How common is loss of smell (anosmia) in #SARSCoV2 #COVID19, and how useful is it for ruling the diagnosis in or out? Let’s take a look at the data.
Here’s a quick #HowIReadThisPaper on two @AnnalsofEM papers addressing this question:
Chua et al
&
Peyroney et al
(Thread)
First, a question:
Let’s assume you have a limited supply of swabs and need to prioritize which patients to test for COVID19.
In which skilled nursing facility (SNF) setting would you expect anosmia to be more useful in identifying patients who will test positive?
Chua et al annemergmed.com/article/S0196-…
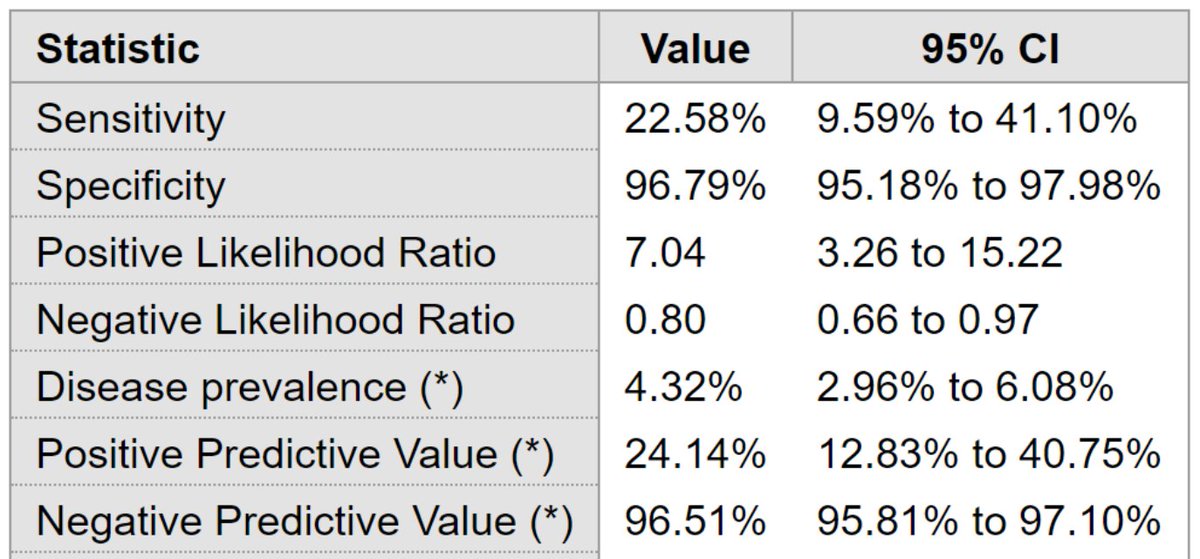
Question: What are the test characteristics of acute olfactory loss (hyposmia or anosmia for <14d) for Dx of COVID19, using oropharyngeal PCR as the gold standard?
Design: single-center cross-sectional study via chart review (retrospective)
Population: 717 patients presenting to a single ED in Singapore from 3/23/2020 - 4/4/2020
Procedures: All patients tested for COVID-19 via OP swab (those with respiratory symptoms or recent travel) were also asked about hyposmia & anosmia from 3/23/3030 onward.
Author's conclusions: among patients presenting to the ED with respiratory symptoms, hyposmia and anosmia are highly specific (but not at all sensitive) for the diagnosis of COVID-19. PPV was low, but NPV was high.
How should we use these results?
A few thoughts:
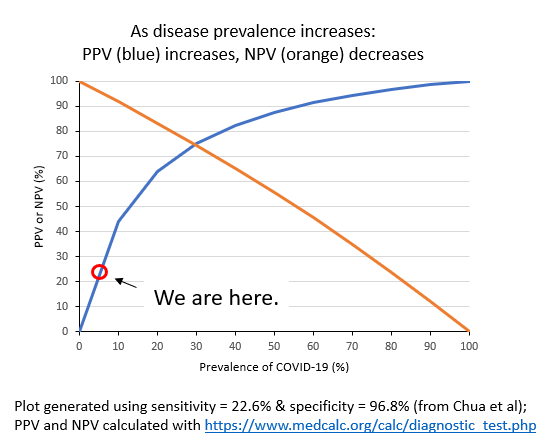
You can see why this is bad. A PPV of <50% means that more than half of people with acute olfactory loss will test negative for COVID19!
But – what about the specificity of 96.8%, doesn’t that mean anosmia should be useful for ruling in COVID19?
Yes, but at the cost of many false positives when the disease is rare.
Therefore, acute olfactory loss is not really useful when disease prevalence is low.
What about when disease prevalence is high? Let’s take a look at the second paper to find out.
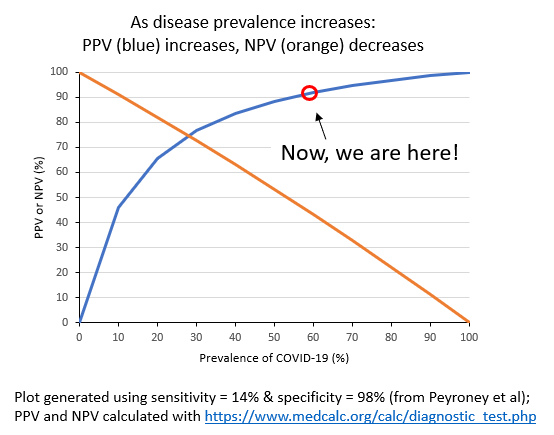
Peyrony et al annemergmed.com/article/S0196-…
Question: What are the test characteristics of anosmia (among other things) for diagnosis of COVID19, using nasal PCR as the gold standard?
Design: single-center prospective cohort study
Population: 391 patients presenting to a single ED in France from 3/9/2020 - 4/4/2020
Procedures: Testing (via nasal swab) was clinically driven; dyspneic, older, and sicker patients were more likely to be tested. Patients were only asked about anosmia from 3/24/3030 onward.
Revisiting the original question:
Assuming you have a limited supply of swabs and need to prioritize who to test for COVID19:
In which skilled nursing facility (SNF) setting would you expect anosmia to be more useful in identifying patients who will test positive?
Bottom line: At low prevalence of COVID19, the PPV of acute olfactory loss (anosmia) is also low: more false positives than true positives are likely below a prevalence of 10-15%.
As prevalence ↑, the PPV of anosmia also ↑: at a prevalence of ~60%, the PPV is >90%.
(End)