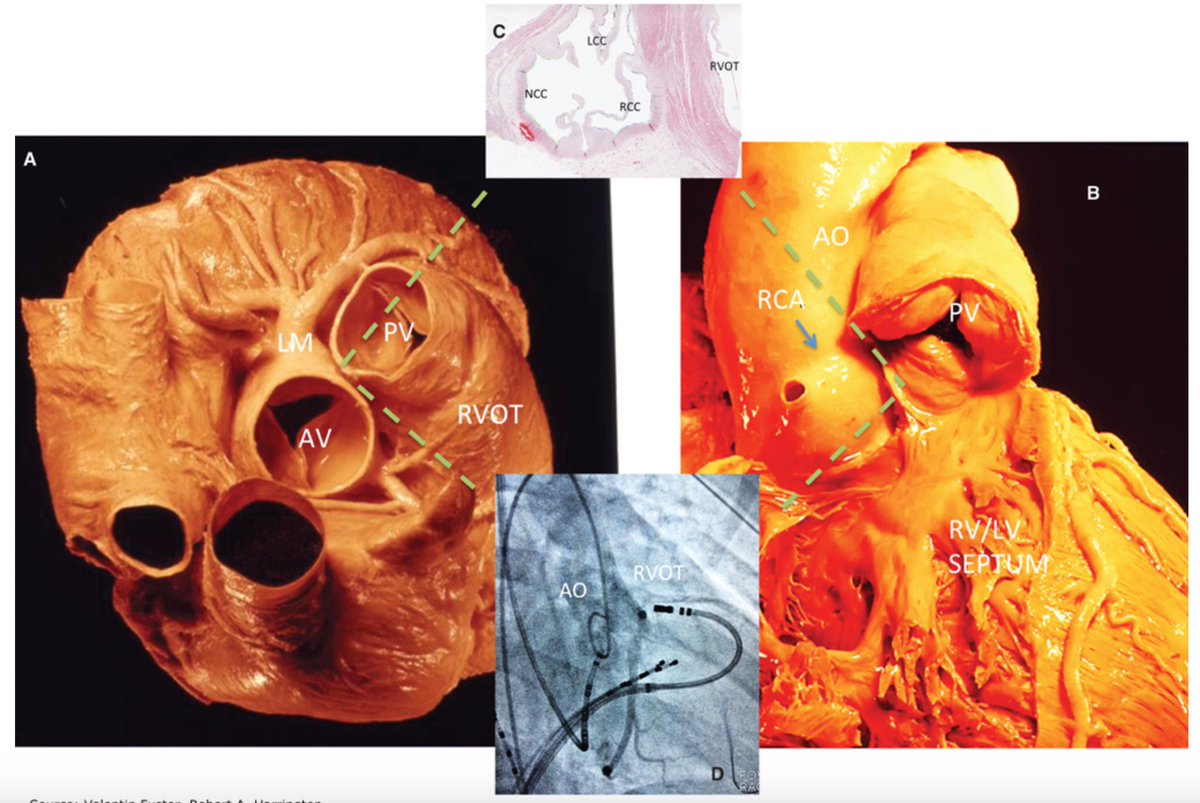
2/10 - Wide complex tachycardia
Always consider clinical Scenario!
Look for history of MI and cardiomyopathy ➡️ strongly favor #VT!
* If structural heart disease is present, you will be correct 9/10 times with diagnosis of VT!
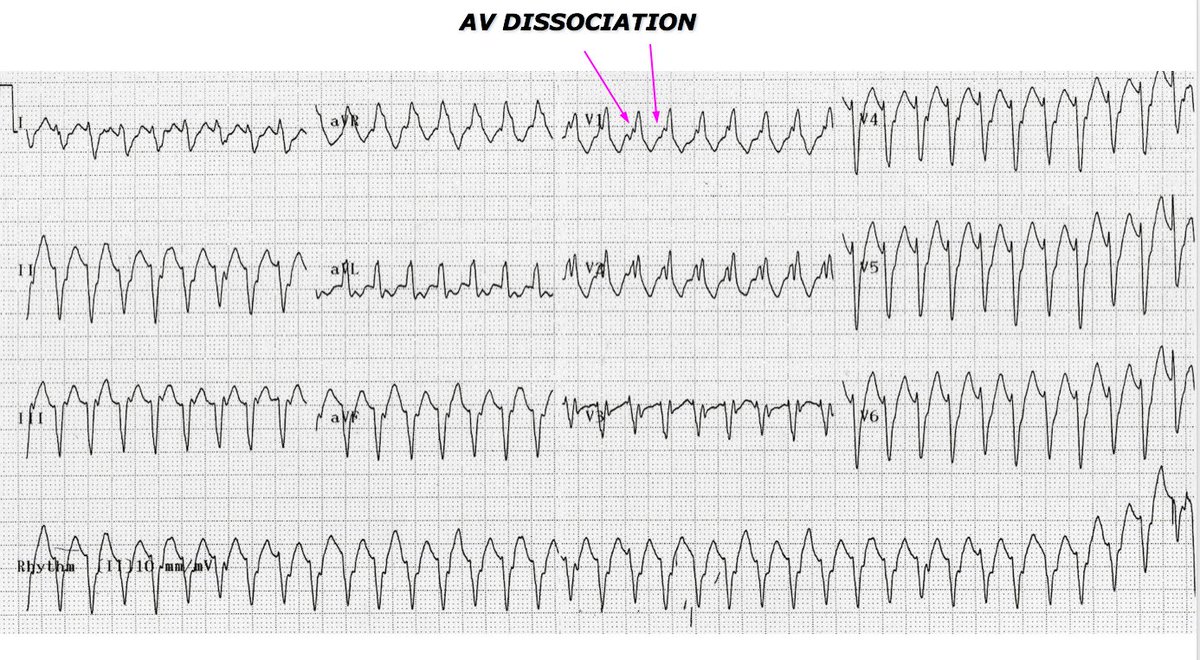
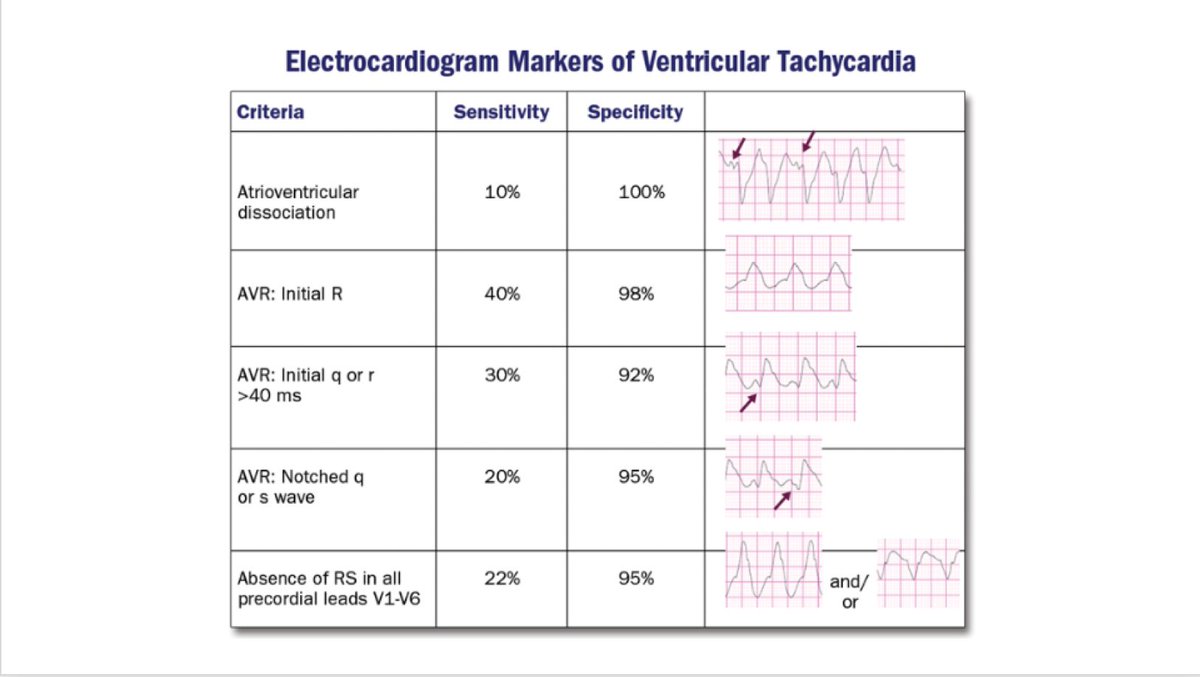
4/10 – VT from SVT (Brugada Criteria)
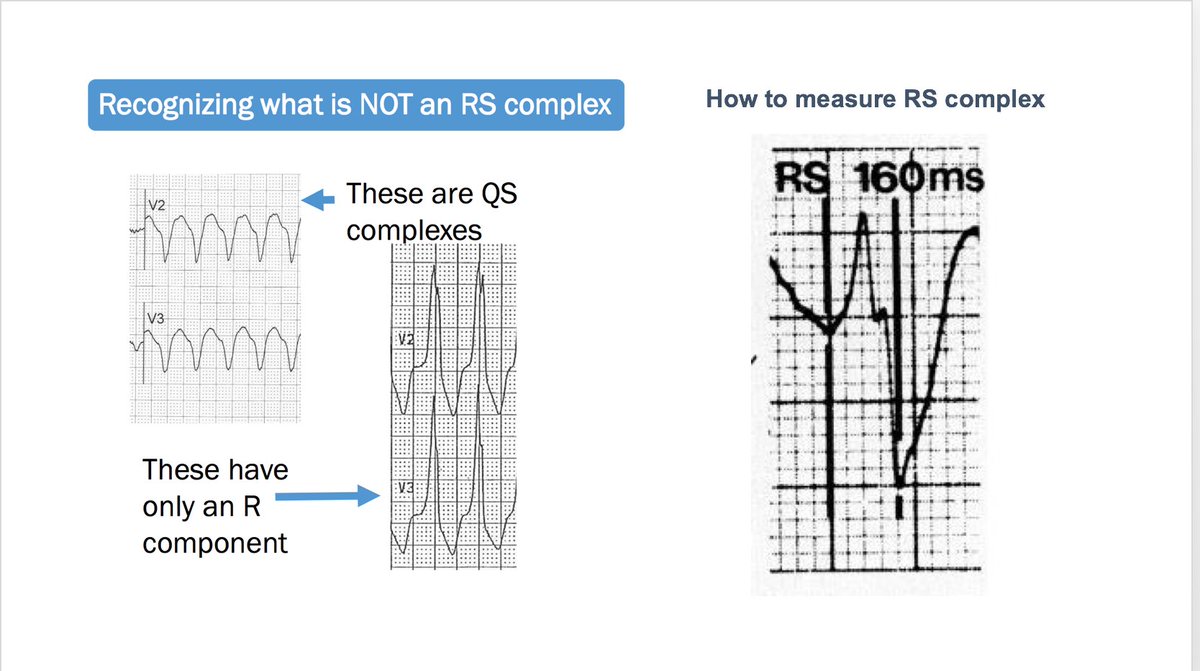
Q1) RS absent in precordial leads? If YES, it’s #VT!
Q2) If present, is RS interval > 100ms? If YES, it’s #VT!
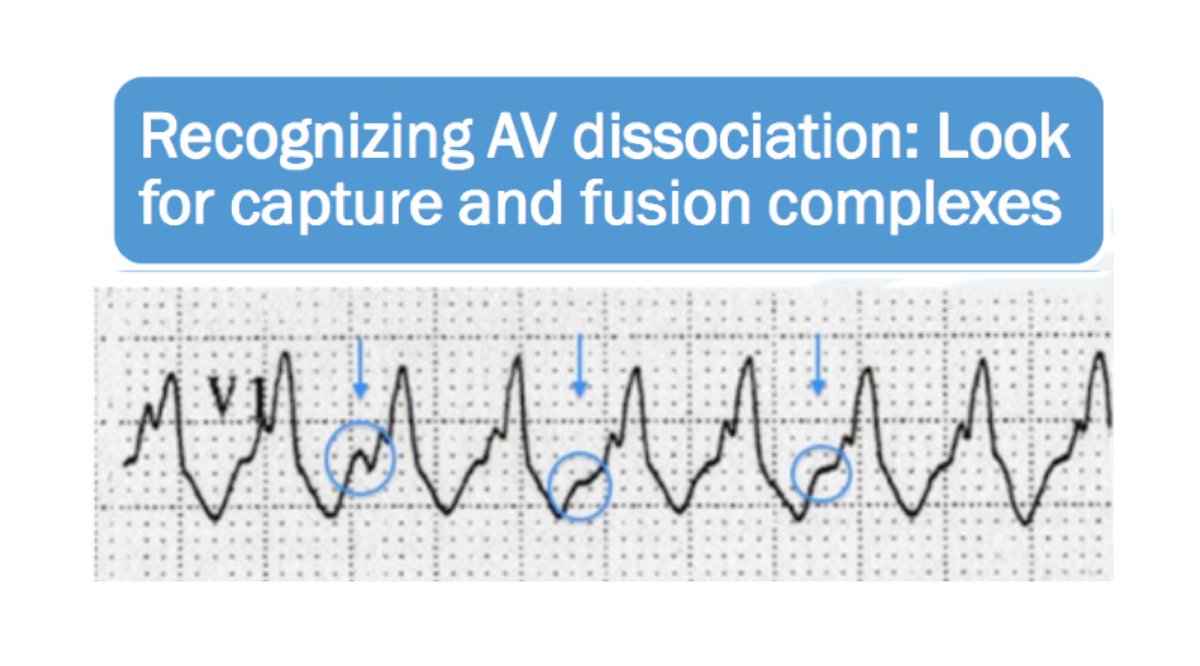
Q3) If Q1 & 2 are NO, any AV dissociation? If YES, it’s #VT!
If all Qs are NO, then ✔️QRS morphology
5/10 – VT from SVT continued...
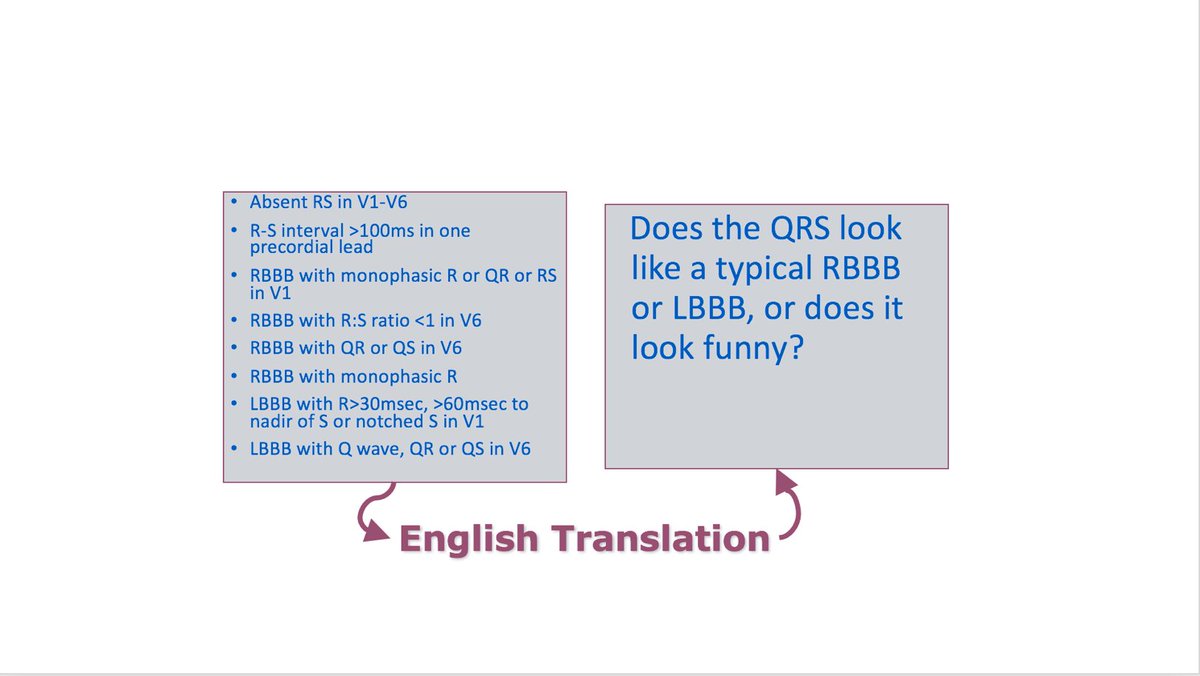
If prior 3 Qs are NO ➡️ check QRS morphology
Q4) Does QRS appear like a typical RBBB or LBBB, or does it look funny?
If funny looking, likely #VT!
Specific criteria for #VT by QRS morphology (extensive, see figure)
6/10 – Other useful #ECG findings suggestive of VT:
-Axis - Extreme AD (“northwest axis”) — QRS + in aVR & - in I / aVF
-QRS width - Very broad (RBBB > 140 ms, LBBB >160 ms)
-Q waves – sign of CAD
-Josephson’s sign – Notching near nadir of the S-wave
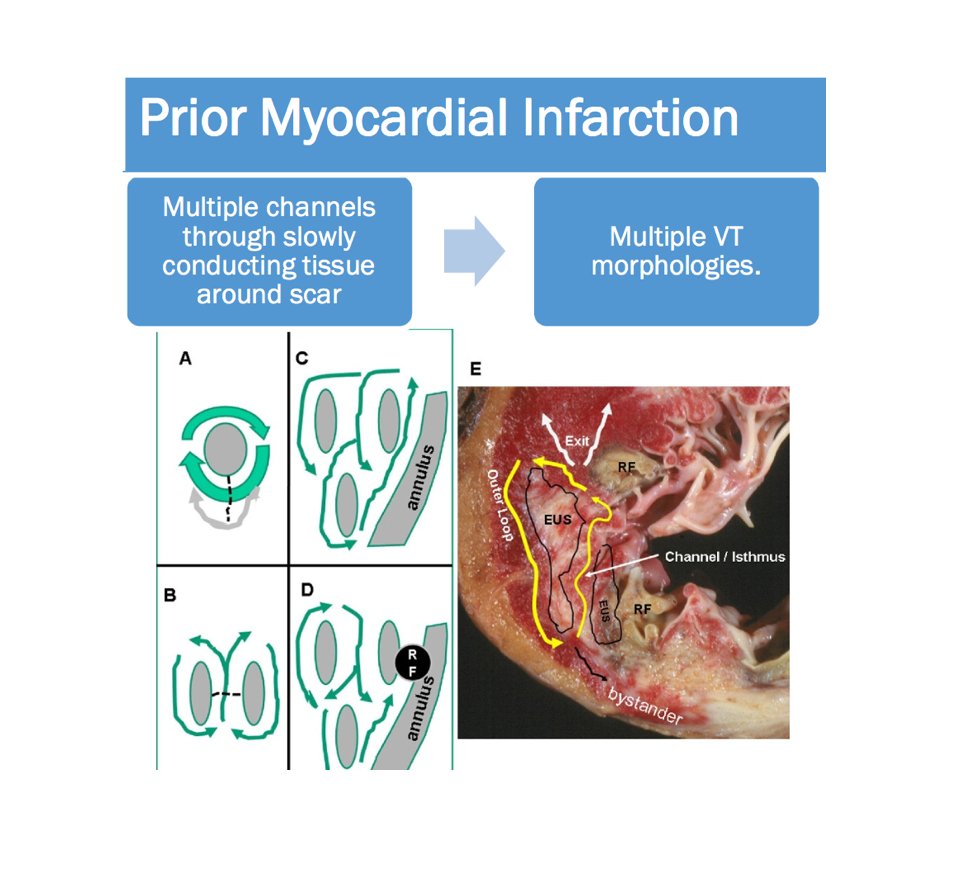
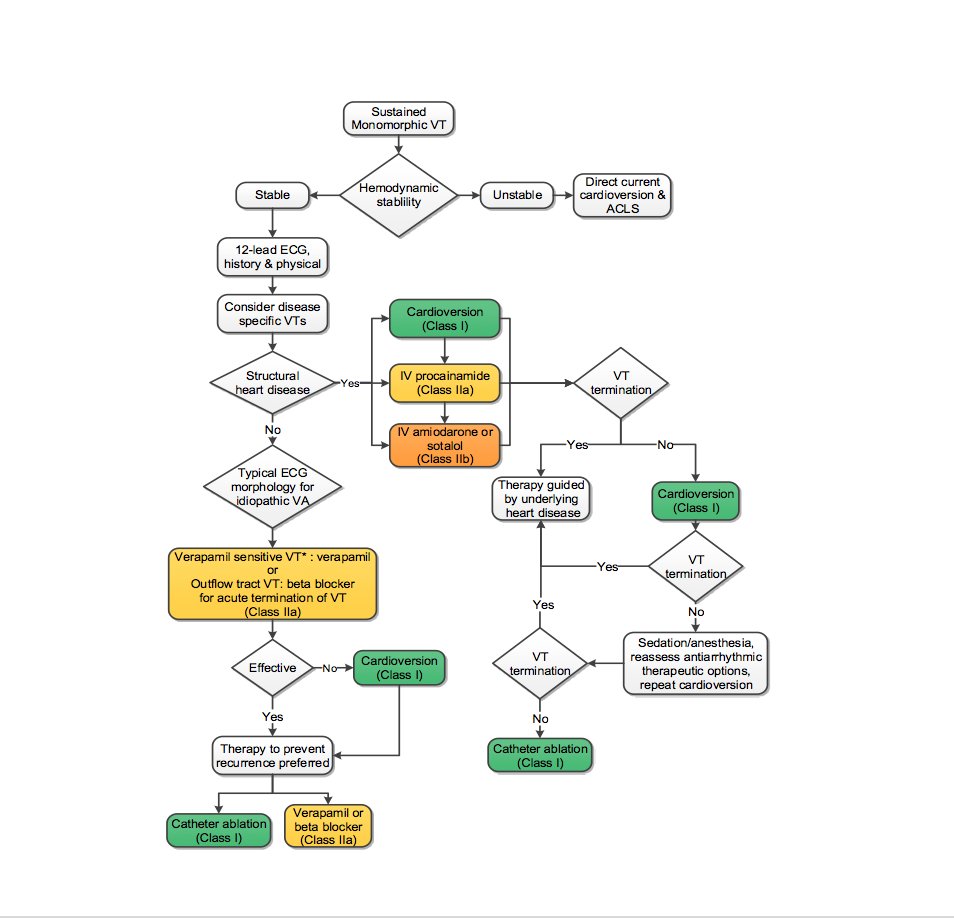
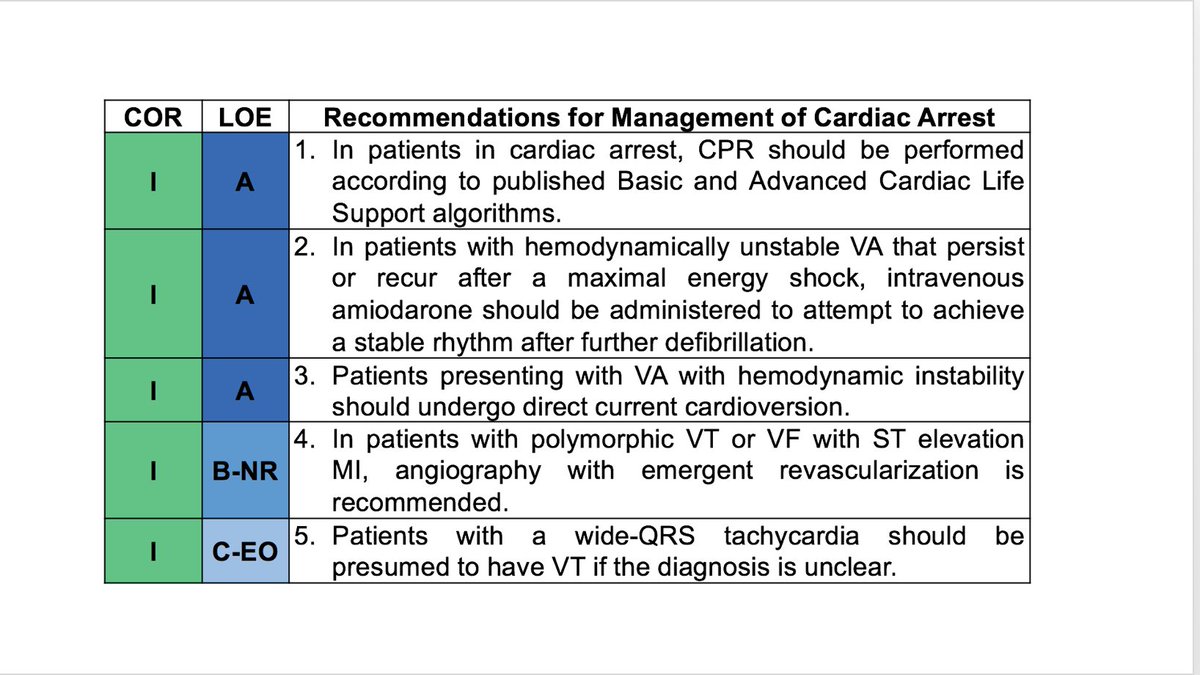
7/10 – Management of Monomorphic #VT
-Usually 2/2 reentry around scar
-Initial Tx – ACLS!
-Immediate cardioversion if unstable, or drugs don’t work!
-HD stable? Give amiodarone 150mg over 10 minutes followed by 1mg/min
-Evaluate underlying etiology!
8/10 – Long term #VT Tx:
-Assess SCD risk & ICD need
-Anti-arrhythmic Tx (amio, sotalol, mexiletine)
-Ablation in selected pts
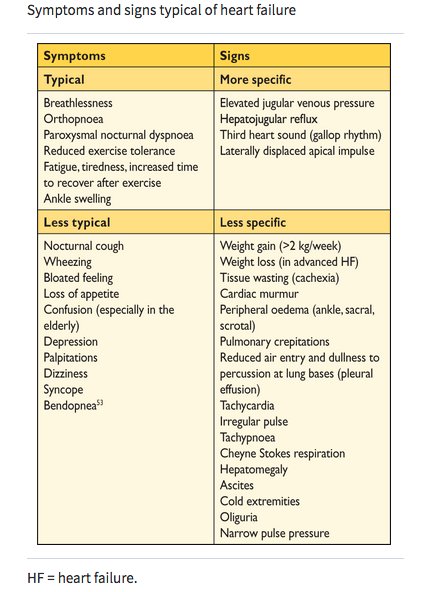
-HF therapy
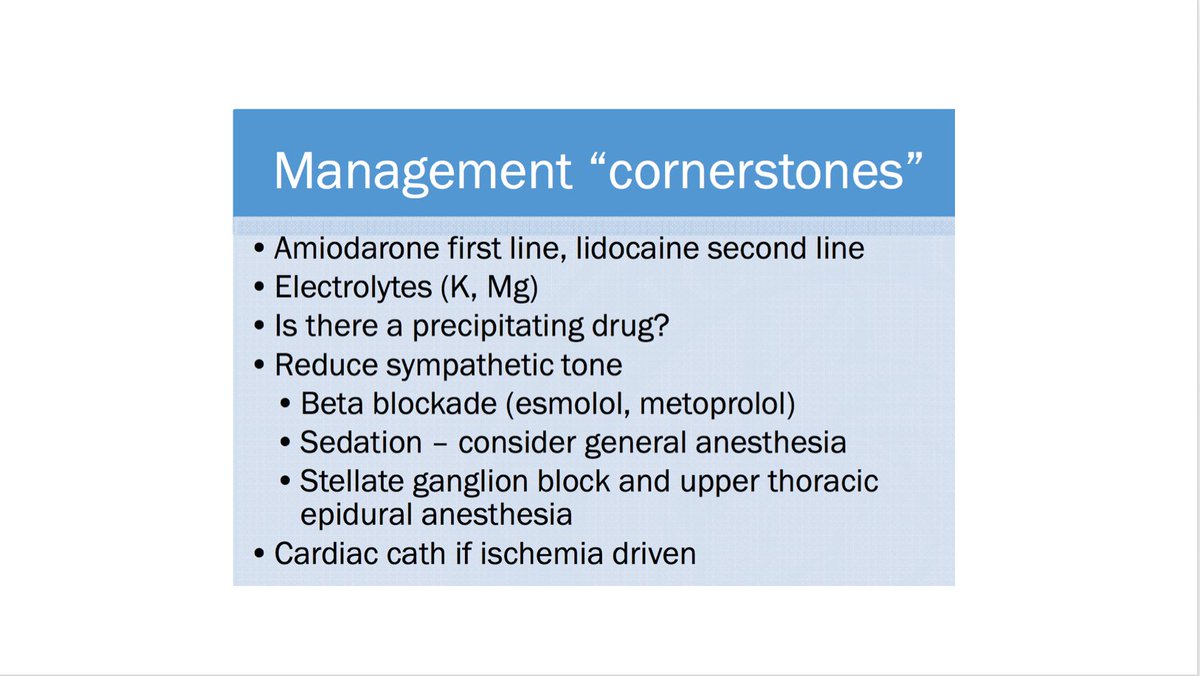
#VT Storm:
≥3 VT episodes/ 24 hrs
Can ☞ incessant state!
Tx - amio > lido, lytes, BB (see Tx “cornerstones”)
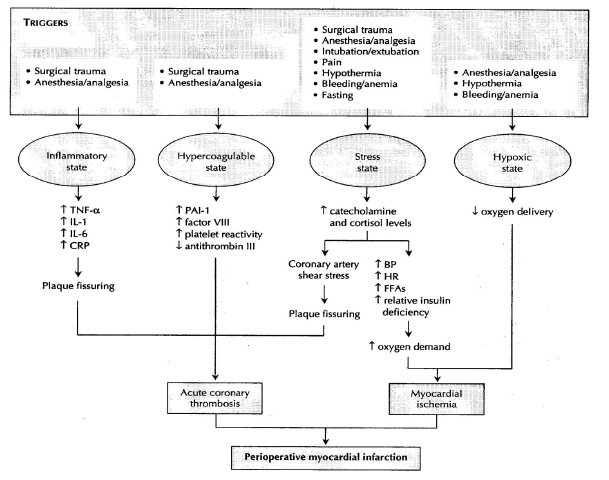
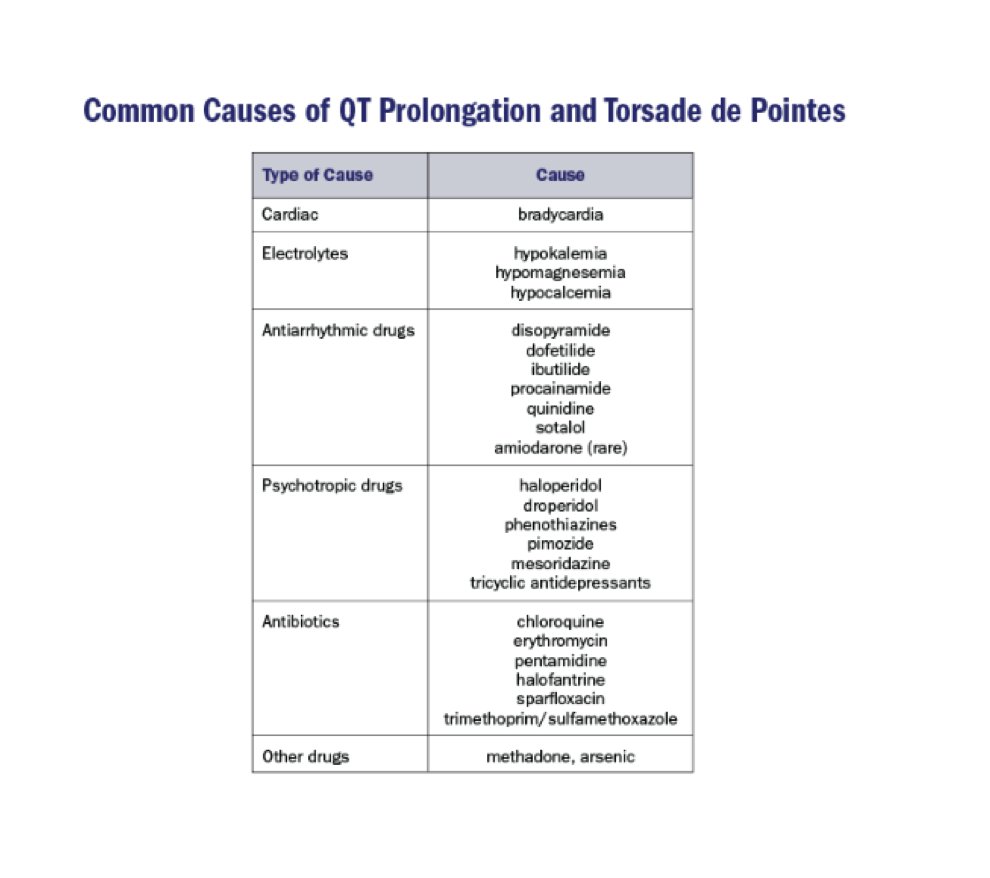
9/10 – Polymorphic VT/VF
Think ischemia!!!
#AMI ➡️ early cardiac cath!
Other precipitating causes: Drugs (QT prolonging -- see figure), electrolytes, decompensated HF
PVC may trigger polymorphic VT/VF; can be a target for ablation (see fig)
10/10 Summary
If HD unstable ⇧ HR ⇒ shock!
✔️ Narrow vs wide QRS & rhythm regularity ➡️narrow DDx
✔️ Brugada criteria to 👀 VT vs SVT. If underlying SHD, 90% it’s VT!
Follow Tx discussed
Now a few 💪 practice cases! Plz share your thoughts!