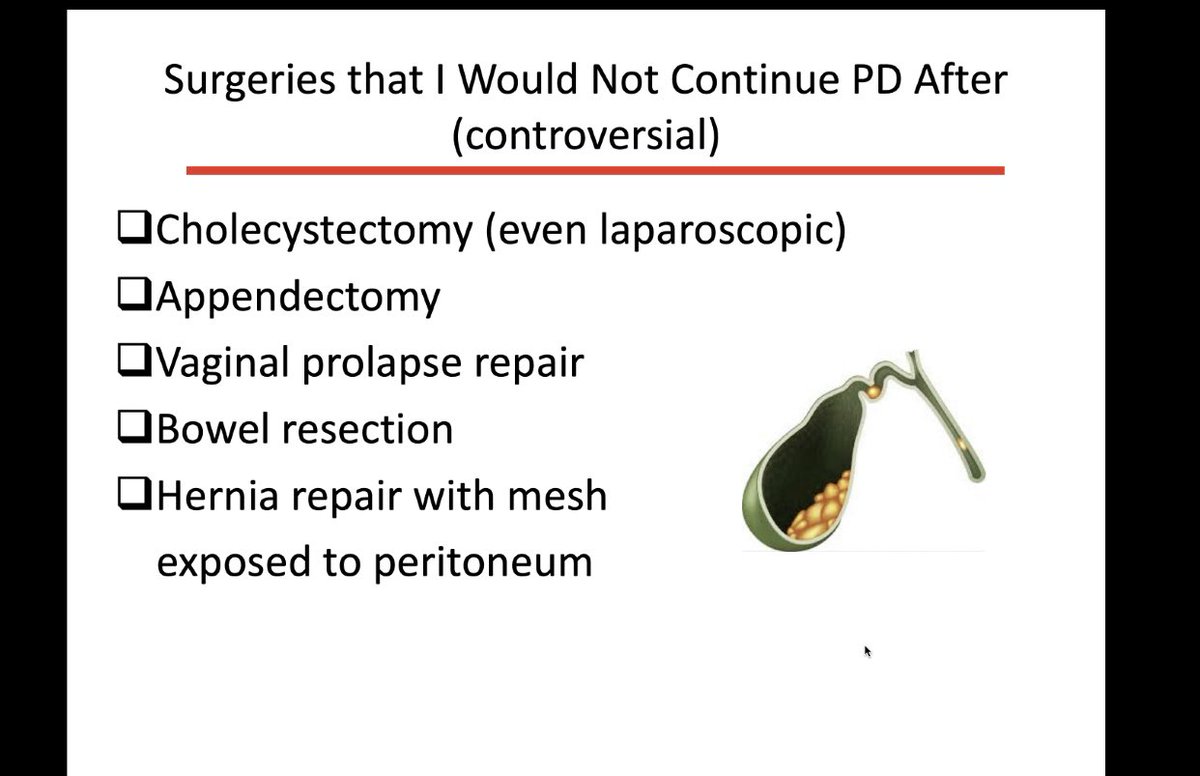
Depends – personally I always try and continue with PD post-surgery where it’s safe to do so ..
• Glucose is not good for the PD membrane
• What is the point – will end up on HD anyway
• They have kids
• They have a dog /cat/snake etc...
• They have an LRD in the pipeline
• They may get ESP...