(1/12)
(2/2)
#COVID19 #VentilatorShortage
(3/12)
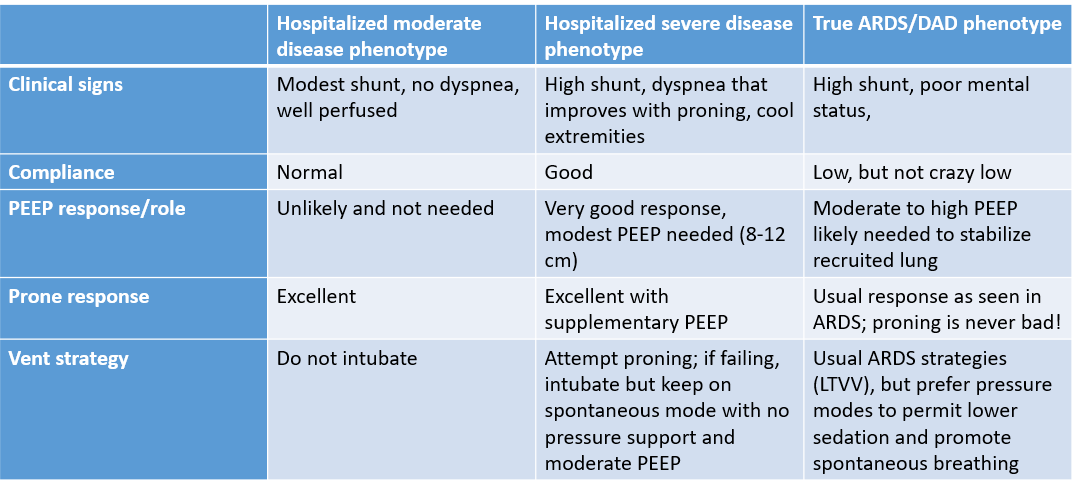
Even post-pandemic, I’m going to try awake prone on HHHFNC for all pts w/ hypoxemic RF & acceptable WOB. Amazing strategy
(4/12)
(5/12)
(6/12)
(7/12)
(8/12)
Always #ccecho findings predicted by physical findings & context. Did not change mgmt.
Really doubt lung #POCUS has much role in ICU #COVID19 pts & would not #echofirst
(9/12)
Differences in outcomes for pts will ultimately be related to adequacy & quality of RN care, RT, #rapidresponse systems, not medications, # of vents, etc
(10/12)
I cannot imagine struggles of families in these times, probably very difficult to trust #healthcare team when you can't see it firsthand
Expect a big #ICU #burnout wave post #COVID19
(12/12)


