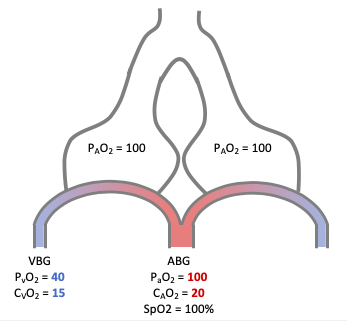
1/
2/
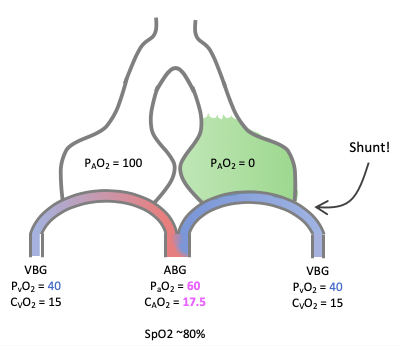
7/
➡️liebertpub.com/doi/full/10.10…
8/
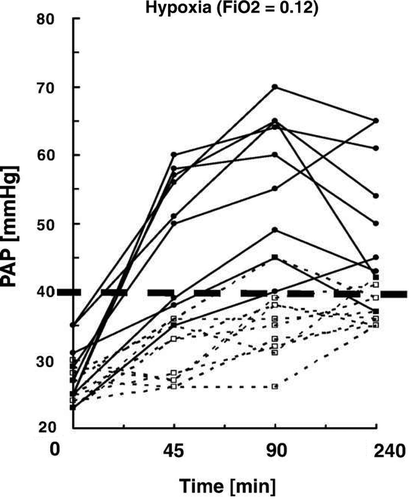
9/
thorax.bmj.com/content/63/Sup…
11/
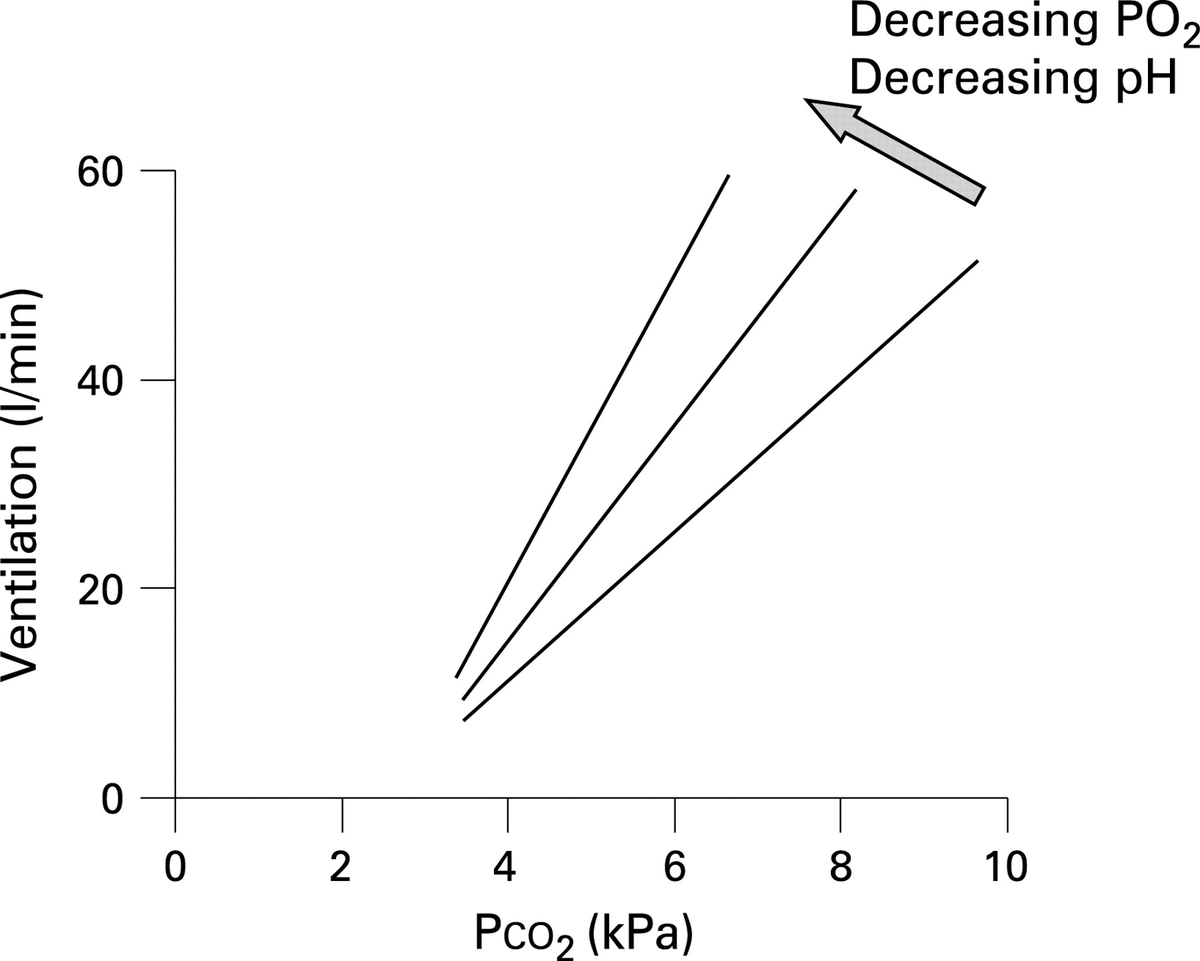
12/
➡️bit.ly/3dYo2Xn
* HPV determines how much shunt we get when we have a patchy pulmonary process. This varies widely from person to person.
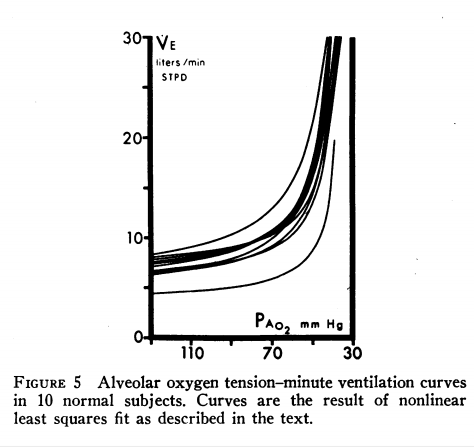
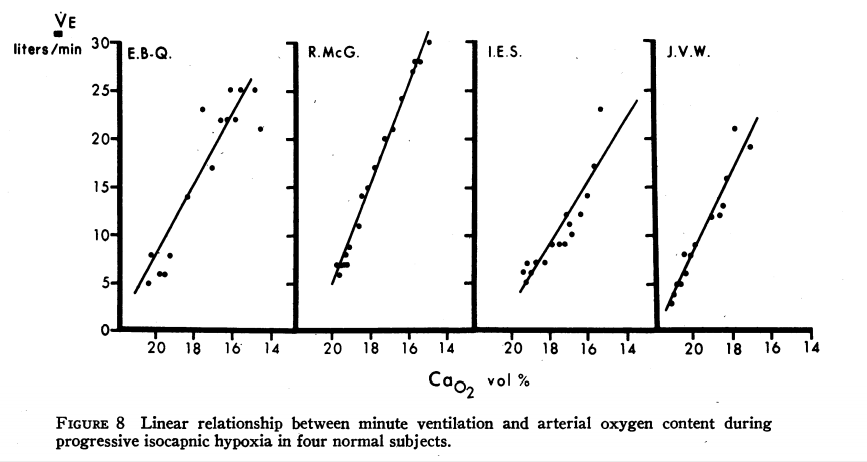
* HVD determines how much shortness of breath we feel and how much we increase our ventilation w/ hypoxia. This also varies a lot.
12/
fin/