1/ #BreastRadPath with @DrJordanaP
For this tweetorial we are going to talk about how we evaluate the biomarkers ER, PR, and HER2.
@BIDMCpath @BIDMC_BreastImg @CollinsLauraC @ADamronMD @GuzmanArocho @XeniaParisi @MarcosLepeMD @DrGeeONE @smlungpathguy
For this tweetorial we are going to talk about how we evaluate the biomarkers ER, PR, and HER2.
@BIDMCpath @BIDMC_BreastImg @CollinsLauraC @ADamronMD @GuzmanArocho @XeniaParisi @MarcosLepeMD @DrGeeONE @smlungpathguy

2/ The biomarkers provide predictive information (how a patient may respond to targeted therapy) as well as prognostic information. It helps to organize patients into treatment groups that follow different algorithms and guidelines.
3/ Biomarkers are evaluated in routine clinical mgmt of patients with breast cancer. The 3 routinely tested:
Hormone receptors (HR): Estrogen receptor (ER) and Progesterone receptor (PR)
&
Human epidermal growth factor receptor 2 (HER2)
(chart from: bit.ly/3lPbqoY)
Hormone receptors (HR): Estrogen receptor (ER) and Progesterone receptor (PR)
&
Human epidermal growth factor receptor 2 (HER2)
(chart from: bit.ly/3lPbqoY)

4/ We use the testing guidelines from the American Society for Clinical Oncology (ASCO) and the College of American Pathologists (CAP). They include technical information about how the tissue should be handled. 👇
5/ ER and PR: Most recent guidelines published in 2020 (updated from 2010) bit.ly/36Xpo3s
HER2: Most recent guidelines published in 2018 (first released in 2007 and updated in 2013) bit.ly/36XLqTV

HER2: Most recent guidelines published in 2018 (first released in 2007 and updated in 2013) bit.ly/36XLqTV


6/ We use immunohistochemistry (IHC) to determine ER and PR status by staining ER/PR receptors in the nuclei. Guidelines require that IHC reports include: % of tumor cells with nuclear staining, intensity of staining (weak, moderate, strong), & interpretation (pos vs neg).
7/ ER & PR result categories:
Positive: ≥1% of tumor nuclei staining
Negative: <1% of tumor nuclei staining
For ER, there is a “low positive category” --> 1-10% of nuclei staining
Positive: ≥1% of tumor nuclei staining
Negative: <1% of tumor nuclei staining
For ER, there is a “low positive category” --> 1-10% of nuclei staining
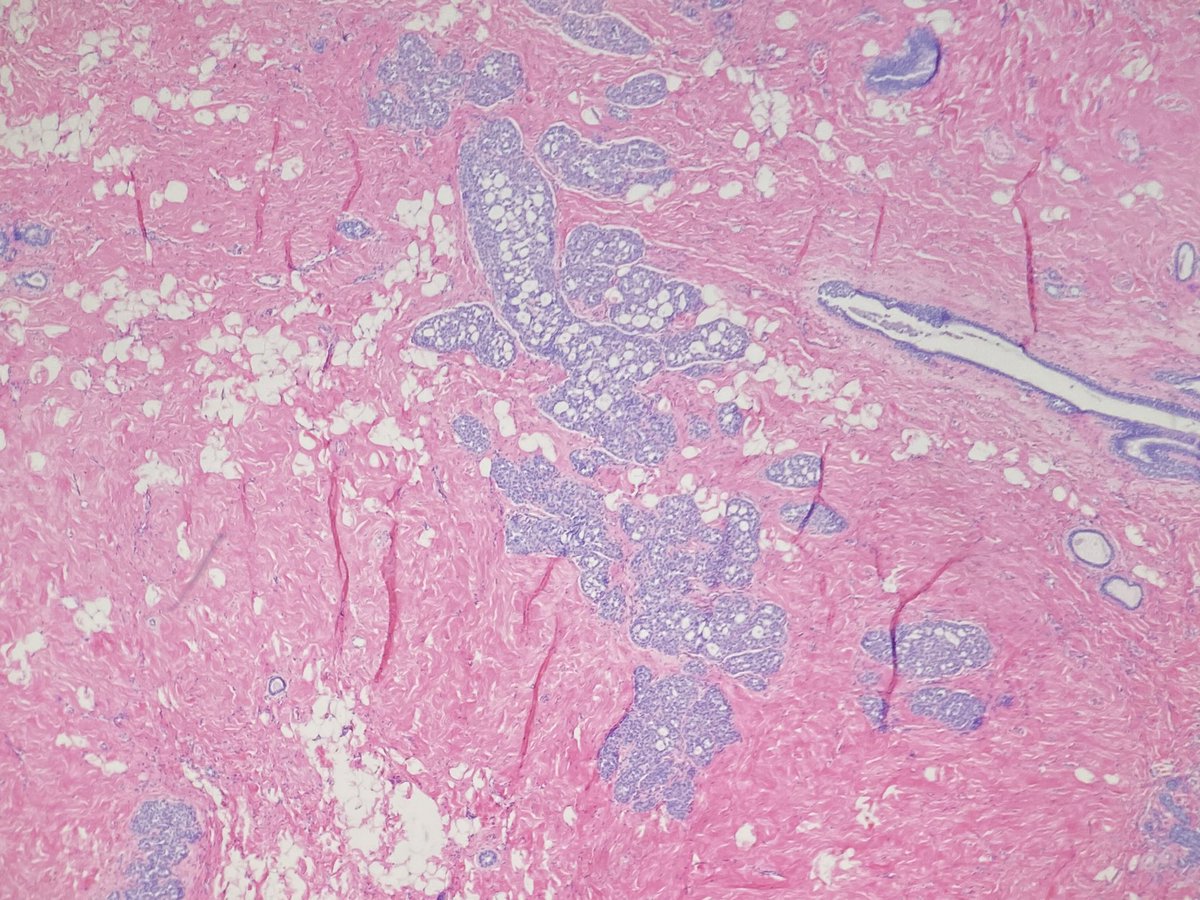
8/ For example, this case of an invasive lobular carcinoma (H&E stain on left) is: ER positive, >95% of nuclei are staining with strong intensity (the brown dots on the right). (PR positive would look similar). 

10/ HER2 can be evaluated by different methods. HER2 protein overexpression is assessed by IHC. HER2 gene amplification is assessed by in situ hybridization (ISH). There are different types of ISH, we do FISH (fluorescent ISH).
11/ For evaluation by IHC we evaluate the cell membrane staining to look for HER2 protein expression. 

12/ Here is an example of a HER2 positive invasive ductal carcinoma showing 3+ membrane staining. To me, in positive cases, it looks like someone took a sharpie and drew around each cell. 

13/ For HER2 gene amplification the gene copies of HER2 (on chromosome 17) are compared to CEP17 (centromeric region of chromosome 17). See the flow chart from the guidelines to see how we interpret the results. 

14/ Here is an example of a breast cancer with amplified (FISH positive) HER2 --> each cell (blue circle) has many more red dots than green dots. 

15/ Many institutions start with IHC and only send the 2+ equivocal cases for FISH to classify HER2. Most of the cases will fall into FISH positive (group 1) or negative (group 5). We send both IHC and FISH on all of our cases of invasive breast cancer.
16/ Cases that fall into the non-classical FISH groups (groups 2, 3 and 4) we use IHC result and the group number to help classify. It is a bit complicated so see table below 👇 

17/ These are the three routine biomarkers we do on every case of invasive carcinoma. We perform these studies on the core needle biopsy and sometimes on the excision. We also perform them in cases of metastatic breast carcinoma so it can help guide treatment.
18/ There are pitfalls and other considerations, but we can address those in a future post!
• • •
Missing some Tweet in this thread? You can try to
force a refresh