Listen now! #Blooducation Graphic Medicine @Pathologists virtual lecture with @KreuterMD
learn.cap.org/lms/activity_o…
learn.cap.org/lms/activity_o…

Important to know how to approach a #DonorLookBack which is a multistep process a blood establishment must complete as a response to a donor who is newly reactive for an infectious disease test. Check out @bloodbankguy for more information 👆🏼👉🏼 bbguy.org/education/glos… 

Look up the relevant laws of blood transfusion check out the Code of Federal Regulations --> Title 21 --> 600 series👉🏼
accessdata.fda.gov/scripts/cdrh/c…
accessdata.fda.gov/scripts/cdrh/c…

HIV and HepC positivity in #DonorLookBack are codified and written in federal law (#CodeofFederalRegulations) which provide timelines of identifying and handling products as well as notifying transfused individuals. 

Whereas a #marketwithdrawal is when a donor forgets to disclose info requiring further action, NOT due to the error in blood collection following FDA guidelines. An example would be a person who forgot to disclose a pertinent travel history ✈️aabb.org/tm/questionnai… 

Next part was a discussion about working through RBC antibody panels! @KreuterMD shared how as a resident working through them caused "panel anxiety" 😲
Me too! 🪜But a step-by-step approach is key. Always ask yourself, "What is the next step?"
Me too! 🪜But a step-by-step approach is key. Always ask yourself, "What is the next step?"

Like our counterpart in anatomic pathology, it's all about #PatternRecognition. For more information on how to approach an antibody panel, watch this awesome @bloodbankguy video 🅰️🅱️🆎🅾️👉🏼bbguy.org/education/vide… 

Next was a neonatal #Blooducation topic: Neontal Alloimmune Thrombocytopenia. Similar to HDFN, this is when antibodies to PLTs cross the placenta and bind to fetal platelets causes neonatal thrombocytopenia. 

Important 🔦👶🏼👶🏾points to remember about NAT:
1. ) IgG antibody crosses the placenta and is actively transported to provide passive immunity to the baby
2.) Unlike HDFN, NAT can affect first born babies.
1. ) IgG antibody crosses the placenta and is actively transported to provide passive immunity to the baby
2.) Unlike HDFN, NAT can affect first born babies.
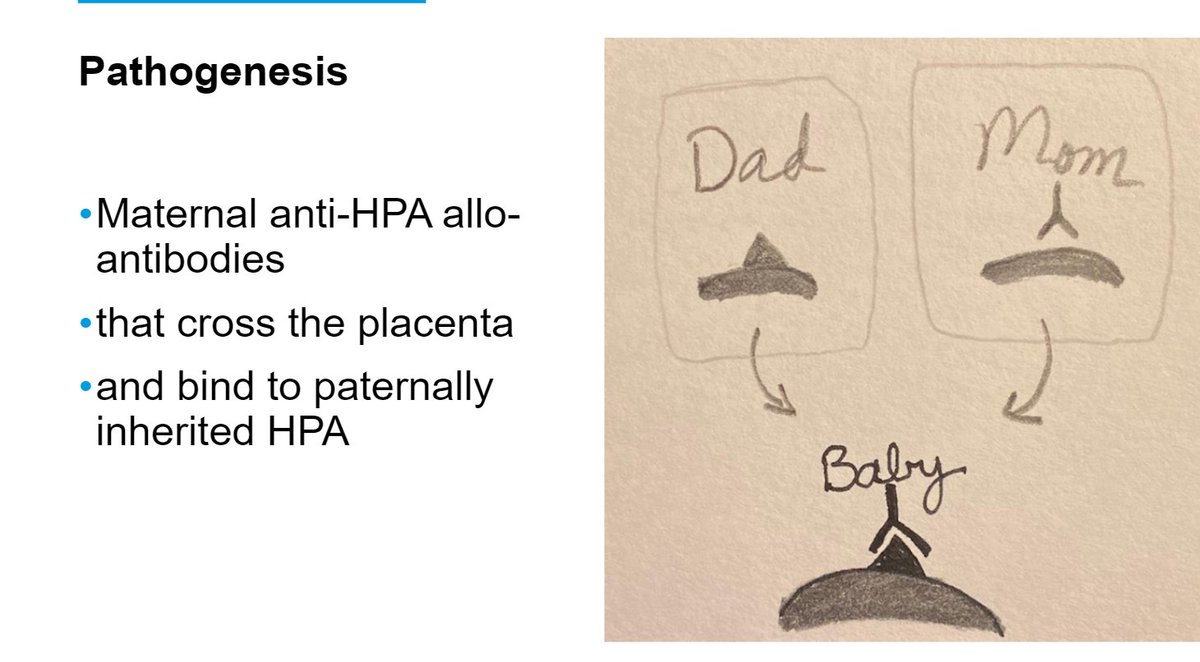
🔍PLT HPA Ags are located on the platelet surface & are are LARGE glycoproteins. They normally serve a functional role in coagulation. These antigens can have point mutations. NAT occurs when a 🤰🏾mother (homozygous for HPA1b antigen) makes Abs against the HPA1a antigens. 

🧐The choice of platelet transfusion really depends on the clinical context. For instance, if NAT is suspected and planned C-section is possible, then collecting the mother's antigen negative platelet (washed and irradiated) would be appropriate. @ash_bo21 

Big bleeds is another important area within #TransfusionMedicine, and understanding the historical trials that provide us with our key concepts in #traumarescucitation is important.

https://twitter.com/HermelinMD/status/1169089671634329601?s=20

Two major trials (jamanetwork.com/journals/jama/… & pubmed.ncbi.nlm.nih.gov/23560283/) helped us in delivering blood products that recapitulate whole blood,
This is pivotal to prevent or correct the coagulopathy of trauma 👉🏾
This is pivotal to prevent or correct the coagulopathy of trauma 👉🏾
https://twitter.com/acweyand/status/1318530448599941120?s=20

🌟🅰️🅱️🆎🅾️Absolutely phenomenal #Blooducation lecture covering a range of topics from donor collection to #traumaresuscitation. If you missed it, don't worry! Just scan the HDR below. A million thank yous to @KreuterMD & @Pathologists for providing this learning opportunity! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh