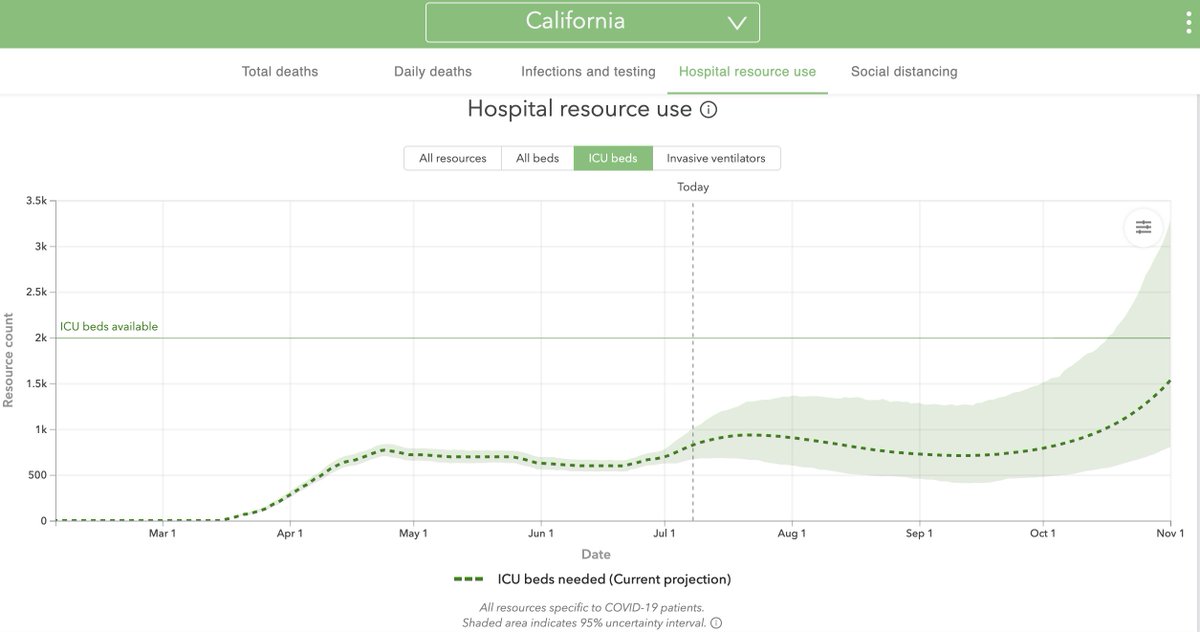
Buckle up for a #tweetorial about ICU capacity and what it means in the context of #COVID19.
1/




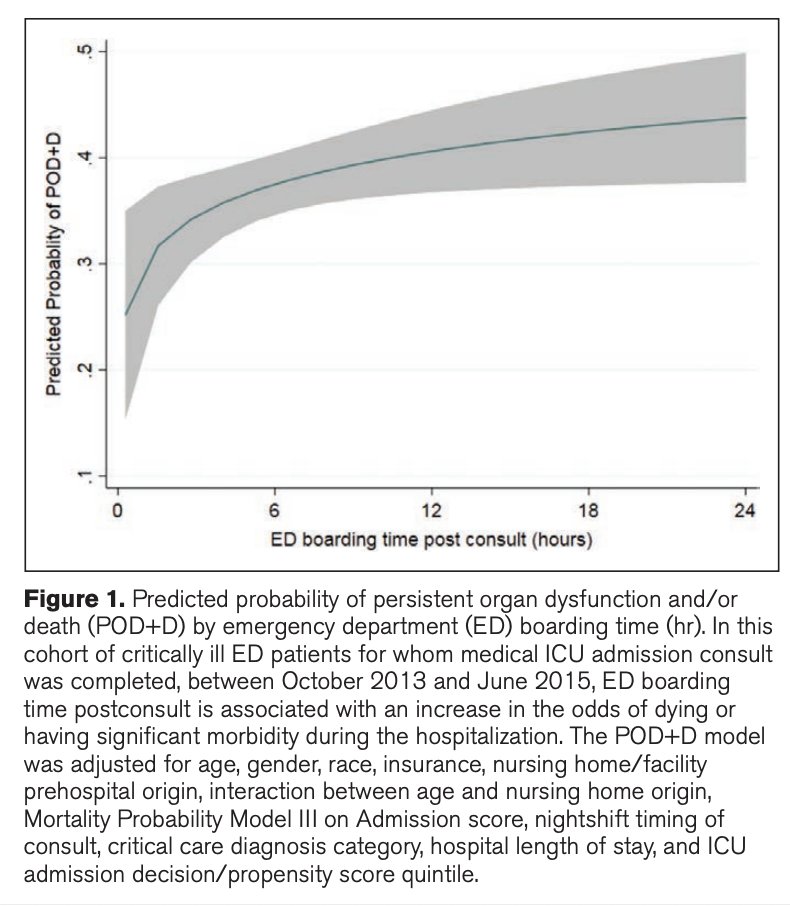
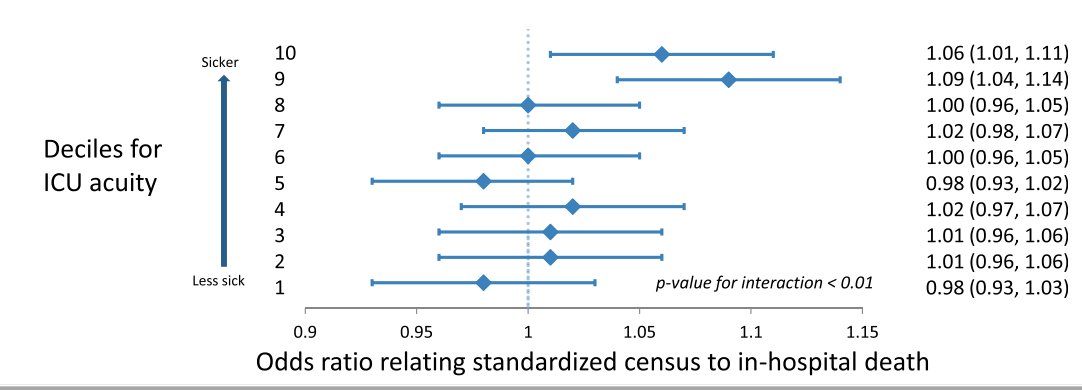
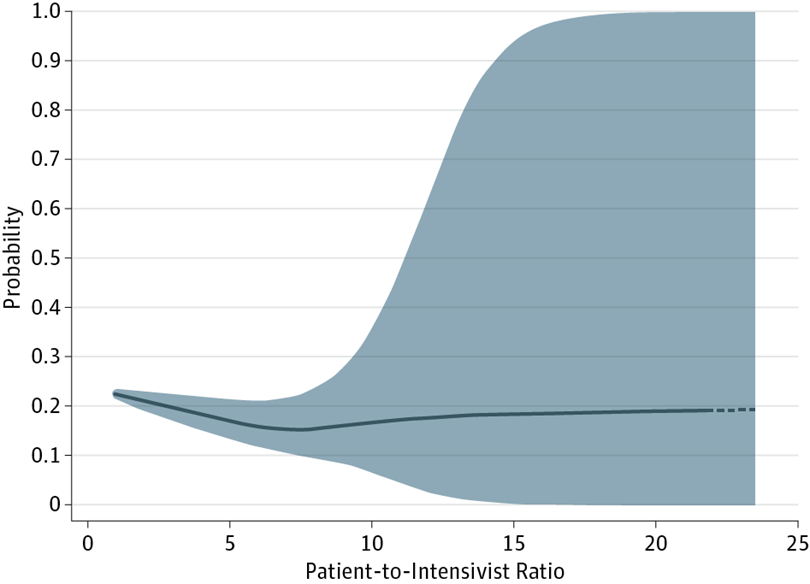
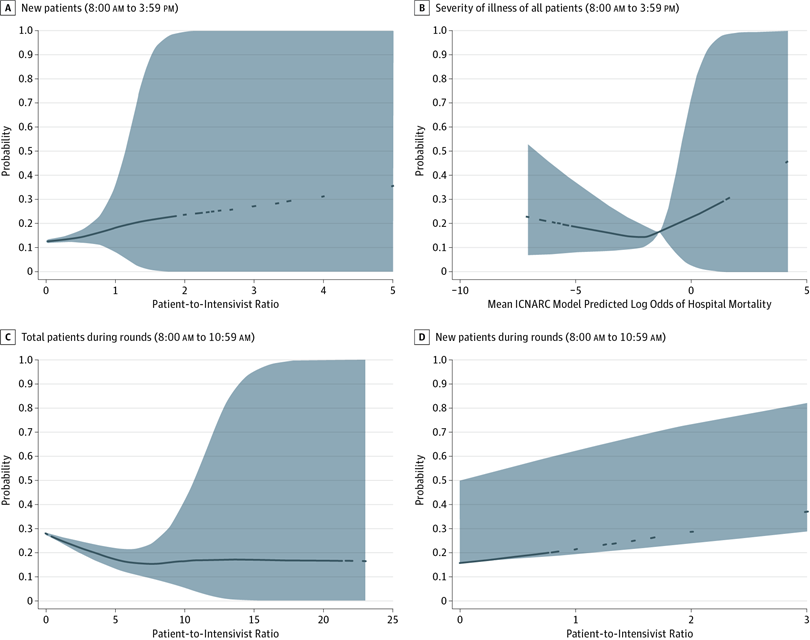
There is evidence that higher ICU census is associated with worse outcomes:
3/
➡️atsjournals.org/doi/pdf/10.116…
4/
➡️jamanetwork.com/journals/jamai…
5/
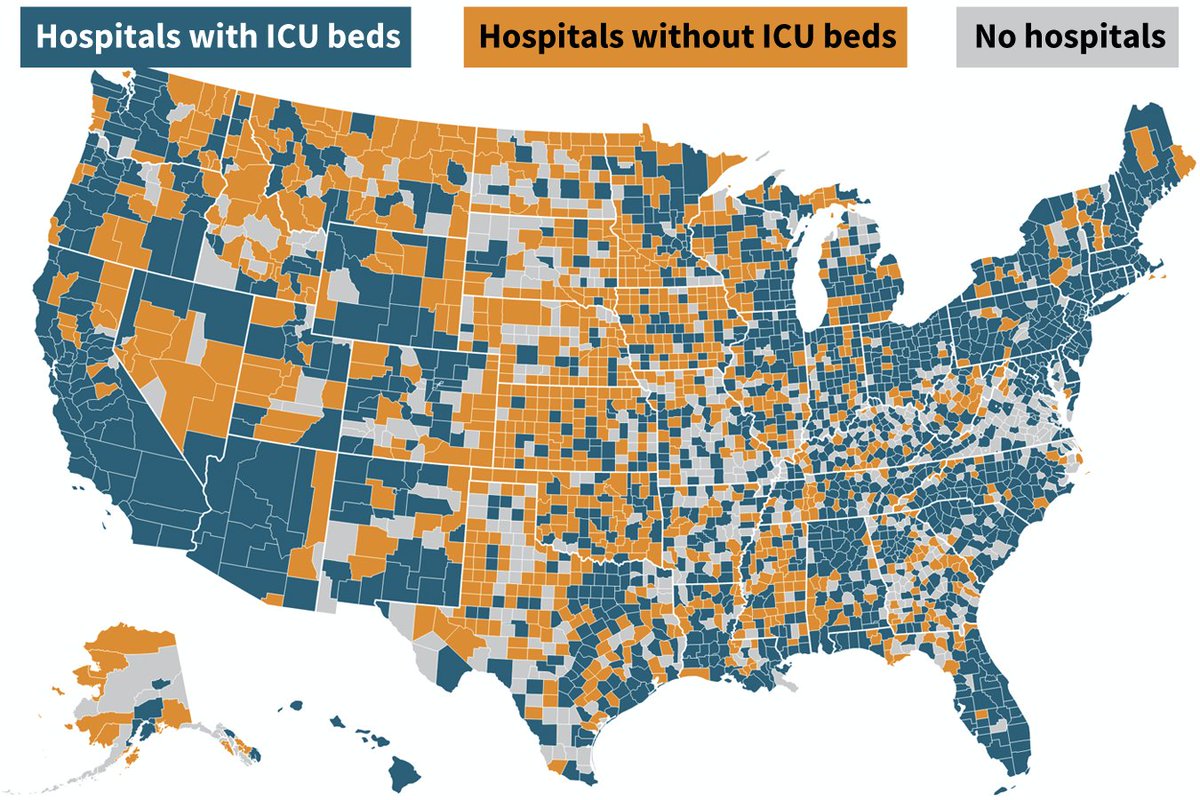
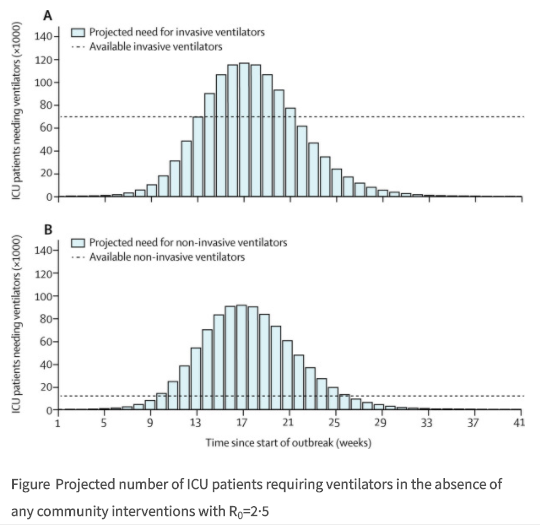
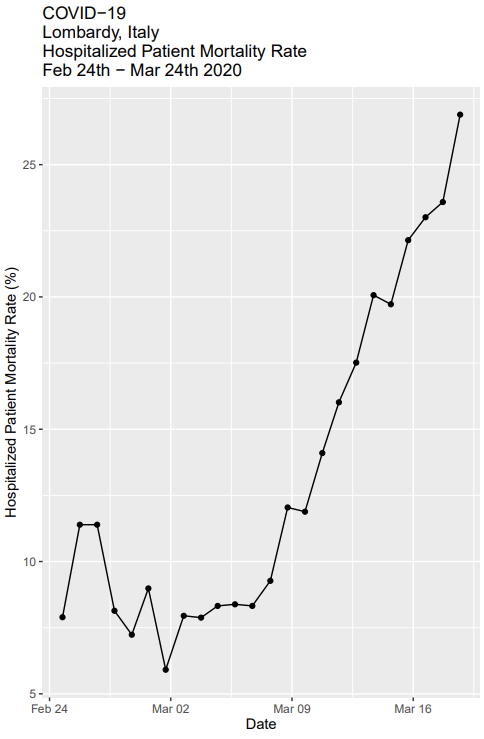
When there aren’t enough beds, some people who need ICU interventions (ventilators, vasopressors, dialysis) don’t get them, as in Italy:
6/
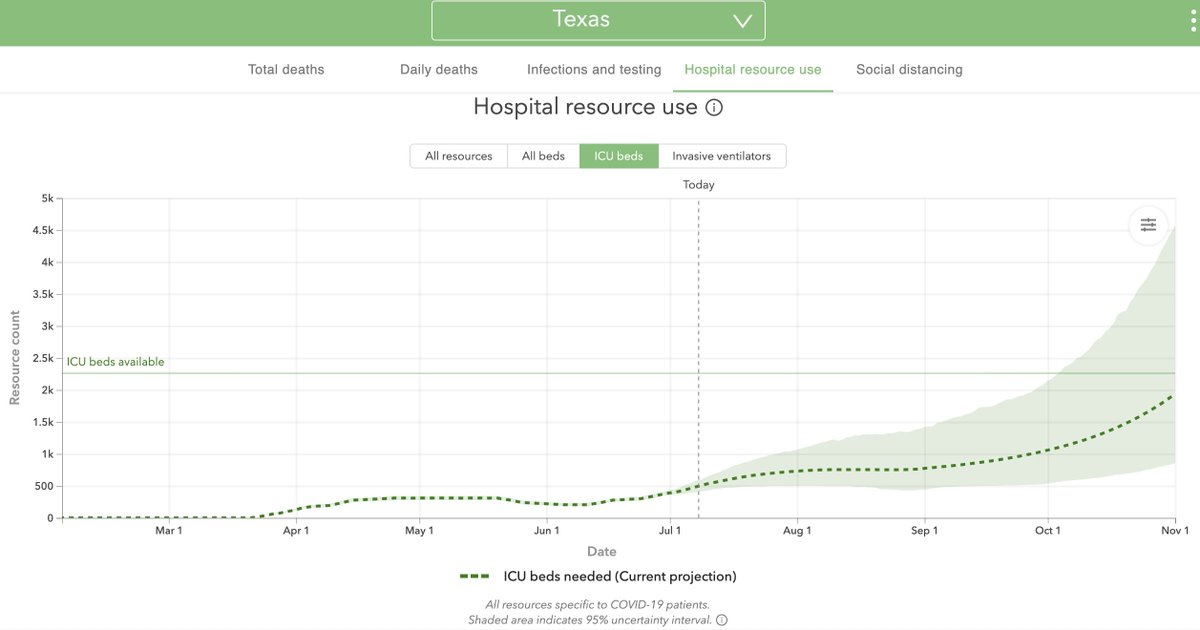
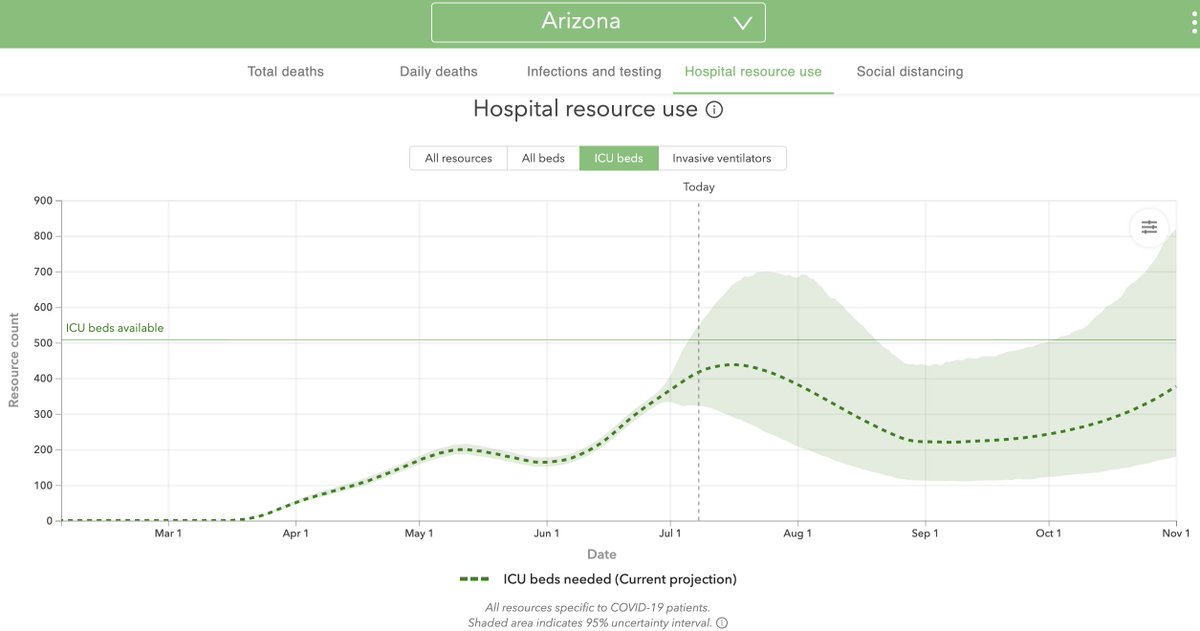
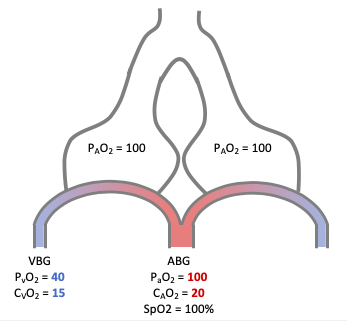
From the perspective of ICU strain, acuity, & Patient:Intensivist ratio (PIR), COVID-19 is the perfect storm.
8/
This is not the case with COVID19.
9/
➡️medrxiv.org/content/10.110…
10/
- Not all have negative pressure rooms.
- Not all have connections to run dialysis machines.
- Not all are accustomed to caring for patients with severe ARDS from COVID & only some are familiar with ECMO, proning, etc.
13/
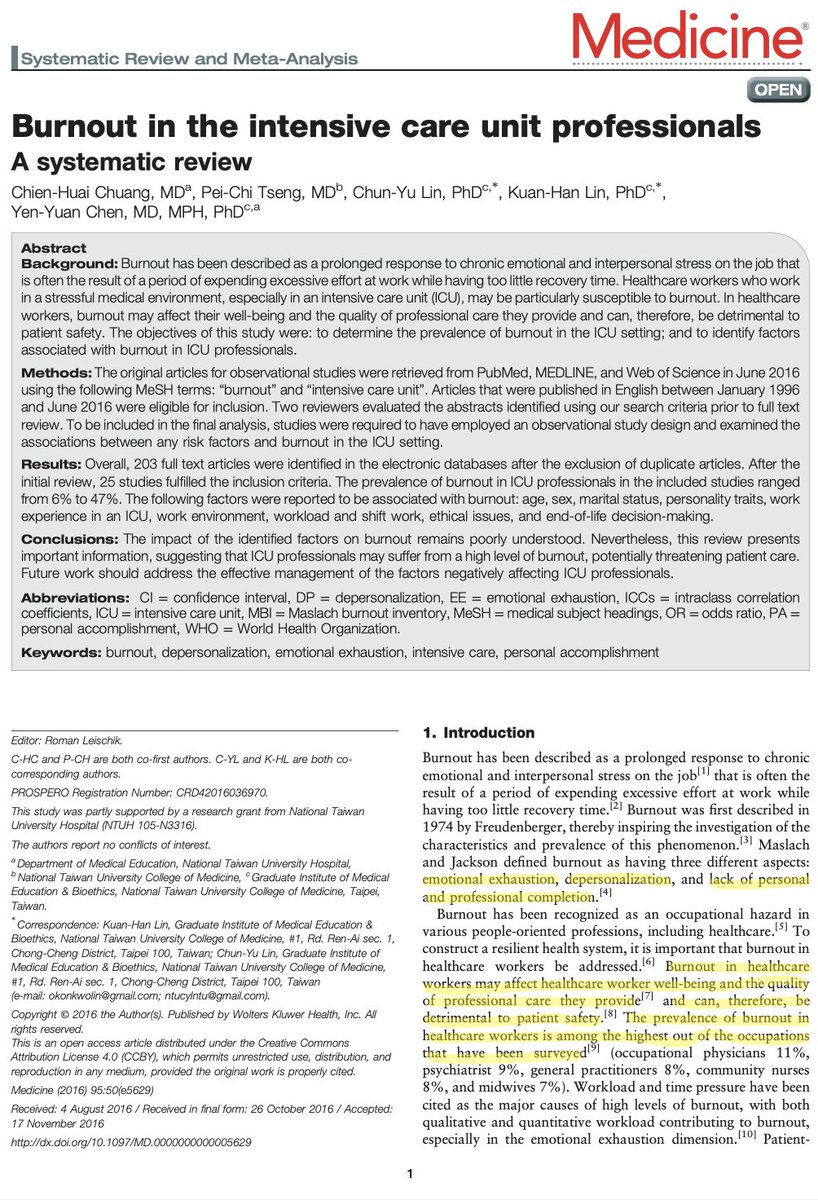
Critical care is less about specialized machines & more about highly trained professionals who can care for sick patients. You can ‘uplevel’ a step-down unit but you can’t easily create more CCRNs, RTs, pharmacists, etc.
14/
Prior to COVID there was a national shortage of ICU RNs: of the 3.3m RNs in the US, just 290k (~15%) are critical care RNs. This includes adult, peds, & neonatal.
COVID has exacerbated the shortage.
➡️healthaffairs.org/do/10.1377/hbl…
15/
ICU staffing flexes to match these changes. Short term holes can be filled with overtime, but this model can't work for months on end.
If ICUs are full for weeks, we will have major staffing shortages.
16/
Despite widespread underreporting, as of May >60,000 US HCPs had been infected.
In NYC, serological testing revealed that 12% of HCWs had antibodies against SARS-CoV-2.
17/
npr.org/sections/healt…
Despite 6 more months to prepare, there are worrisome signs that this new surge could once again make PPE scarce.
18/
washingtonpost.com/health/2020/07…
I’ve been worried about this since the early days of the pandemic:
20/
* limit further spread of the coronavirus #stayhome #WashYourHands #WearAMask
* bring trained staff, such as civilian volunteers or military medical teams, to the hardest hit hospitals,
* keep staff safe & healthy #GetUsPPE