Let's talk about placement of small bore nasoenteric feeding tubes and use of ultrasound for this (A thread)
Scenario: Pt with gastroparesis and COVID/ARDS, planning to prone, want post-pyloric tube. No dedicated team for this. Can we place safely w #POCUS guidance?
1/
Scenario: Pt with gastroparesis and COVID/ARDS, planning to prone, want post-pyloric tube. No dedicated team for this. Can we place safely w #POCUS guidance?
1/
How is small bore feeding tube (SBFT) different from standard NG?
Narrower (6-8 Fr vs 14-18 Fr), more flexible (but w rigid stylet for placement), longer. Thus: more comfortable, gastric or post-pyloric, ineffective for suction, prone to clogging, prone to PTX if placed in lung.
Narrower (6-8 Fr vs 14-18 Fr), more flexible (but w rigid stylet for placement), longer. Thus: more comfortable, gastric or post-pyloric, ineffective for suction, prone to clogging, prone to PTX if placed in lung.
Some methods used for placement
1) Blind placement - NOT RECOMMENDED. 1-2% risk of PTX
2) 2 radiograph method (safe but time consuming)
3) Capnometry
4) Endoscopic visualization
5) Electromagnetic
6) Fluoroscopic
7) Ultrasound?
Nice article on this: med.virginia.edu/ginutrition/wp…
3/
1) Blind placement - NOT RECOMMENDED. 1-2% risk of PTX
2) 2 radiograph method (safe but time consuming)
3) Capnometry
4) Endoscopic visualization
5) Electromagnetic
6) Fluoroscopic
7) Ultrasound?
Nice article on this: med.virginia.edu/ginutrition/wp…
3/
Let's talk about the methods that can be done safely with x-ray and #POCUS.
-the 2 radiograph method
-ultrasound confirmation (neck and subxyphoid)
Reminder before advancing tube into nose: remember to verify no history of recent ENT procedures!
4/
-the 2 radiograph method
-ultrasound confirmation (neck and subxyphoid)
Reminder before advancing tube into nose: remember to verify no history of recent ENT procedures!
4/
First the 2-radiograph method
1) Step 1: place to 30 cm
2) Step 2: CXR. If tube below carina, advance further. If in airway, remove and repeat.
This is a safe method, but time consuming
See below: initial placement in airway, requiring adjustment. Good thing for 30 cm CXR!
5/



1) Step 1: place to 30 cm
2) Step 2: CXR. If tube below carina, advance further. If in airway, remove and repeat.
This is a safe method, but time consuming
See below: initial placement in airway, requiring adjustment. Good thing for 30 cm CXR!
5/




What about #POCUS? First we will talk about the technique, then look at whether or not this can be done consistently/safely
6/
6/
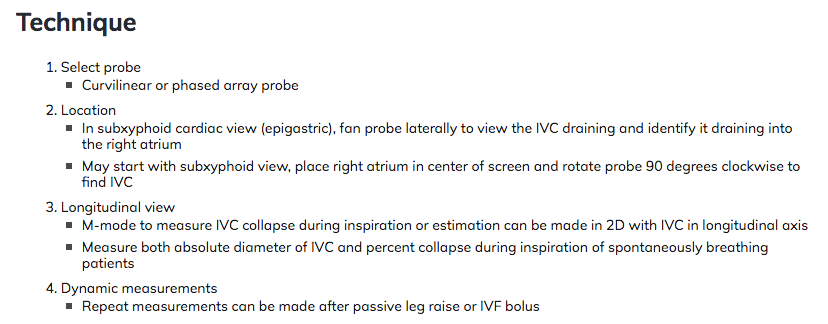
The technique (preferably 2 operator)
1) Place to 20-30 cm. Place linear probe transverse over midline neck and attempt to visualize bright tube in esophagus (lateral to trachea on either side). This is similar to (but opposite) ultrasound for endotracheal tube confirmation.
7/
1) Place to 20-30 cm. Place linear probe transverse over midline neck and attempt to visualize bright tube in esophagus (lateral to trachea on either side). This is similar to (but opposite) ultrasound for endotracheal tube confirmation.
7/

The technique (continued)
2) Confirm in long axis.
8/
2) Confirm in long axis.
8/
The technique (continued)
2) Ideally move the tube and verify that the bright structure moves, and is in fact the feeding tube.
9/
2) Ideally move the tube and verify that the bright structure moves, and is in fact the feeding tube.
9/
The technique (continued)
3) Confirm again that this is in the esophagus (not trachea) by return to short axis.
(This is somewhat similar in idea to wire confirmation in CVC placement)
10/
3) Confirm again that this is in the esophagus (not trachea) by return to short axis.
(This is somewhat similar in idea to wire confirmation in CVC placement)
10/

The technique (continued)
4) Pause. This is the key step in safety.
If the tube is in the trachea and is advanced further, PTX may occur. If there is any doubt whatsoever, obtain CXR. In theory, if esophageal placement definitively confirmed, tube can be advanced.
11/
4) Pause. This is the key step in safety.
If the tube is in the trachea and is advanced further, PTX may occur. If there is any doubt whatsoever, obtain CXR. In theory, if esophageal placement definitively confirmed, tube can be advanced.
11/
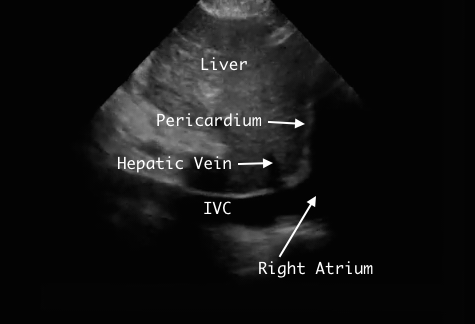
The technique (continued)
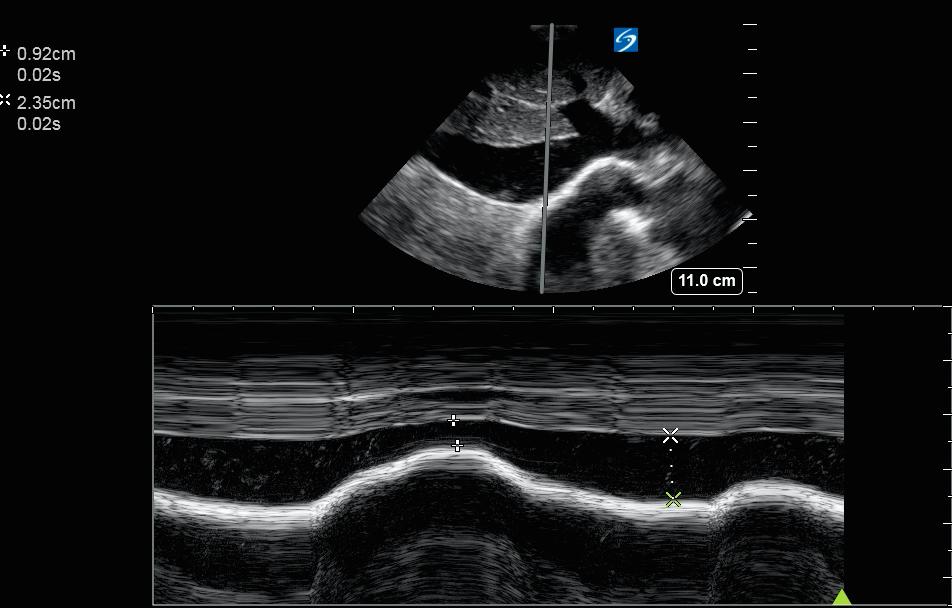
5) Advance into stomach/post pyloric. Can attempt to visualize in stomach/duodenum with ultrasound using phased array or curvilear probe placed over epigastrium.
12/
5) Advance into stomach/post pyloric. Can attempt to visualize in stomach/duodenum with ultrasound using phased array or curvilear probe placed over epigastrium.
12/
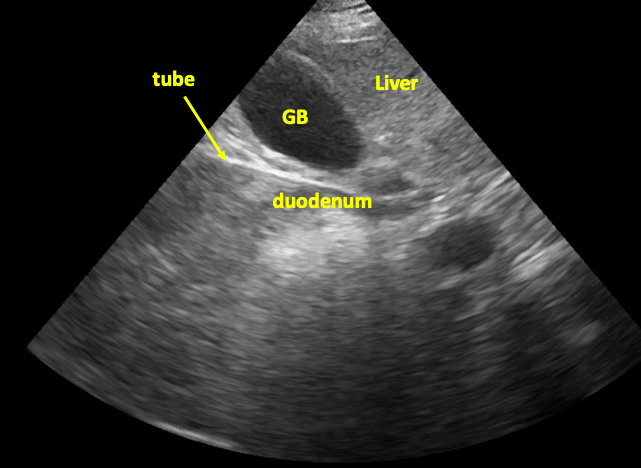
Tube in stomach/duodenum in short axis
13/
13/
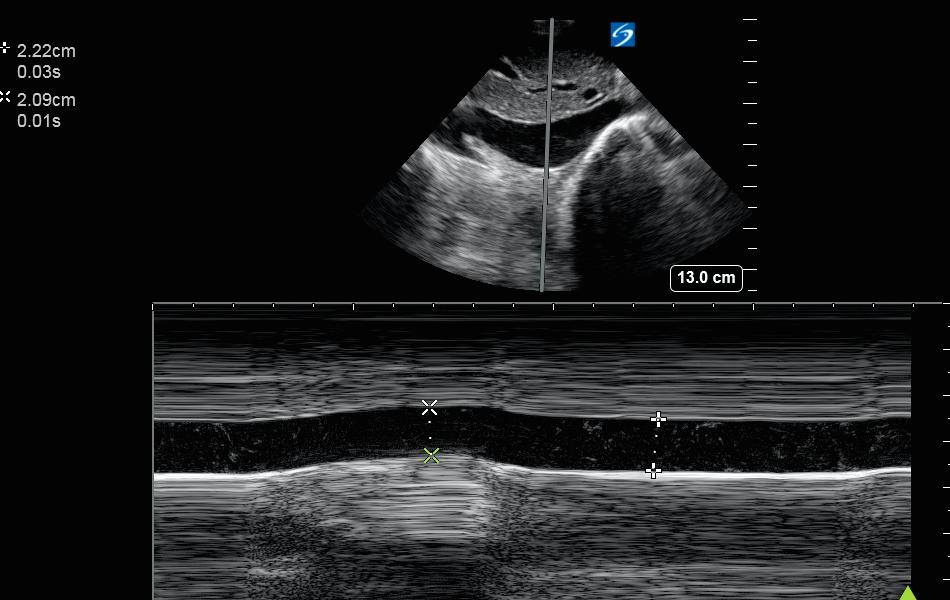
The technique (continued)
If a separate NG is in place already, can suction out all air and fill with 60-180 cc fluid to optimize acoustic window.
In this image, tube in seen in duodenum in long axis.
14/

If a separate NG is in place already, can suction out all air and fill with 60-180 cc fluid to optimize acoustic window.
In this image, tube in seen in duodenum in long axis.
14/

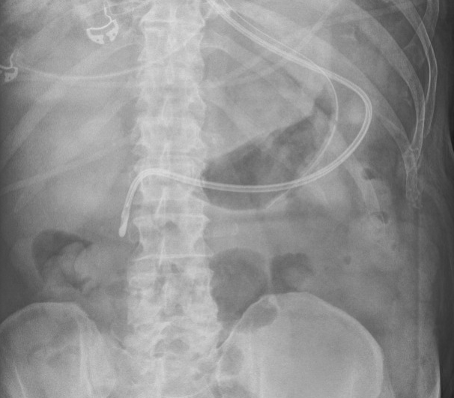
The Technique (continued)
6) Obtain abdominal xray to verify placement (and perhaps CXR as well to exclude PTX)
(Here we see tip of tube in second portion of duodenum)
7) Remove stylet, ok to use
15/
6) Obtain abdominal xray to verify placement (and perhaps CXR as well to exclude PTX)
(Here we see tip of tube in second portion of duodenum)
7) Remove stylet, ok to use
15/
So we see that this method can be done. But there are still many questions
1) How reliable/safe is this?
2) How often can the views be obtained (esophageal or gastric/duodenal)
3) Is this worth the time/effort, compared to other methods?
16/
1) How reliable/safe is this?
2) How often can the views be obtained (esophageal or gastric/duodenal)
3) Is this worth the time/effort, compared to other methods?
16/
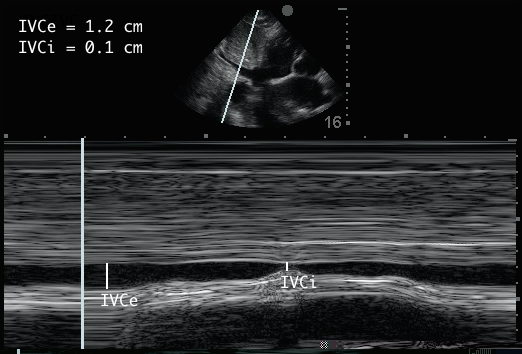
Study by Gok et al, 56 patients underwent tube placement, with esophageal visualization in 52 (94%) and no complications. When esophageal visualization not seen, 1/4 (25%) had tracheal placement. In 3/4 cases, tube was not seen for unclear reasons. onlinelibrary.wiley.com/doi/abs/10.117…
17/
17/
In a study by Nedel et al, 41 pts were evaluated for tube placement by ultrasound.
Sens 97%, NPV: 66% (if not seen in correct position, could still be correct or misplaced)
Spec and PPV: 100% (if seen to be in correct position, was always correct)
jintensivecare.biomedcentral.com/articles/10.11…
18/

Sens 97%, NPV: 66% (if not seen in correct position, could still be correct or misplaced)
Spec and PPV: 100% (if seen to be in correct position, was always correct)
jintensivecare.biomedcentral.com/articles/10.11…
18/


In a study by Yıldırım et al, combined neck and subxyphoid ultrasound yielded good sensitivity (>90%) and 100% specificity (and PPV) for placement.
hindawi.com/journals/emi/2…
19/
hindawi.com/journals/emi/2…
19/

In summary of these data, it seems that if the tube is definitively seen in the esophagus, it is 100% likely to be in the esophagus and can be advanced. If it is not seen, it may or may not be in the esophagus, and a CXR should be obtained before advancing a small bore tube.
20/
20/
Some closing points
-risk of PTX w small bore feeding tube placement is real. If any doubt, get CXR at 30-35 cm
-POCUS can guide placement
-still get abd xray before using in most cases
-a dedicated team is ideal, but if unfeasible, US guided placement may help
21/
-risk of PTX w small bore feeding tube placement is real. If any doubt, get CXR at 30-35 cm
-POCUS can guide placement
-still get abd xray before using in most cases
-a dedicated team is ideal, but if unfeasible, US guided placement may help
21/
What do others think about the use of ultrasound for placement of small bore feeding tube?
Who has done this? What have been your experiences?
@TimRowesays @ArgaizR @Cometin007 @agraviersymmes @NephroP @DRsonosRD @laxswamy
@DrGalenMD @cameron_baston @MedEdPGH @hraza222
22/
Who has done this? What have been your experiences?
@TimRowesays @ArgaizR @Cometin007 @agraviersymmes @NephroP @DRsonosRD @laxswamy
@DrGalenMD @cameron_baston @MedEdPGH @hraza222
22/
@kyliebaker888 @RogerAlvarezDO @MikeRoseMDMPH @cianmcdermott @easypocus @Wilkinsonjonny @load_dependent @iceman_ex @JCHCheung @jtanguay11
@ScottTiltonCRNP @ubcimpocus @JRH_MD @fluidloading @drshahrul80 @jminardi21 @jelevenson @SonoInternist @unicipa @khldtaha @FMsono
@ScottTiltonCRNP @ubcimpocus @JRH_MD @fluidloading @drshahrul80 @jminardi21 @jelevenson @SonoInternist @unicipa @khldtaha @FMsono
@bryanboling @virenkaul @pedrodammert @criticalcareuk
@redneeraj @ccpractitioner @BrunoAlvCon @antonyashton @drpaulinosegun1 @wandering_er @interconsulta @UltrasoundHub @MedTweetorials @ThinkingCC @VirtueOfNothing @siddharth_dugar @msenussiMD @POCUS_Society @POCUSAcademy
@redneeraj @ccpractitioner @BrunoAlvCon @antonyashton @drpaulinosegun1 @wandering_er @interconsulta @UltrasoundHub @MedTweetorials @ThinkingCC @VirtueOfNothing @siddharth_dugar @msenussiMD @POCUS_Society @POCUSAcademy
.
It has become important to add a bit more description on 1) what exactly is a SBFT?
2) what does this mean for the lungs?
3) how high really is the PTX risk?
Would like to emphasize: standard NG placed blindly, minimal PTX risk. But SBFT placed blindly does have PTX risk.
23/
2) what does this mean for the lungs?
3) how high really is the PTX risk?
Would like to emphasize: standard NG placed blindly, minimal PTX risk. But SBFT placed blindly does have PTX risk.
23/
small bore feeding tube - some names include dobhoff, duotube, corpak, and probably others. (i.e. Dobhoff is a type of SBFT)
SBFT: 6-10 Fr = 2-3 mm outer diameter (OD)
Standard NG: 14-18 Fr = 5-6 mm OD
Peds bronchoscope (Q190): 4.8 mm OD
Therapeutic scope (TH190): 6 mm OD
24/
SBFT: 6-10 Fr = 2-3 mm outer diameter (OD)
Standard NG: 14-18 Fr = 5-6 mm OD
Peds bronchoscope (Q190): 4.8 mm OD
Therapeutic scope (TH190): 6 mm OD
24/
What does this mean for the lung?
The standard NG will not pass the main bronchi (not quite as far as a peds bronchoscope)
The SBFT will reach terminal bronchioles. It can be believed that this would increase PTX risk.
See Weibel diagram: from epj-conferences.org/articles/epjco…
25/

The standard NG will not pass the main bronchi (not quite as far as a peds bronchoscope)
The SBFT will reach terminal bronchioles. It can be believed that this would increase PTX risk.
See Weibel diagram: from epj-conferences.org/articles/epjco…
25/


But is the risk of PTX real for SBFT?
According to this study: 3.2% likelihood of respiratory tree placement, with 1.2% risk of PTX pubmed.ncbi.nlm.nih.gov/17595433/
Others show lower risks (but still appreciable, in the 0.3-1.0% range), as described in med.virginia.edu/ginutrition/wp…
26/
According to this study: 3.2% likelihood of respiratory tree placement, with 1.2% risk of PTX pubmed.ncbi.nlm.nih.gov/17595433/
Others show lower risks (but still appreciable, in the 0.3-1.0% range), as described in med.virginia.edu/ginutrition/wp…
26/
Pulling this reply with Cochrane review to main thread
https://twitter.com/drhazemlashin/status/1328132860868485122?s=20
Thanks all for the discussion. Ultimately, this is probably not the highest yield POCUS application, but an interesting one to consider, and may be time-saving compared to the 2-radiograph method, if that is the alternative.
• • •
Missing some Tweet in this thread? You can try to
force a refresh