⚠️NOT "clearance"!
Purpose of consult
-Evaluate pt`s medical status
-Risk assessment
-Management recs
-Treat modifiable risk factors
-"Team" approach for shared decision making
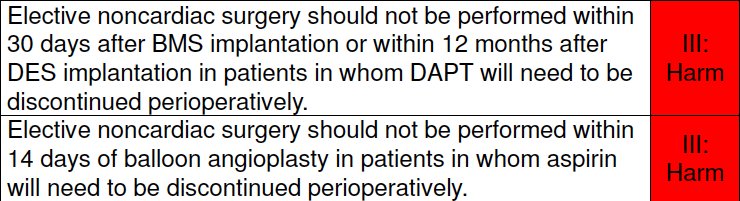
-Should pt have surgery? Emergent or not?
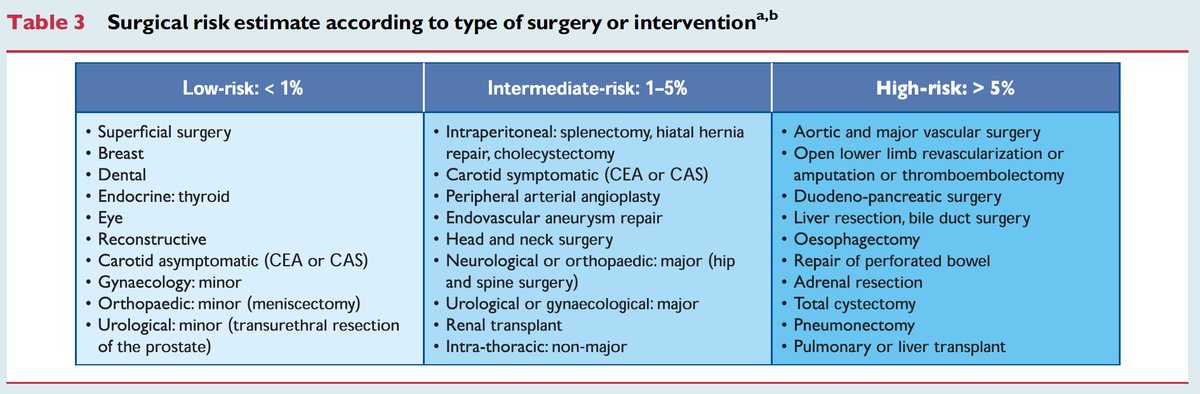
-Type of surgery and type of anesthesia?
-Functional status of the pt?
-Relevant medical hx and any ongoing cardiac sx?
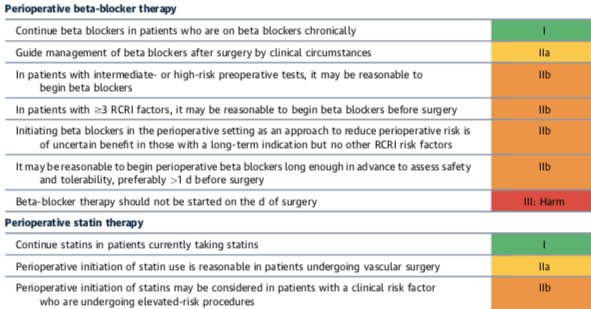
-Review the meds.
-Prior cardiac w/u.
Focus on good history and PE, can save a lot of tests & 💸
Very thorough and informative 📃.
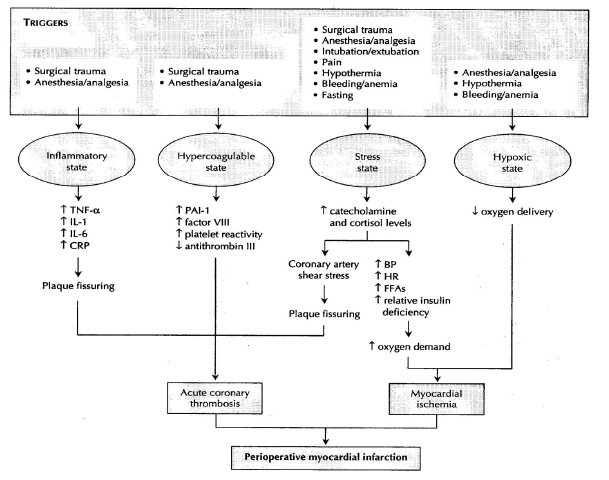
Assess pt`s clinical risk
💠ACC 2009- Low, medium or high risk.
💠ACC 2014 update- Low risk ( <1% risk of MACE) or elevated risk (>1% MACE)
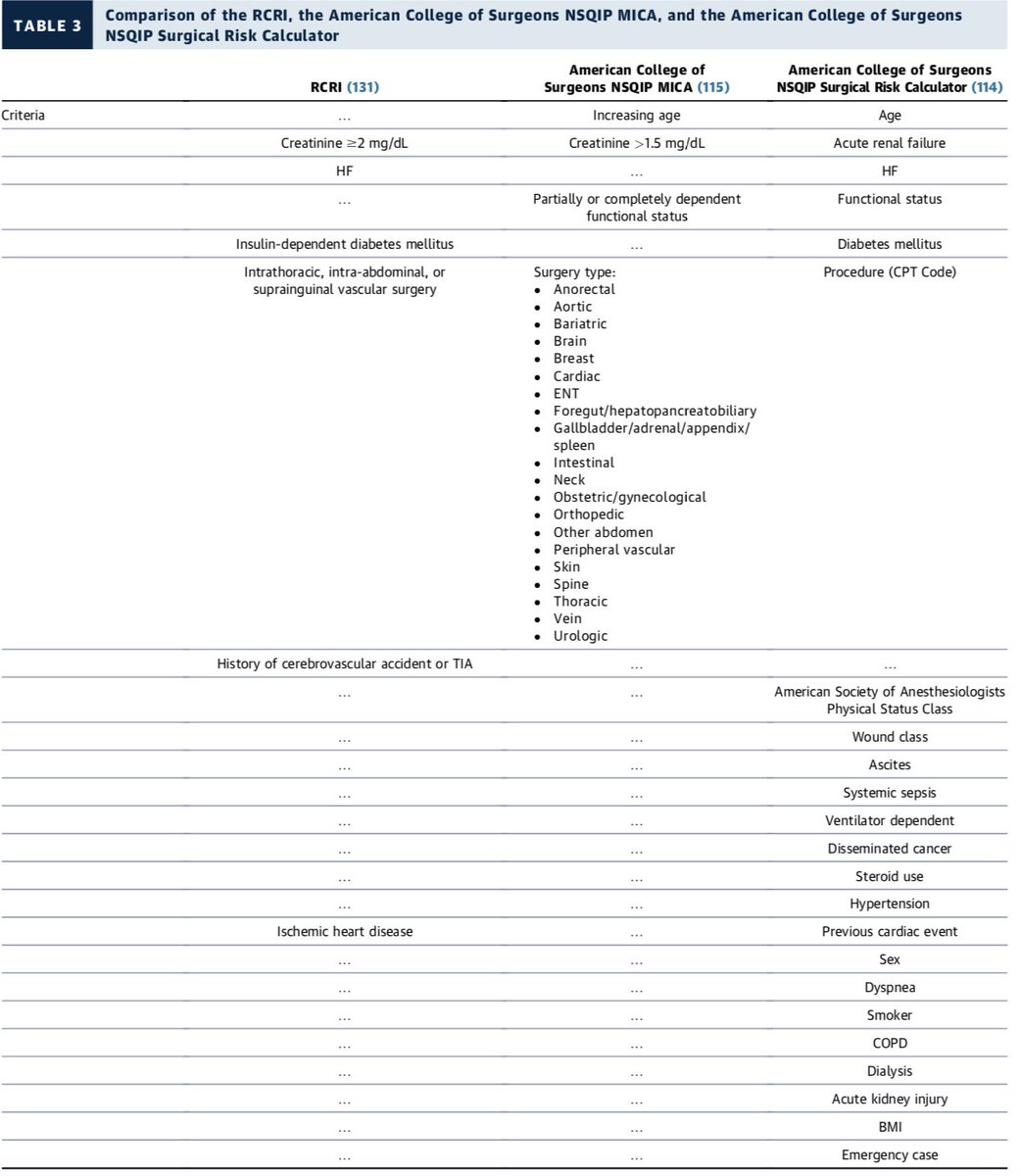
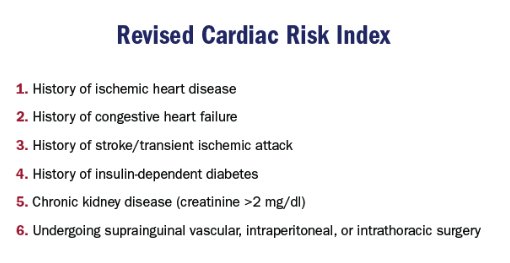
💠Revised Cardiac Risk Index (RCRI)-simple, widely accepted
• 0-1 low risk, >1 elevated risk
💠ACS NSQIP MICA
• (surgicalriskcalculator.com/miorcardiacarr…)
💠ACS NSQIP Surgical Risk Calculator
• (riskcalculator.facs.org)
⚠️Recent (<30 days) or active MI, unstable or severe.
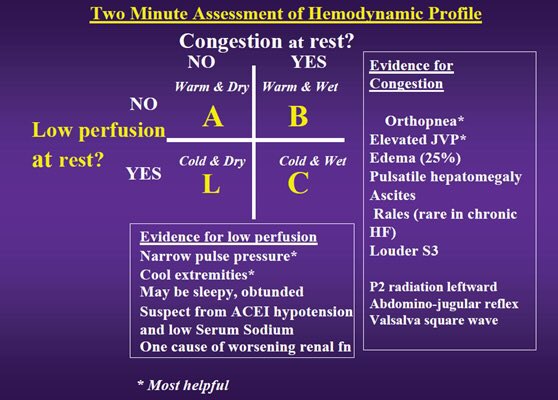
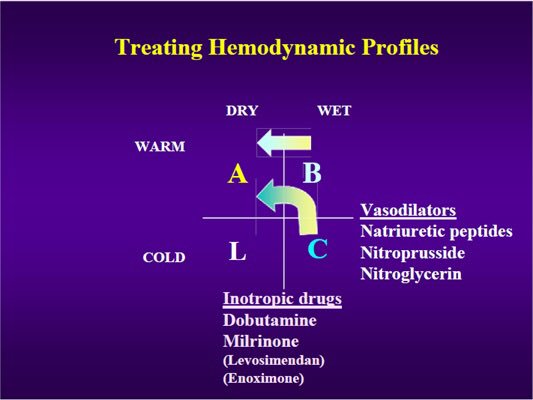
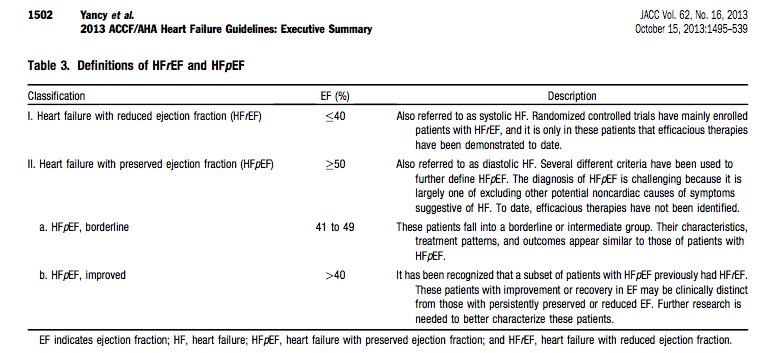
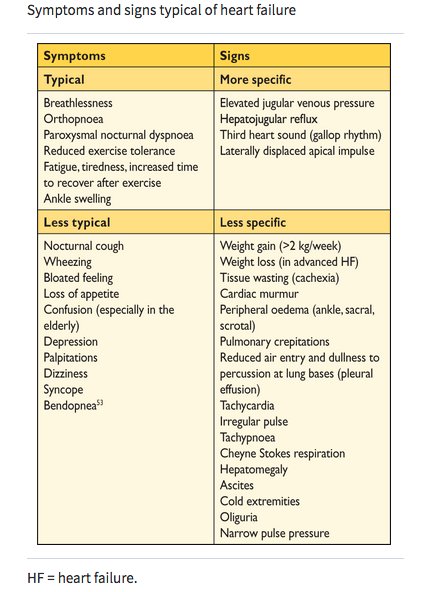
⚠️Acute decompensated HF
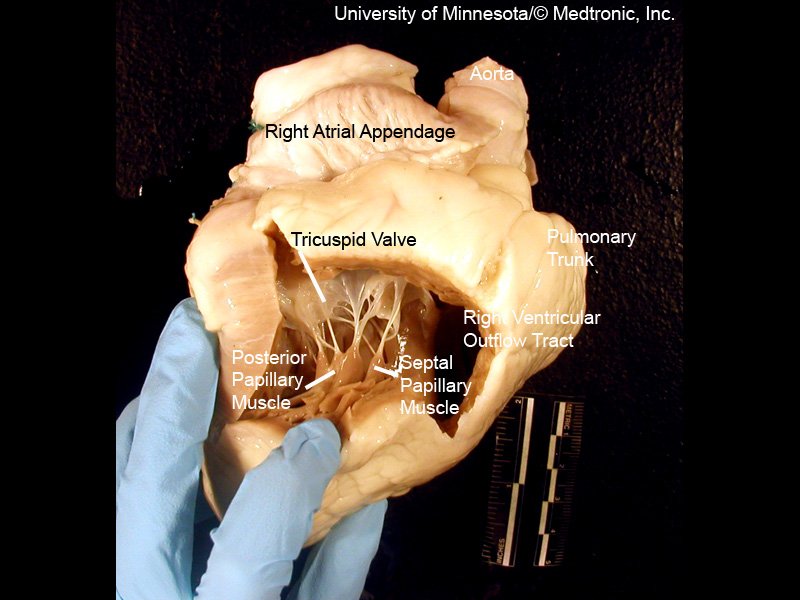
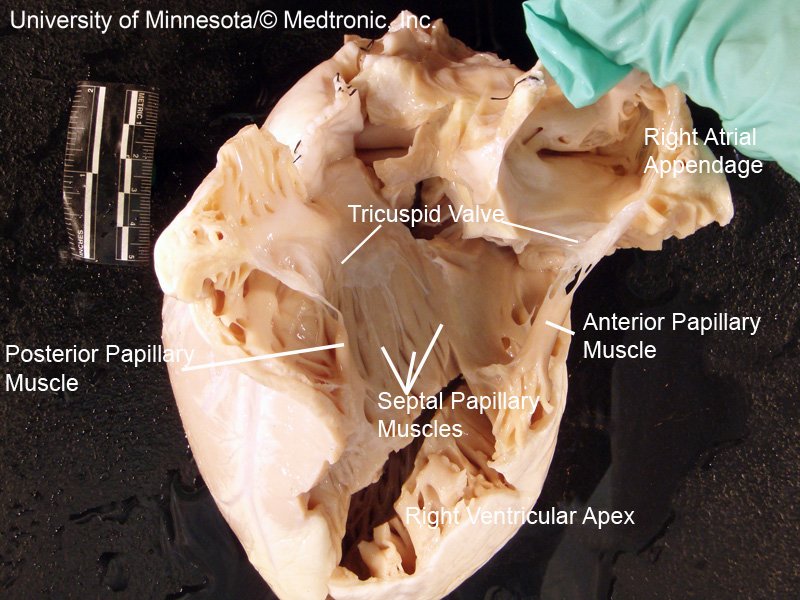
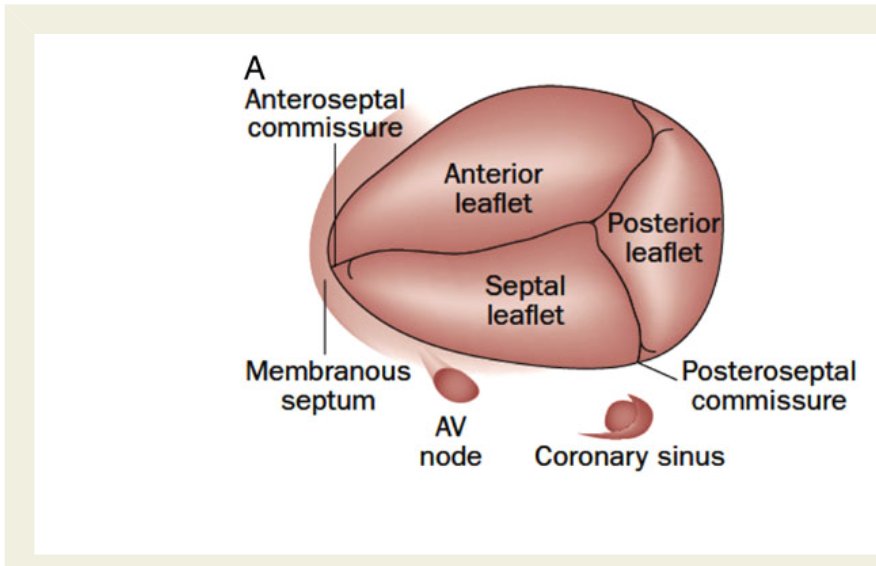
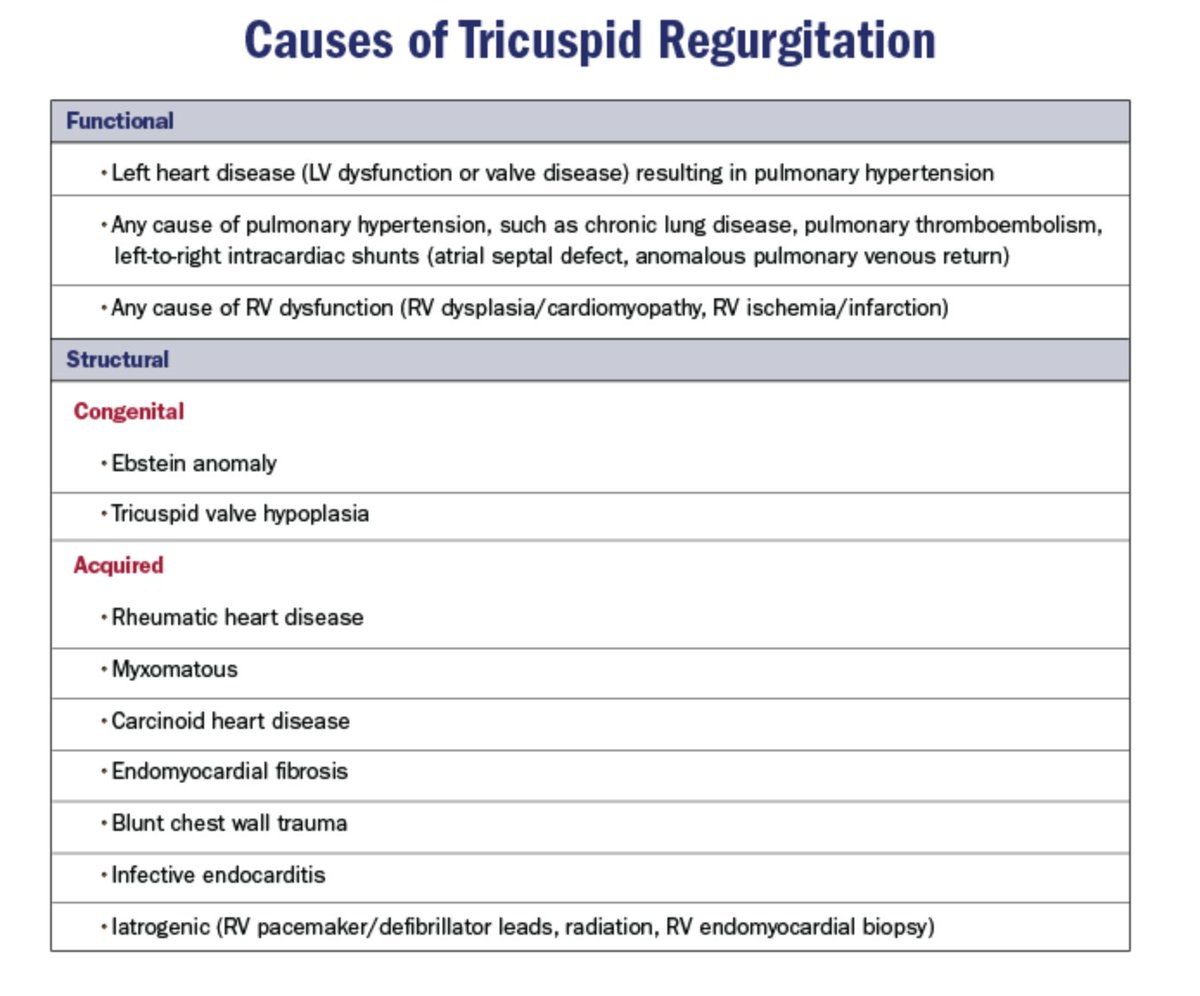
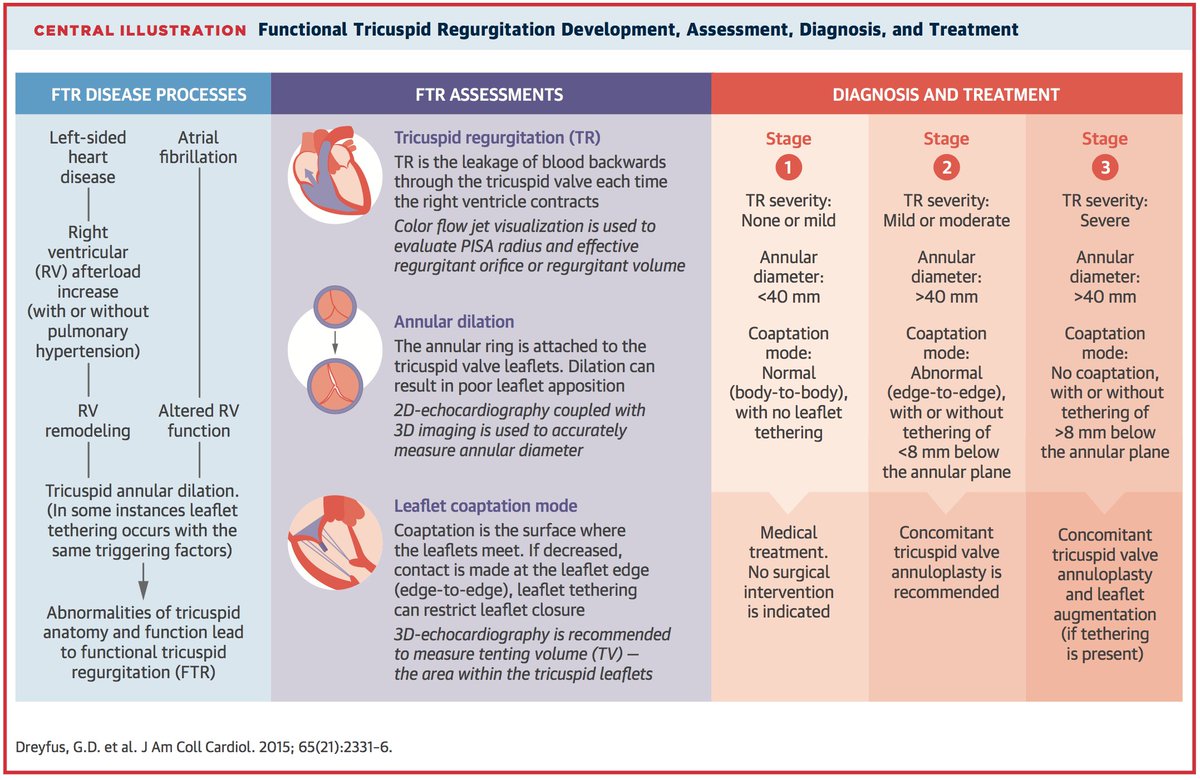
⚠️Severe symptomatic valvular disease
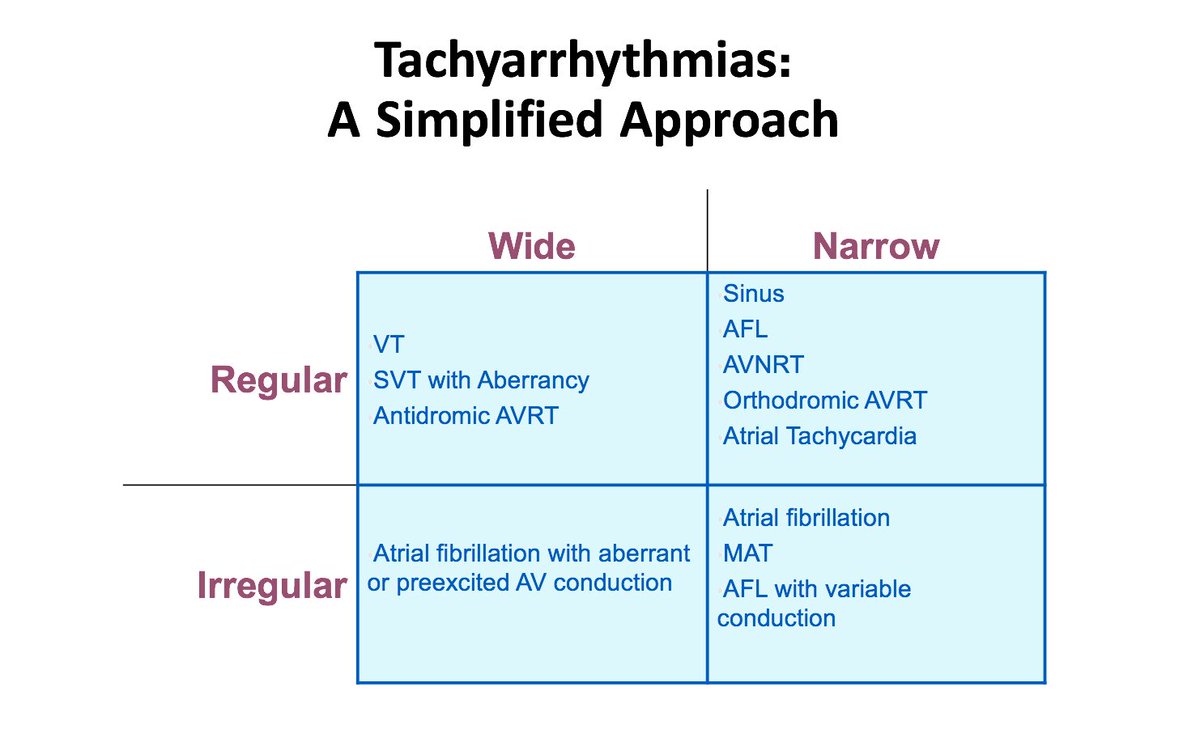
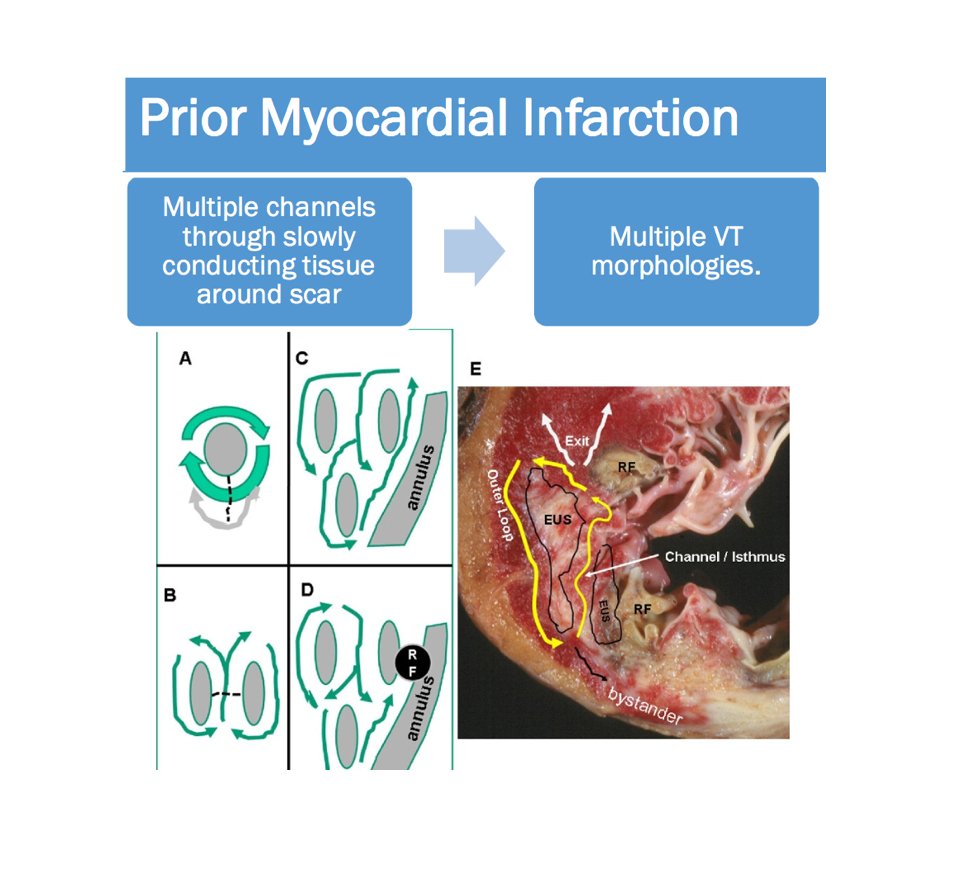
⚠️Significant arrhythmias (tachy/brady)
Consider delaying non-emergent surgery if present.
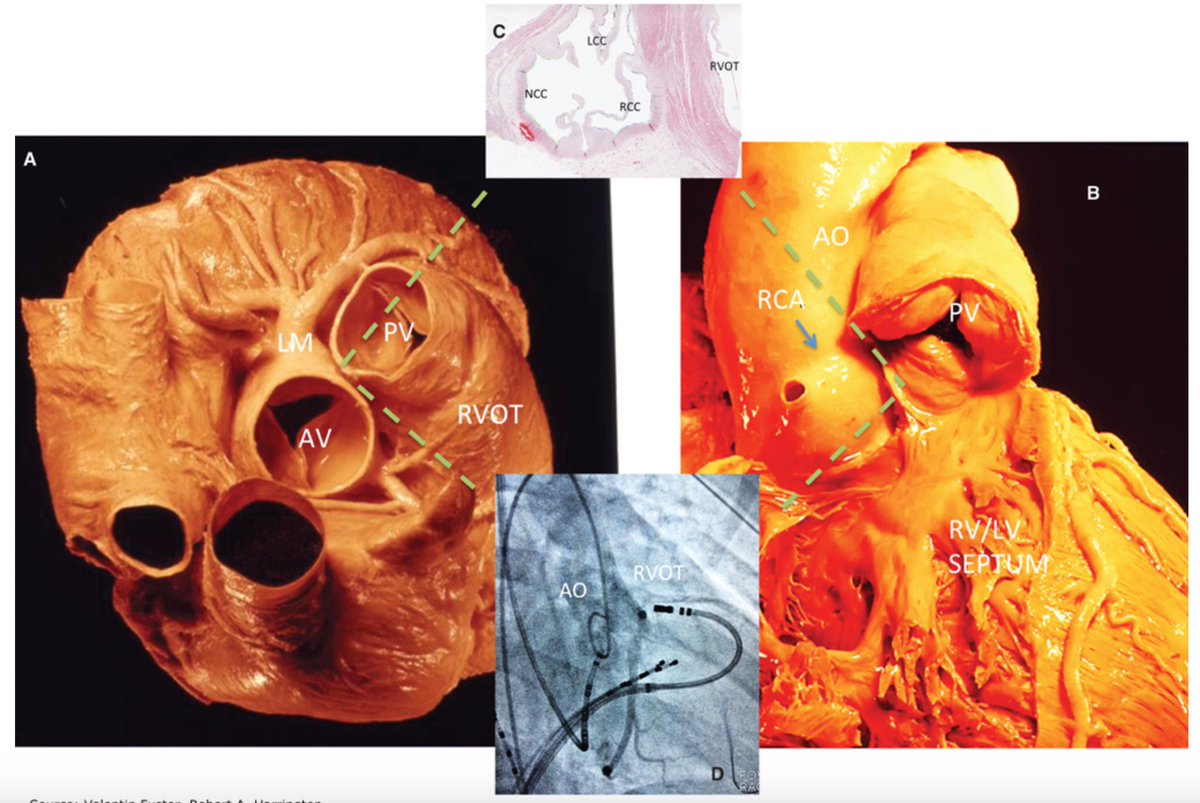
Symptomatic- Rx before elective surgery
💠Symptomatic AS -⬆️ periop mortality ~10%; Rx prior to surgery
💠Severe, asymptomatic AS-acceptable risk(avoid low preload)
💠Severe MV stenosis- avoid ⬆️HR
💠AR/MR-usually well tolerated
☑️Risk stratify, not “clear”
☑️Use “team” approach
☑️Use risk prediction 🛠️
☑️ Obtain good history and PE
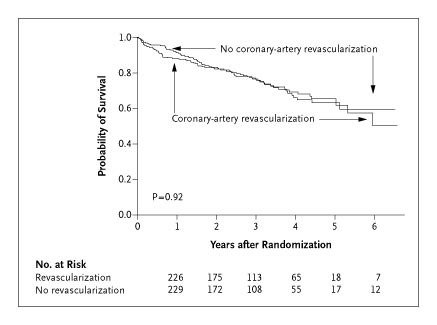
☑️Use additional testing cautiously; can delay the surgery
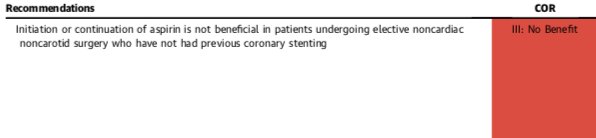
☑️Manage meds, anti-platelets and pts with recent PCI carefully
☑️Remember the “DONTs”