Happy Monday everyone! We have a special case for you today written by UPMC PGY2 #POCUS enthusiast @MikeTao15.
A 52 yo M with hx of EtOH/HCV cirrhosis, VTE on Eliquis, HFrEF presents w worsening abd distention and pain. He is disoriented and unable to give much history.
Cirrhosis previously complicated by esophageal varices, hepatic encephalopathy, and ascites. No follow up since last hospital admission at outside facility ~1 year ago. Has not been taking meds.
Vitals in the ED: Temp 38.1, HR 90, BP 98/70, Pulse Ox 96% on 2L
He is lethargic, arousable to voice and oriented to self only
+scleral icterus
Cardiac + pulmonary exams normal
Abdomen distended, diffusely tender, no rebound/guarding
2+ b/l edema to thighs
Jaundiced, scattered ecchymoses
+asterixis
Labs (unkown baseline):
Na 129, Cr 2.2, Alb 2.8, Tbili 3.2, AST/ALT 140/160, ALP 310
WBC 2.1, Hb 7.4, Plt 80, INR 2.5
Blood cultures are collected. You go find your #POCUS and prepare for a diagnostic paracentesis.
Some polls while we're looking for our ultrasound machines.
How concerned are you for SBP in this patient? (poll)
Would you start empiric abx at this point? (poll)
What would you do with volume? (poll)
Now for our images!
RUQ
RUQ zoomed in
RUQ zoomed in further
Left upper quadrant
Subcostal. Do not have an IVC view available unfortunately
Suprapubic
How would you characterize this patients ascitic fluid? (poll)
How concerned are you for SBP or secondary peritonitis? (poll)
What would you do with volume? (poll)
What is your overall interpretation and next steps?
Pulling in our experts!
@TimRowesays @ArgaizR @Cometin007 @rogeralver @agraviersymmes @NephroP @DRsonosRD @laxswamy @DrGalenMD @cameron_baston @kyliebaker888 @RogerAlvarezDO @MikeRoseMDMPH @cianmcdermott @easypocus
Alright, all. Time to wrap up!
#POCUS interpretation:
Diffuse complex free intraabdominal fluid in the right + left upper quadrants + pericolic gutter with visible fibrin stranding, plankton sign, and hematocrit sign
Simple right renal cyst, no hydronephrosis
The bladder is decompressed with Foley catheter seen
Tachycardia with regular rhythm is noted on subxiphoid view without any significant pericardial effusion. LV and RV function is difficult to assess based on these images, but grossly appears preserved
The patient was had progressive tachycardia to the 120s - 130s. Repeat CBC w downtrending Hgb to 6.2. Mental status worsened, transferred to the ICU and intubated for airway protection. He was resuscitated with pRBCs, plts, and FFP. General surgery consulted.
Pt went to OR for ex lap and bloody ascitic fluid was found but no source of bleeding identified. Bleeding resolved with resuscitation and after a prolonged hospital course pt eventually recovered and was discharged.
Final Diagnosis: Hemoperitoneum, etiology unclear.
Thought-Provoking Questions from this case:
1) What are features on POCUS that would distinguish complex vs simple ascitic fluid?
2) What are ultrasonographic findings of complex fluid? Is there literature behind this?
3) What was the role of POCUS in this case?
1) Simple vx. complex ascitic fluid
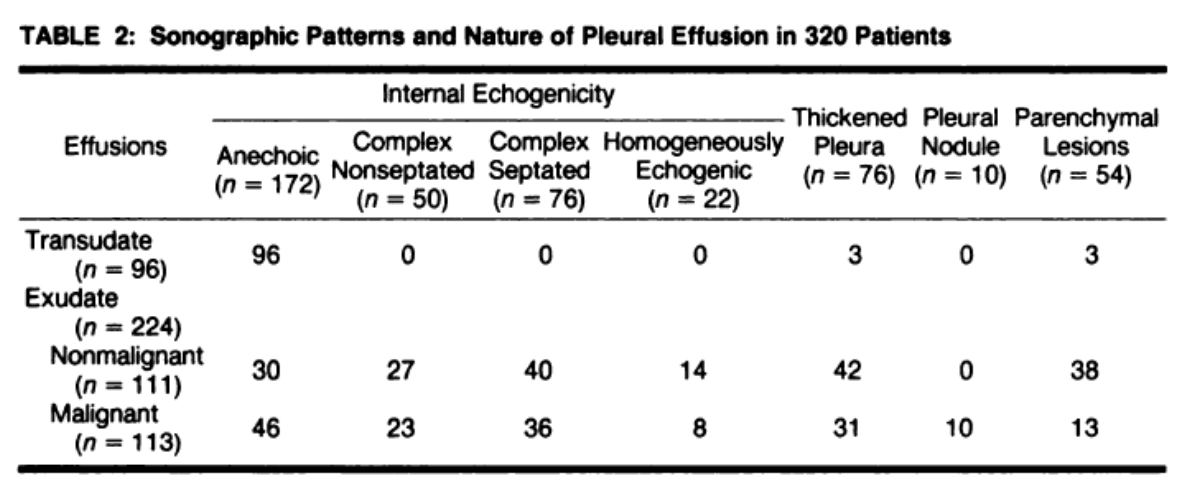
Broadly, ascitic fluid can be characterized as transudative - typically homogenously anechoic - or exudative - can be anechoic or complex. Complex fluid may present with debris, internal septations, and loculated collections.
To our knowledge, most studies on complex vs simple fluid, like @cameron_baston said, are older and on pleural fluid, such as ajronline.org/doi/pdf/10.221…, + conclude that complex effusions are almost always exudates whereas simple effusions can be transudate OR exudate.
An article by Rudralingam et al - ncbi.nlm.nih.gov/pmc/articles/P… - presents a nice case series describing different types of ascites and comes to a similar conclusion - complex fluid may be useful to help rule IN an exudative process.
2) So, what are the #POCUS findings of complex fluid?
The “plankton sign” and “hematocrit sign” are two sonographic findings that have been reported.
Plankton sign reveals echogenic cellular debris that swirl as a result of respiratory motion and vascular pulsations.
3) So how did #POCUS help in this case?
Without much data to support this beyond what we have described above (please post studies or thoughts if you have them!), we think of complex fluid as useful for ruling IN a more complex process
That is, the presence of hematocrit sign, septations, or fibrin stranding significantly increases our suspicion for an alternate process like SBP or hemoperitoneum, but the absence of these signs wouldn’t rule this out, as we all know how tricky it can be to diagnose SBP.
Thanks all for your wise thoughts and insights as always!
Pulling back in our participants.
@cameron_baston @TimRowesays @ThinkingCC @ssrasm
@NephroP @jtanguay11 @jminardi21 @ScottBiggersta1 @buckeye_sanjay
Please pull in anyone we missed.
Happy #POCUS-ing













