Prior dx of kidney stones on CT (6-8 mm, unknown type), managed medically. Has intermittent L flank pain. Last 2 days - f/c/n/v/back pain.
T 38.6 HR 98 BP 154/88 SpO2 99%
UA: 1+ blood, 3+ LE, WBC TNTC
+L CVA and suprapubic tenderness
WBC 18
Cr 1.6 (baseline 1.3)
2/
How specifically could POCUS help here? What POCUS question(s) exactly?
3/
It is 8PM. What would be your approach to imaging (if POCUS unavailable)
(we will assume radiology staff not in house overnight, but could be called in)
4/
@SonoInternist @DRsonosRD @trobertson8 @G2Disrupt @IM_POCUS @buckeye_sanjay @benjikmathews @POCUS_Society @kyliebaker888 @CaseMcQuade @MedEdPGH @HeyDrNik @kkalra_22
1) Is the exam literature-based as a point-of-care study
2) How would each possible finding change mgmt
5/
7/
8/
9/
10/
11/
12/
13/
14/
15/
How does this affect management (in the practical setting)?
What role does POCUS play in the case?
Limitations? Feedback on how to improve image quality?
16/
18/
19/
1) When to obtain imaging in a pt with acute pyelo?
2) How do we grade hydronephrosis on POCUS?
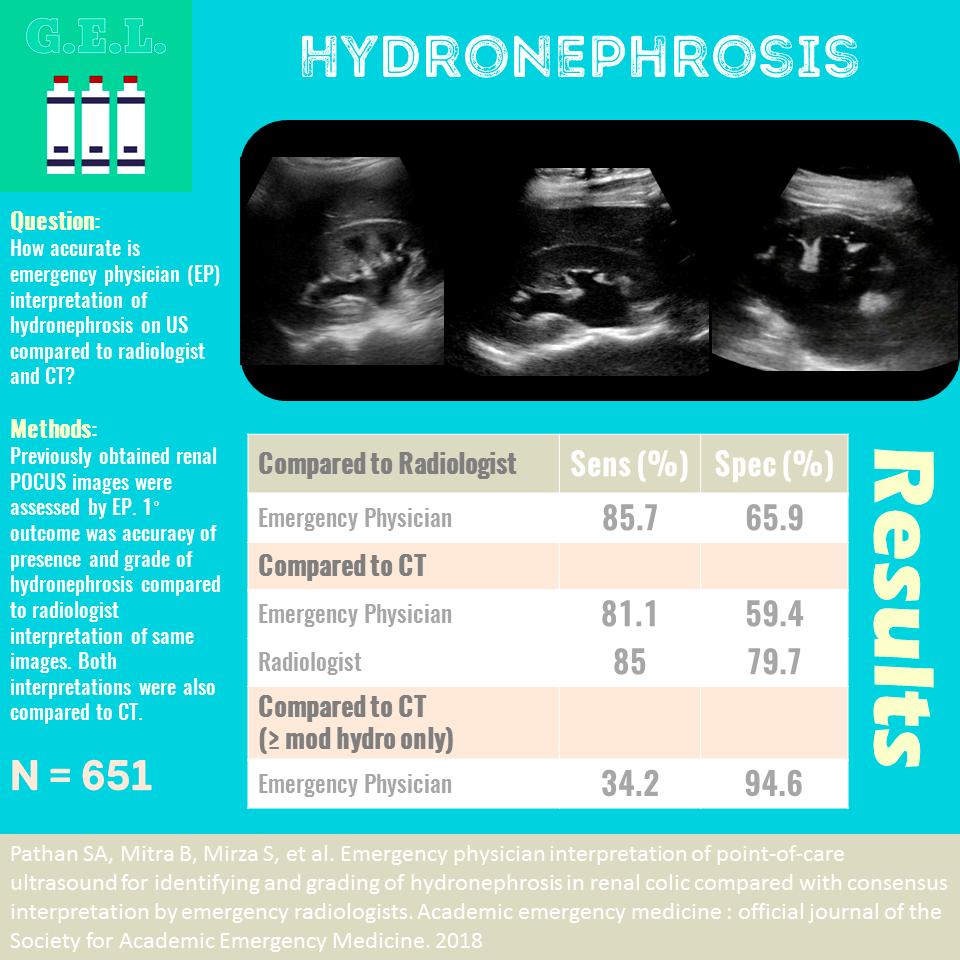
3) How sens and spec is POCUS for hydronephrosis?
4) Is POCUS useful to r/o stone?
5) How do we integrate POCUS findings to affect dx in mgmt in this case?
20/
POCUS for hydronephrosis performed by IM residents had sens of >90% and spec of > 90% (ncbi.nlm.nih.gov/pubmed/24154905). Another study in the ED found sens 86% for any hydronephrosis and 66% spec (95% spec for moderate or greater hydronephrosis) - see image from ultrasound GEL
23/
24/
- Remember to be clear on what exactly you are asking on POCUS, and how possible findings will impact your approach in the practical setting
-In this case presence or absence of hydronephrosis was most critical, and guided urgency of imaging and mgmt
26/
27/